Guide to IBS And Other Gi Disorders
Explore the differences between IBS and other gastrointestinal (GI) disorders. Learn about symptoms, causes, and treatment options to better manage digestive health and improve your quality of life.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

That nagging cramp after a meal, the unpredictable bloating, the urgent rush to the restroom—if this sounds familiar, you might be among the millions navigating life with Irritable Bowel Syndrome (IBS) or another gastrointestinal disorder. These conditions are far more than just occasional indigestion; they are complex, often chronic issues that can significantly impact your quality of life. But you are not alone, and more importantly, you are not without options. This guide is designed to demystify IBS and other GI disorders, moving beyond the confusion to provide clear, actionable information. We will break down the symptoms, explore the underlying causes, differentiate between common conditions, and provide a roadmap for effective management and treatment. Our goal is to empower you with knowledge, so you can take proactive steps toward calming your gut and reclaiming your comfort.
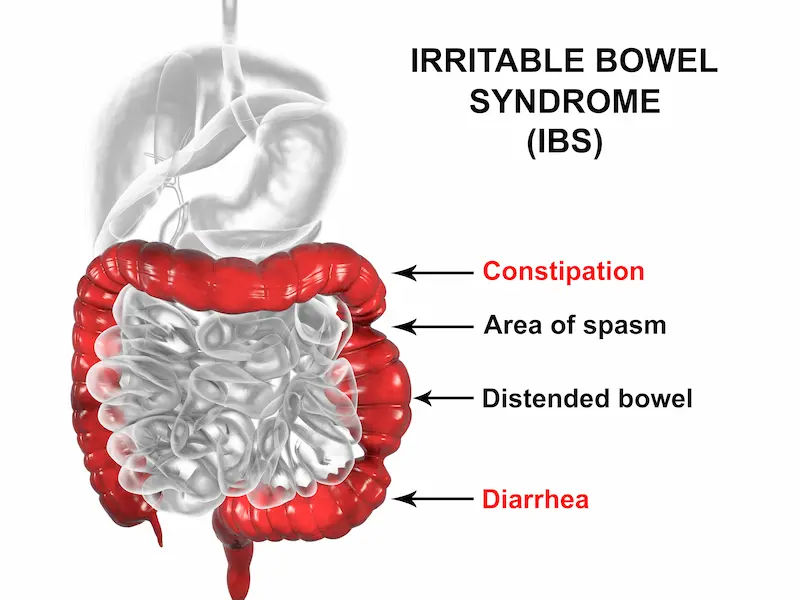
What Exactly is Irritable Bowel Syndrome (IBS)?
Irritable Bowel Syndrome (IBS) is a common disorder that affects the large intestine (colon). It's characterised by a group of symptoms that typically occur together, including recurrent abdominal pain and changes in bowel habits—such as diarrhoea, constipation, or both. Unlike more serious diseases like Crohn's or ulcerative colitis, IBS does not cause inflammation, permanent damage to the digestive tract, or increase your risk of colorectal cancer. It is a chronic condition that requires long-term management, though symptoms often fluctuate and can be well-controlled with the right strategies.
IBS as a Functional GI Disorder
IBS is classified as a functional gastrointestinal disorder. This means that while symptoms are very real, they occur due to a problem with how the gut and brain work together—a "glitch" in communication often called gut-brain axis dysfunction. Imagine the nerves in your digestive system being overly sensitive, causing them to overreact to normal digestive processes like the passage of food and gas. This leads to the pain and discomfort characteristic of IBS. There's no structural damage visible on standard tests, which is why diagnosis can be challenging.
How Common is IBS?
IBS is incredibly prevalent, affecting an estimated 10-15% of the global population. It's the most common disease diagnosed by gastroenterologists and a frequent reason for primary care visits. It's twice as common in women as in men, and it often begins before the age of 50. Despite its prevalence, many people suffer in silence due to embarrassment, making awareness and education crucial.
Recognising the Signs: Symptoms of IBS
The symptoms of IBS can vary widely from person to person and often resemble those of other diseases. The most common signs include:
- Abdominal pain or cramping, usually relieved by having a bowel movement.
- Bloating and a feeling of gas.
- Changes in bowel habits: Diarrhoea (IBS-D), constipation (IBS-C), or alternating between the two (IBS-M).
- Changes in the appearance of stool (e.g., lumpy/hard or loose/watery).
- Mucus in the stool.
A feeling that a bowel movement was incomplete (tenesmus).
It's important to note "red flag" symptoms that are NOT typical of IBS and warrant immediate medical attention: unexplained weight loss, rectal bleeding, fever, persistent pain that isn't relieved by passing gas or a bowel movement, and symptoms that wake you from sleep.
The Four Types of IBS
To guide treatment, doctors often categorise IBS into four main subtypes based on your predominant bowel habit:
1. IBS with constipation (IBS-C): Hard or lumpy stools ≥25% of the time and loose/watery stools <25%.
2. IBS with diarrhoea (IBS-D): Loose/watery stools ≥25% of the time and hard/lumpy stools <25%.
3. IBS with mixed bowel habits (IBS-M): Both hard/lumpy and loose/watery stools on >25% of bowel movement days.
4. IBS unclassified (IBS-U): Insufficient abnormality in stool consistency to meet the criteria for IBS-C, D, or M.
Other Common Gastrointestinal Disorders
While IBS is a functional disorder, other GI conditions involve structural or inflammatory changes. It's vital to distinguish between them.
- Inflammatory Bowel Disease (IBD): Crohn's & Ulcerative Colitis
- IBD is not the same as IBS. Inflammatory Bowel Disease is an umbrella term for conditions involving chronic inflammation of the digestive tract, which can lead to severe complications.
- Crohn's Disease: Can affect any part of the GI tract, from mouth to anus, with inflammation that extends deep into the tissue layers.
- Ulcerative Colitis: Involves continuous inflammation and ulcers only in the large intestine's innermost lining.
- Key Difference: IBD causes visible inflammation and damage seen during colonoscopy or imaging, while IBS does not.
Consult Top Specialists
Gastroesophageal Reflux Disease (GERD)
GERD occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (oesophagus). This backwash (acid reflux) can irritate the oesophageal lining. While a separate condition, it's not uncommon for individuals with IBS to also experience GERD symptoms like heartburn and regurgitation.
Celiac Disease
Celiac disease is an immune reaction to eating gluten, a protein found in wheat, barley, and rye. Over time, this reaction damages the small intestine's lining, preventing nutrient absorption. While it shares symptoms like diarrhoea and abdominal pain with IBS-D, it is a distinct autoimmune disorder that requires a strict gluten-free diet.
