Post-Dialysis Care: Essential Tips for Maintaining Health and Well-Being
Post-dialysis care: Essential tips for maintaining health and well-being. Learn how to manage your health after dialysis and improve your quality of life.

Written by
Last updated on 3rd Jul, 2025
Introduction
Dialysis is a lifesaving treatment for individuals with kidney failure, as it helps remove waste, excess fluid, and toxins from the blood when the kidneys are no longer able to perform these essential functions. While dialysis can significantly improve quality of life and extend lifespan, the care required after a session is equally important to ensure the treatment is effective and to improve the patient’s overall quality of life. Post-dialysis care focuses on managing common side effects, staying hydrated, eating properly, taking the right medications, and seeking emotional support. This guide will provide actionable advice on how patients can best manage their well-being after dialysis sessions.
Understanding Dialysis and Its Impact
Dialysis is a process that removes waste products, excess fluids, and toxins from the blood when the kidneys are no longer able to do so. It helps maintain a balance of electrolytes in the body and prevents complications associated with kidney failure. There are two primary types of dialysis: hemodialysis and peritoneal dialysis.
1. Hemodialysis
Hemodialysis is the most common form of dialysis. It involves using a machine to filter the blood outside the body. Here's how it works:
Procedure: During a hemodialysis session, the patient's blood is drawn out through a needle inserted into a blood vessel, typically in the arm. The blood travels through a series of tubes into a dialyser (artificial kidney), where it is cleaned and filtered. The filtered blood is then returned to the body through another needle.
Frequency: Hemodialysis sessions typically occur three times a week, with each session lasting about 3-5 hours.
Location: Hemodialysis can be performed in a dialysis centre or at home, depending on the patient's condition and preferences.
2. Peritoneal Dialysis
Peritoneal dialysis uses the lining of the abdomen (peritoneum) as a natural filter to clean the blood. Here's how it works:
Procedure: A catheter is surgically inserted into the abdomen. During a session, dialysis solution is introduced into the abdominal cavity through the catheter. The solution absorbs waste and excess fluids from the blood through the peritoneum. After a few hours, the solution, now containing waste, is drained out and replaced with a fresh solution.
Frequency: There are two main types: Continuous Ambulatory Peritoneal Dialysis (CAPD), which involves manual exchanges several times a day, and Automated Peritoneal Dialysis (APD), which uses a machine to perform exchanges overnight while you sleep.
Location: Peritoneal dialysis can be performed at home, giving patients more flexibility and independence in managing their treatment.
Both types of dialysis are physically and emotionally demanding, which is why proper post-dialysis care is essential for overall health and well-being.
Common Side Effects After Dialysis
Going through dialysis can be a crucial part of managing kidney disease, but it's not without its side effects. Here's a look at some of the common ones.
Fatigue and Feeling Worn Out: Feeling tired or drained after dialysis is completely normal. Your body has just gone through a lot, so it needs some time to rest and recover.
Dizziness and Low Blood Pressure: Dialysis can sometimes cause a drop in blood pressure, making you feel dizzy or lightheaded. This happens when too much fluid is removed during treatment.
Muscle Cramps: Muscle cramps can be an annoying side effect after dialysis, caused by changes in fluid and electrolytes in your body.
Itchy Skin: If you notice your skin itching, it's often due to a buildup of waste products in the blood that haven't been fully filtered out. High phosphorus levels are usually to blame.
Nausea and Vomiting: Some people feel nauseous or even vomit during or after dialysis. This can happen when waste products are removed quickly or when there’s a shift in your body’s fluids.
Headaches: Headaches can be another side effect of dialysis, caused by changes in your blood pressure or the removal of waste products.
Infection Risk: Infections can happen at the site where dialysis needles are inserted or around a catheter in peritoneal dialysis.
Blood Clots: Blood clots can form at the access site, causing swelling, redness, or pain.
Consult Top Urologists
Post-Dialysis Care: Essential Tips for Patients
Going through dialysis can be tough, but taking care of yourself after each session is just as important for your health and well-being. Here are some essential tips to help you feel better and stay on top of your health after dialysis.
1. Managing Post-Dialysis Fatigue
