A Complete Guide to Dialysis: Types, Risks, and Complications
Learn everything about dialysis—types, processes, risks, complications, diet, and lifestyle tips. A complete guide for patients and caregivers.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Md Yusuf Shareef MBBS, Advanced Certificate Course in Dermatology
Last updated on 13th Jan, 2026

Understanding Your Options: The Two Main Types of Dialysis
Dialysis essentially performs the job of failed kidneys artificially. There are two primary methods, each with its own procedure, schedule, and lifestyle implications. Understanding these dialysis types is the first step in determining which might be the best fit for you.
Haemodialysis (HD): How It Works
Haemodialysis is the most common form of dialysis. It uses a machine called a dialyser, which acts as an artificial kidney to clean your blood outside your body.
The Haemodialysis Process Step-by-Step
Access: Your blood is safely diverted from your body through a special access point, typically in your arm.
- Filtration: The blood travels through soft tubes to the dialyser. Inside this filter, your blood flows through thin fibres, while a special fluid (dialysate) flows on the outside. Waste products and extra fluid pass from your blood into the dialysate through tiny pores.
- Return: The cleaned blood is then returned to your body through another tube.
- A standard haemodialysis session lasts about 3–4 hours and is usually needed three times a week at a dialysis centre. Some patients may opt for home haemodialysis, which can allow for more frequent, shorter sessions.
Vascular Access: The Lifeline for Haemodialysis
The access point is crucial. The three main types are:
- Arteriovenous (AV) Fistula: A surgically created connection between an artery and a vein. It’s the preferred option due to its lower risk of infection and clots.
- AV Graft: A synthetic tube used to connect an artery and a vein if your veins are too small for a fistula.
- Central Venous Catheter (CVC): A tube inserted into a large vein in the neck or chest. This is usually a temporary solution but carries a higher risk of infection.
Peritoneal Dialysis (PD): How It Works
Peritoneal dialysis uses the natural lining of your abdomen (the peritoneum) as a filter. A sterile cleansing fluid (dialysate) is introduced into your abdominal cavity through a permanent catheter.
Consult a Specialist for Personalised Advice
The Peritoneal Dialysis Process Step-by-Step
Fill: The dialysate flows into your abdomen through the catheter and dwells there for a prescribed period (usually 4–6 hours, called a "dwell time").
- Dwell: During this time, waste products and excess fluid pass from the blood vessels in your peritoneal membrane into the dialysate.
- Drain: After the dwell time, the used fluid, now containing the wastes, is drained out of your abdomen into a sterile bag and discarded.
- This drain-fill-dwell cycle, called an exchange, is typically repeated 4–5 times a day. Alternatively, a machine (cycler) can perform these exchanges automatically while you sleep, a method known as Automated Peritoneal Dialysis (APD).
The PD Catheter: Your Access Point
A soft plastic tube (catheter) is surgically placed into your abdomen. This catheter remains there permanently and is used to pour in and drain out the dialysate fluid. Proper care of the catheter site is essential to prevent peritoneal dialysis infection, known as peritonitis.
Head-to-Head: Comparing Haemodialysis and Peritoneal Dialysis
Choosing between HD and PD is a personal decision based on your health, lifestyle, and preferences. Here’s a breakdown of the pros and cons.
Pros and Cons of Haemodialysis
- Pros: Treatment is supervised by medical professionals. You have days off between sessions. No equipment or supplies are stored at home.
- Cons: Requires strict adherence to a treatment schedule at a centre. Travel to and from the centre is necessary. Diet and fluid intake restrictions are often more stringent. There can be significant "ups and downs" in how you feel before and after sessions.
Pros and Cons of Peritoneal Dialysis
- Pros: Offers greater flexibility and independence. Can be done at home, work, or while travelling. Provides a more consistent blood cleansing, leading to fewer dietary restrictions. No needles are required for each treatment.
- Cons: Requires daily treatment without a day off. Demands a significant commitment to cleanliness to avoid infection. Requires space to store supplies at home. May not be suitable for everyone, such as those with certain abdominal surgeries or severe inflammatory bowel disease.