What Causes IBS?
The exact cause of IBS is unknown, but several factors are believed to play a role synergistically.
The Gut-Brain Axis Connection
This is a critical concept. The gut and brain are in constant communication via nerves, hormones, and signals from gut microbes. In IBS, this axis is disrupted. The brain may misinterpret normal digestive signals as painful (visceral hypersensitivity), or stress signals from the brain can slow down or speed up digestive processes, leading to symptoms.
Food Sensitivities and FODMAPs
For many, symptoms are triggered by specific foods. While not true allergies, these are intolerances. A major breakthrough in understanding how to relieve IBS pain has been the identification of FODMAPs—Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are short-chain carbohydrates that are poorly absorbed in the small intestine, ferment in the colon, and draw water into the bowel, causing gas, bloating, pain, and altered motility.
The Role of Stress and Mental Health
Can stress cause irritable bowel syndrome? While it doesn't cause it, it is a potent trigger. High stress levels can exacerbate symptoms significantly. Many people with IBS also have conditions like anxiety and depression, further highlighting the brain-gut link.
How is IBS Diagnosed?
There is no single test for IBS. Diagnosis is primarily based on your symptoms and medical history, following a process of exclusion to rule out other conditions.
The Rome IV Criteria
Doctors use the Rome IV criteria, a standardized tool for diagnosing functional GI disorders. For an IBS diagnosis, you must have recurrent abdominal pain at least one day per week in the last three months, associated with two or more of the following: related to defecation, associated with a change in frequency of stool, or associated with a change in the form (appearance) of stool.
Tests to Rule Out Other Conditions
To ensure your symptoms aren't from something else, your doctor may order tests. If your condition does not improve after trying initial management methods, consult a doctor online with Apollo24|7 for further evaluation. They may recommend:
- Blood tests: To check for anaemia, infection, or celiac disease.
- Stool tests: To look for infection, inflammation, or blood.
- Hydrogen breath test: To test for small intestinal bacterial overgrowth (SIBO) or lactose intolerance.
- Colonoscopy/Gastroscopy: To visually examine your colon and rule out IBD, celiac disease, or cancer. Apollo24|7 offers convenient home collection for tests like basic blood panels that can be a first step in this diagnostic process.
Effective Management and Treatment Strategies for IBS
Managing IBS is highly individual. A multi-faceted approach combining diet, lifestyle, and sometimes medication is most effective.
Dietary Changes: The Low FODMAP Approach
The low FODMAP diet for beginners is a three-phase elimination diet proven to reduce symptoms in about 70% of people with IBS. It's not a lifelong diet but a diagnostic tool to identify your personal triggers. It should be undertaken with guidance from a registered dietitian.
1. Elimination: Strictly avoid high-FODMAP foods for 2-6 weeks.
2. Reintroduction: Systematically challenge food groups to identify triggers.
3. Personalisation: Reintegrate tolerated foods to create a sustainable, long-term diet.
Lifestyle Modifications: Stress Reduction and Exercise
Regular physical activity helps reduce stress and stimulates normal contractions of your intestines. Stress management techniques are non-negotiable. Practices like yoga, meditation, cognitive-behavioural therapy (CBT), and even simple deep-breathing exercises can significantly calm the gut-brain axis and reduce symptom severity.
Medications for Symptom Relief
Various medications can target specific symptoms:
- Fibre supplements (e.g., psyllium) for IBS-C.
- Laxatives (e.g., polyethylene glycol) for constipation.
- Anti-diarrheal medications (e.g., loperamide) for IBS-D.
- Antispasmodics (e.g., hyoscine) to reduce colon spasms and pain.
- Low-dose antidepressants: Used for their neuromodulatory effects on the gut-brain axis, not for depression.
The Promise of Probiotics and Gut Health
Certain probiotics for IBS, particularly strains of Bifidobacterium and Lactobacillus, may help restore a healthy balance of gut bacteria, alleviate bloating and gas, and regulate bowel movements. Results vary, so it may take trying a few different products to find one that works for you.
When to See a Doctor?
It's crucial to seek professional medical advice for a proper diagnosis, especially if you experience any "red flag" symptoms like unexplained weight loss, rectal bleeding, fever, or persistent pain. If symptoms persist beyond two weeks and disrupt your daily life, consult a doctor online with Apollo24|7 to discuss your symptoms and begin the diagnostic process. Self-diagnosing and treating can lead to missing a more serious condition.
Conclusion
Living with Irritable Bowel Syndrome can be a frustrating and isolating journey, but it's important to remember that it is a manageable condition. By understanding the triggers, embracing a personalised approach to diet and lifestyle, and working closely with healthcare professionals, you can significantly reduce the impact of symptoms and regain control. This guide to IBS and other GI disorders is your starting point. Listen to your body, be patient with the process of identifying your unique triggers, and don't hesitate to seek support. If your symptoms feel overwhelming, take the next step today. Book a physical visit to a doctor with Apollo24|7 to create a tailored management plan that works for you. A calmer, more comfortable life is within reach.
Consult Top Specialists
Consult Top Specialists

