Guide to Kidney Transplant Nephrology: Are You Ready for the Journey?
Learn everything about kidney transplant nephrology—from eligibility, matching, and surgery to recovery, lifestyle, and long-term care. Prepare confidently for your transplant journey with clear, practical advice.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Mohammed Kamran MBBS, FIDM
Last updated on 13th Jan, 2026
_3.webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Introduction
Kidney disease can creep up silently, but when the kidneys can no longer perform their vital functions, a kidney transplant can be life-changing. This guide to kidney transplant nephrology will help you understand whether you’re prepared for the journey—especially if you’re living with chronic kidney disease (CKD).
We’ll explain who benefits most from a transplant, how eligibility is assessed, what to expect on the waiting list, and how life changes after surgery. You’ll learn about living versus deceased donors, matching and paired exchange, medicines that protect your new kidney, and the day-to-day habits that keep it healthy. We’ll also cover realistic risks, costs, and a practical checklist to help you make informed decisions.
If your doctor has mentioned transplant—or you’re asking, “Am I ready?”—this guide will help you plan your next move. If you experience swelling, extreme fatigue, or persistent changes in urination beyond two weeks, consult a doctor online with Apollo24|7 for timely evaluation and care.
Consult a Top Nephrologist for Personalised Advice
Kidney Transplant: How It Helps Chronic Kidney Disease
A transplant offers a life-changing solution for those living with advanced kidney disease, restoring function and improving quality of life.
CKD in Stages: When Kidneys Struggle
Chronic kidney disease progresses through five stages based on estimated glomerular filtration rate (eGFR). Early stages may cause few symptoms, while later stages bring swelling, tiredness, breathlessness, and changes in urination. Transplant nephrology focuses on restoring kidney function by replacing the failing organ, which filters waste, balances fluids, and supports blood pressure and bone health.
Why Transplant Often Beats Long-Term Dialysis
For many with advanced kidney disease, a transplant offers better survival and quality of life than dialysis. Patients typically regain energy, experience fewer dietary restrictions, and return to work or study sooner. However, factors such as age, medical history, and donor availability all influence outcomes.
Who Benefits Most and Who May Not
- A transplant benefits those with irreversible kidney failure, reasonable heart and lung health, and the ability to take medicines reliably. Conditions like active infection, untreated cancer, or inability to adhere to treatment can delay candidacy.
- Unique insight: Don’t wait until dialysis starts—early evaluation (eGFR below 20 mL/min) improves fitness and can increase your chances of a pre-emptive transplant.
Are You a Candidate? Evaluation and Readiness
Understanding your medical fitness and completing the right tests are key to determining transplant readiness.
Medical Tests You Can Expect
Expect comprehensive checks including:
- Blood tests (blood type, tissue typing, kidney and liver function, viral screening, and diabetes tests)
- Imaging (ultrasound or CT scan)
- Heart assessments (ECG, echocardiogram, or stress test)
- Cancer and dental screening to eliminate infection risks
If you need updated results, Apollo 24|7 offers convenient home collection for creatinine, eGFR, urine albumin, and HbA1c tests.
Absolute vs Relative Contraindications
- Absolute contraindications include uncontrolled infection, metastatic cancer, or inability to take immunosuppressants. Relative contraindications such as heart disease, obesity, or frailty may be improved through targeted treatment and rehabilitation.
- Unique insight: Frailty increases risk—“prehabilitation” with tailored exercise and nutrition can enhance recovery.
Prehabilitation: Strength, Nutrition, and Vaccines
- Exercise: Gentle resistance and balance work 3–5 times a week.
- Nutrition: Adequate protein (0.8–1.0 g/kg/day) and limited sodium (<2 g/day).
- Vaccines: Complete non-live vaccines (hepatitis B, pneumococcal, COVID-19, flu) before transplant.
Donors and Matching: Living, Deceased, and Paired Exchange
Finding the right donor match is vital for a successful transplant and long-term kidney survival.
Blood Types, HLA, and Crossmatch Explained
Compatibility depends on blood type, HLA tissue matching, and a crossmatch test to ensure no immune reaction between donor and recipient.
Living Donor Advantages
Living donor kidneys usually work immediately, last longer, and reduce waiting times. Donors undergo detailed assessments and typically live normal, healthy lives with regular follow-up.
When a Swap Solves Incompatibility
Paired kidney exchange allows incompatible donor–recipient pairs to “swap” kidneys with others, expanding access for hard-to-match patients.
From Waitlist to Operating Room: The Transplant Journey
The road from evaluation to surgery involves careful coordination, patience, and preparation.
Getting Listed: What to Expect
Your transplant centre submits your details to a national or regional system. Wait time depends on blood type, antibodies, and location. Keep health updates current to maintain eligibility.
The Call, the Surgery, and Hospital Stay
- Once a kidney becomes available, surgery typically lasts 2–4 hours. The new kidney is placed in the lower abdomen and connected to your blood vessels and bladder. Most people stay in the hospital for 3–7 days.
- Unique insight: Prepare a “go bag” (ID, medication list, charger, loose clothes) and nominate an emergency contact.
Recovery Week by Week
- Weeks 1–2: Soreness and fatigue; energy gradually improves.
- Weeks 3–12: Frequent clinic visits for medication adjustments.
- Months 3–12: Routine stabilises; most people return to work within 8–12 weeks.
Medicines and Monitoring: Protecting Your New Kidney
Long-term success depends on taking your medicines correctly and attending regular follow-up appointments.
The “Big Three” Immunosuppressants
Typical regimens include:
- Tacrolimus or Cyclosporine (calcineurin inhibitors)
- Mycophenolate or Azathioprine (antimetabolites)
- Prednisone (steroid, tapered to the lowest effective dose)
Common Side Effects and Management
Tacrolimus can raise blood pressure or sugar levels; Mycophenolate may cause stomach upset; steroids may affect mood and weight. Regular lab checks ensure correct dosing. Apollo24|7 offers home collection for tacrolimus and kidney function monitoring.