Feeling tired or weak after dialysis is one of the most common complaints. This happens because the body undergoes a lot of changes during dialysis, and the treatment process itself can be physically demanding. To manage fatigue, consider the following:
Rest Adequately: Allow yourself enough time to recover after dialysis. Try to take naps or relax after your sessions to help recharge.
Stay Hydrated: Dehydration can worsen fatigue. Drinking enough water between dialysis sessions (as advised by your healthcare provider) can help maintain energy levels.
Eat Nutrient-Rich Meals: A balanced diet with sufficient protein, vitamins, and minerals can support energy levels. Include whole grains, fruits, vegetables, and lean proteins in your meals.
2. Hydration and Fluid Management
Managing hydration is one of the most critical aspects of post-dialysis care. Fluid balance can be difficult for dialysis patients since their kidneys no longer perform the task of regulating fluid levels. Here are some guidelines:
Follow Fluid Restrictions: Your healthcare team will provide specific guidelines on how much fluid you can safely consume between dialysis sessions. It’s important to follow these instructions to prevent fluid overload.
Monitor Swelling: If you notice swelling in your legs, ankles, or face, it could be a sign of excess fluid in your body. In such cases, contact your healthcare provider.
Use Salts Sparingly: Excess sodium (salt) in your diet can lead to fluid retention and increase the risk of high blood pressure. Avoid processed foods and salty snacks to maintain fluid balance.
3. Nutrition After Dialysis
Proper nutrition is essential for dialysis patients, as it helps the body heal, maintain strength, and prevent complications. Key considerations for post-dialysis nutrition include:
Focus on Protein: Dialysis can lead to the loss of protein from the body, so consuming high-quality protein sources such as lean meats, fish, eggs, and plant-based proteins is vital.
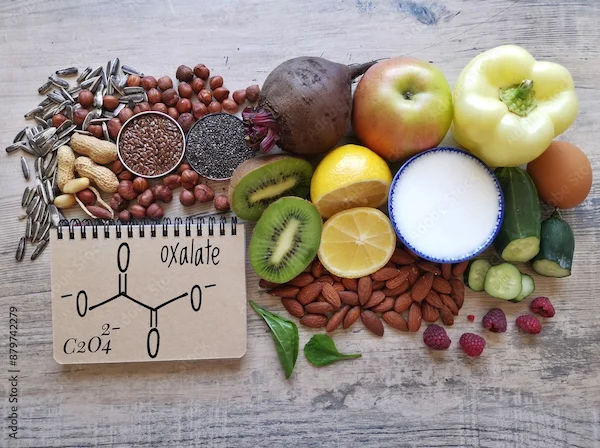
Limit Phosphorus and Potassium: Some foods high in phosphorus (like dairy products, nuts, and beans) and potassium (such as bananas, potatoes, and tomatoes) should be limited in your diet to prevent imbalances.
Balance Your Meals: Work with a renal dietitian to ensure you’re getting the right balance of nutrients based on your specific needs. A well-balanced meal plan can promote optimal kidney health and reduce the strain on your body.
4. Medication Management
After dialysis, it’s essential to follow your prescribed medication regimen carefully. Dialysis can affect how medications are absorbed and processed in the body, so make sure you:
Take Prescribed Medications on Time: Take your prescribed medications, such as phosphate binders or blood pressure medications, exactly as directed by your doctor.
Inform Your Doctor About New Medications: If you’re prescribed any new medications (including over-the-counter ones), make sure to consult your healthcare provider to ensure they are safe for dialysis patients.
Monitor for Side Effects: Be aware of any side effects from medications, especially if you experience new or unusual symptoms. Report these promptly to your healthcare team.
5. Emotional Support and Mental Well-being
Dialysis treatments can have a significant emotional impact on patients, especially when it becomes a regular part of life. It’s essential to address your mental health and seek emotional support if needed. Here’s how:
Reach Out for Support: Talking to friends, family, or a counsellor can help manage feelings of anxiety, stress, or depression related to your condition and treatment.
Join Support Groups: Connecting with other people who are going through similar experiences can provide emotional support and help you learn from others’ experiences.
Practice Relaxation Techniques: Techniques such as deep breathing, mindfulness, and meditation can help manage stress and improve mental clarity.
When to Seek Medical Attention
While post-dialysis care focuses on managing the common side effects of treatment, it’s important to know when to seek medical attention. You should contact your healthcare provider if:
You experience severe or prolonged fatigue, dizziness, or lightheadedness after dialysis sessions.
You have trouble breathing or notice significant swelling in your legs, abdomen, or face.
You notice changes in your urine output or experience discomfort while urinating.
You experience signs of infection, such as fever, redness, or swelling at your dialysis access site.
Conclusion
Taking care of yourself after dialysis is essential for staying healthy and feeling your best. By following these tips, you can support your recovery and improve your overall well-being. Always remember that your healthcare provider is there to help you every step of the way, so don't hesitate to reach out for advice and support. With the right care and attention, you can manage the challenges of dialysis and continue living a fulfilling life.
Consult Top Urologists
Consult Top Urologists