Dr Bhargav Vuppumalla
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD GENERAL MEDICINE
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr Harish K C
Gastroenterology/gi Medicine Specialist
15 Years • MBBS MD DM MRCP(UK) (SCE-Gastroenterology and Hepatology)
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru

Dr Rohit Sureka
Gastroenterology/gi Medicine Specialist
15 Years • MBBS, DNB General Medicine, DNB Gastroenterology
Jaipur
Apollo 247 virtual - Rajasthan, Jaipur

Dr. Shivaraj Afzalpurkar
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD General medicine (Gold medalist), DrNB (Gastroenterology), MNAMS
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Amit Pandita
Gastroenterology/gi Medicine Specialist
10 Years • MBBS. MD (INTERNAL MEDICINE) DrNB (GASTROENTEROLOGY AND HEPATOLOGY)
Delhi
Apollo Hospitals Indraprastha, Delhi
Consult Top Specialists

Dr Bhargav Vuppumalla
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD GENERAL MEDICINE
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr Harish K C
Gastroenterology/gi Medicine Specialist
15 Years • MBBS MD DM MRCP(UK) (SCE-Gastroenterology and Hepatology)
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru

Dr Rohit Sureka
Gastroenterology/gi Medicine Specialist
15 Years • MBBS, DNB General Medicine, DNB Gastroenterology
Jaipur
Apollo 247 virtual - Rajasthan, Jaipur

Dr. Shivaraj Afzalpurkar
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD General medicine (Gold medalist), DrNB (Gastroenterology), MNAMS
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Amit Pandita
Gastroenterology/gi Medicine Specialist
10 Years • MBBS. MD (INTERNAL MEDICINE) DrNB (GASTROENTEROLOGY AND HEPATOLOGY)
Delhi
Apollo Hospitals Indraprastha, Delhi
More articles from Irritable Bowel Syndrome
Frequently Asked Questions
What is the difference between IBS and a food allergy?
food allergy involves the immune system and can cause severe, immediate reactions like hives or anaphylaxis. IBS food intolerances (like to FODMAPs) involve the digestive system, causing delayed symptoms like gas, bloating, and pain hours after eating, without triggering an immune response.
Can IBS go away on its own?
IBS is a chronic condition, meaning it is long-lasting. Symptoms can wax and wane. You may experience long periods of relief (remission) followed by flare-ups. However, with proper management, many people achieve significant and long-term control over their symptoms.
Is there a cure for IBS?
There is currently no definitive cure for IBS. The goal of treatment is effective symptom management to improve quality of life. Research is ongoing, and our understanding of the gut-brain connection continues to evolve, leading to new and promising therapies.
Are probiotics really effective for IBS?
The evidence is mixed but promising for specific strains. Probiotics like Bifidobacterium infantis have shown efficacy in reducing overall symptoms, bloating, and bowel movement difficulty. It's not a one-size-fits-all solution, and it may take trial and error to find the best probiotic for your IBS subtype.
What are the worst foods for someone with IBS?
This is highly individual, but common trigger foods high in FODMAPs include: onions, garlic, wheat, beans, lentils, dairy products (high in lactose), certain fruits (apples, mangoes, watermelon), and artificial sweeteners (sorbitol, mannitol). Identifying personal triggers through a method like the Low FODMAP diet is key.