Building Routines for Perfect Adherence
Use reminders, pillboxes, and keep an updated medicine list. Never skip doses—contact your care team for advice if you do.
Living Well After Transplant
Healthy habits, good nutrition, and mental well-being are key to maintaining your kidney and overall health.
Diet and Nutrition
Focus on lean proteins, fruits, and whole grains. Limit salt, and avoid raw or unpasteurised foods to reduce infection risk. A renal dietitian can tailor advice to your needs.
Exercise, Work, and Mental Health
Begin gentle walking and breathing exercises early, increasing activity gradually. Many return to work within 8–12 weeks. Counselling and peer support help manage anxiety or fear of rejection.
Vaccines, Travel, and Pregnancy
Keep non-live vaccines up to date, delay long travel for 3 months, and discuss pregnancy plans with your nephrologist—most centres recommend waiting at least a year.
Risks to Know and How to Respond
Recognising risks early helps prevent complications and ensures long-term kidney function.
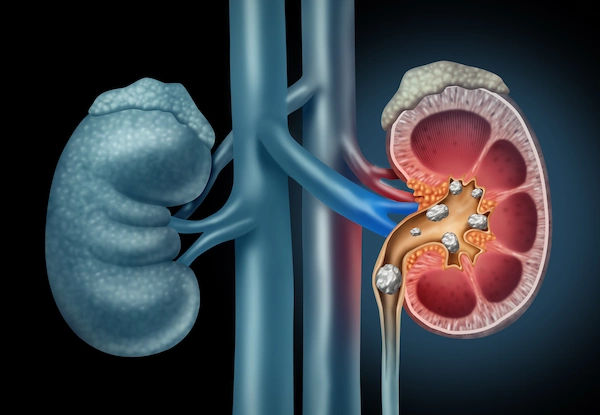
Rejection and Warning Signs
Watch for decreased urine output, swelling, fever, or tenderness near the graft. Some rejection is silent—regular blood tests are essential.
Infections and Skin Cancer
Report fevers promptly. Wear sunscreen and protective clothing—immunosuppression increases skin cancer risk.
Other Risks
Post-transplant diabetes and high blood pressure are common but manageable. Some original kidney conditions can recur, so ongoing monitoring is vital.
Costs, Access, and Support Systems
Understanding your financial, emotional, and social resources helps sustain your recovery long-term.
Insurance and Budgeting
Costs vary but include surgery, medication, and lifelong follow-up. Discuss your coverage with your centre’s financial counsellor. Assistance programmes may help with medicine expenses.
Social and Emotional Support
A reliable caregiver is essential for appointments and recovery. Support groups and counselling can reduce anxiety and improve long-term outcomes.
Your Preparation Checklist
Preparation helps you stay organised and confident before and after your transplant.
Step-by-Step Readiness Plan
- Early evaluation (eGFR <20)
- Fitness and nutrition improvements
- Complete vaccinations
- Medication plan and reminders
- Prepare your go bag and contact tree
- Explore living or paired donation
- Budget for lifelong medicines
- Arrange regular tests (Apollo 24|7 offers home collection)
Questions to Ask Your Team
- Am I eligible for pre-emptive transplant?
- What are my donor options?
- Which immunosuppressants will I need?
- How will we manage my other health conditions?
Conclusion
A kidney transplant marks the beginning of a new chapter—one that demands care, discipline, and partnership with your medical team.
A kidney transplant is more than a medical procedure—it’s a lifelong partnership between you, your kidney, and your care team. By preparing early, maintaining fitness, adhering to medication, and attending regular check-ups, you can protect your new kidney and lead a full, healthy life.
Risks such as rejection and infection are real but manageable with vigilance and support. Surround yourself with informed caregivers and use trusted tools like Apollo 24|7 for online consultations and home lab collection to stay consistent with your follow-up. With commitment and knowledge, you can move from managing kidney disease to truly thriving after a transplant.
Consult a Top Nephrologist for Personalised Advice
Consult a Top Nephrologist for Personalised Advice
Dr Gayatri Pegu
Nephrologist
15 Years • MD (General Medicine) DM(Nephrology)
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr Praveen Kumar Etta
Nephrologist
10 Years • MBBS,MD DM(SGPGI) FORMER ASST(PIMS)
Hyderabad
Apollo Spectra Ameerpet, Hyderabad

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly
Consult a Top Nephrologist for Personalised Advice
Dr Gayatri Pegu
Nephrologist
15 Years • MD (General Medicine) DM(Nephrology)
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr Praveen Kumar Etta
Nephrologist
10 Years • MBBS,MD DM(SGPGI) FORMER ASST(PIMS)
Hyderabad
Apollo Spectra Ameerpet, Hyderabad

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly
More articles from Kidney Disease
Frequently Asked Questions
How long do kidney transplants last?
Living donor kidneys often function 12–20 years, while deceased donor kidneys average 10–15 years. Consistent follow-up and adherence extend graft life.
Can I get a transplant before dialysis?
Yes, early (pre-emptive) transplants offer better outcomes. Ask your team about evaluation once eGFR drops below 20 mL/min.
What are early signs of rejection?
Reduced urine, swelling, fever, or tenderness. Some cases are silent—regular lab checks are crucial. For advice, contact an Apollo24|7 nephrologist online.
Will I need to change my diet after transplant?
Yes—focus on balanced, heart-healthy eating and food safety. A dietitian can personalise your plan.
How soon can I return to work and exercise?
Most resume light activity within a few weeks and full work in 8–12 weeks, depending on recovery.