Dr. Sateesh Marriwada
Urologist
17 Years • MBBS, MS (General Surgery), Mch ( Genito Urinary Surgery)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr Tharaka Mourya Nutulapati
Urologist
7 Years • MBBS, MS (General Surgery), Mch ( Urology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Moin Mohammed Bavakatti
Urologist
13 Years • MBBS, MS (General Surgery), Mch (Urology), DNB (Urology), Diploma in Minimal Access Surgery, Fellow of Internal College of Robotic Surgeons), Vinci Surgical system, Fellow in Endocrinology, Clinical and Research fellow in Laparoscopic Urology, Laser Endourology & Laparoscopic & Robotic Urology, Fellowship in 3D laparoscopic Urology
Bengaluru
Dr Moin Mohammed Bhavikatti Clinic, Bengaluru
(150+ Patients)

Dr. Yogesh Taneja
Urologist
15 Years • MBBS , MS (General surgery), DNB (Genito Urinary Surgery)
Gurugram
Procyon Health, Gurugram
Dr. Mohammed Rehan Khan
Urologist
8 Years • MBBS, MS (General Surgery), Mch (Urology)
Barasat
Diab-Eat-Ease, Barasat
Consult Top Urologists

Dr. Sateesh Marriwada
Urologist
17 Years • MBBS, MS (General Surgery), Mch ( Genito Urinary Surgery)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr Tharaka Mourya Nutulapati
Urologist
7 Years • MBBS, MS (General Surgery), Mch ( Urology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Moin Mohammed Bavakatti
Urologist
13 Years • MBBS, MS (General Surgery), Mch (Urology), DNB (Urology), Diploma in Minimal Access Surgery, Fellow of Internal College of Robotic Surgeons), Vinci Surgical system, Fellow in Endocrinology, Clinical and Research fellow in Laparoscopic Urology, Laser Endourology & Laparoscopic & Robotic Urology, Fellowship in 3D laparoscopic Urology
Bengaluru
Dr Moin Mohammed Bhavikatti Clinic, Bengaluru
(150+ Patients)

Dr. Yogesh Taneja
Urologist
15 Years • MBBS , MS (General surgery), DNB (Genito Urinary Surgery)
Gurugram
Procyon Health, Gurugram
Dr. Mohammed Rehan Khan
Urologist
8 Years • MBBS, MS (General Surgery), Mch (Urology)
Barasat
Diab-Eat-Ease, Barasat
_5.webp)


_3.webp)