Navigating the Risks and Common Complications of Dialysis
While life-saving, all medical procedures carry potential dialysis risks and complications. Being aware of them helps in early detection and management.
Risks Associated with Haemodialysis
- Low Blood Pressure (Hypotension): The most common side effect, caused by fluid removal. Symptoms include dizziness, nausea, and fainting.
- Muscle Cramps: Often occur during or after treatment, frequently due to fluid removal and electrolyte shifts.
- Infection: The vascular access site, especially catheters, is a potential entry point for bacteria.
- Blood Clots: Can form in the vascular access, particularly in grafts and fistulas.
- Disequilibrium Syndrome: A rare but serious condition caused by rapid changes in the body's chemistry, leading to headaches, nausea, and, in severe cases, seizures.
Risks Associated with Peritoneal Dialysis
- Peritonitis: The most serious and common complication of PD. Characterised by cloudy dialysis drain fluid, abdominal pain, and fever. Requires immediate medical attention.
- Hernia: The constant presence of fluid in the abdomen increases pressure, which can weaken abdominal muscles and lead to a hernia.
- Weight Gain: The dialysate contains sugar (dextrose), which can be absorbed by the body, leading to extra calorie intake and potential weight gain.
- Catheter Site Infection: The skin around the catheter can become red, tender, and infected.
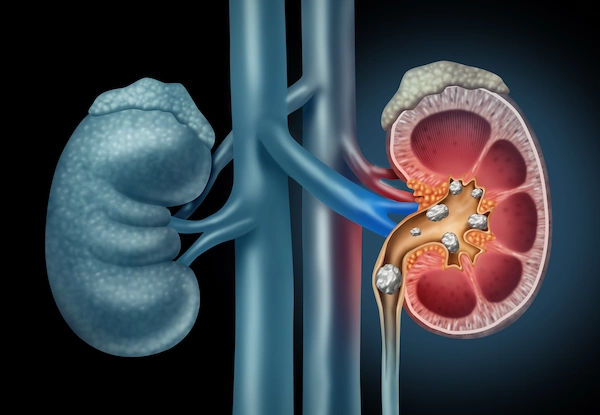
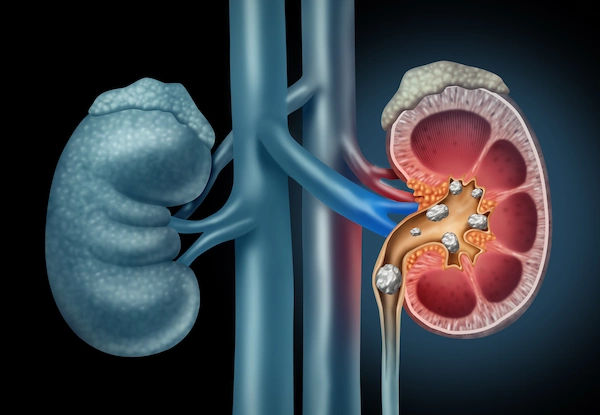
General Health Risks for All Dialysis Patients
- Anaemia: Failing kidneys produce less erythropoietin (EPO), a hormone that stimulates red blood cell production. This, combined with blood loss during dialysis, can lead to severe anaemia and fatigue.
- Bone Diseases: Kidneys play a key role in calcium and phosphorus balance. Dysregulation can lead to weak bones.
- Cardiovascular Disease: Dialysis patients are at a significantly higher risk for heart disease and stroke.
- Dietary Challenges: Managing intake of potassium, phosphorus, sodium, and fluids is critical and can be difficult.
If you experience persistent symptoms like severe fatigue, unusual swelling, or signs of infection, it is crucial to consult a doctor online with Apollo24|7 for prompt evaluation and guidance.
Life on Dialysis: Diet, Lifestyle, and Mental Wellbeing
Adapting to life on dialysis is a journey. A key part of managing your health and minimising complications involves strict attention to diet and mental health.
The Renal Diet: What to Eat and Avoid
A kidney-friendly diet helps control the buildup of waste and fluid. Key principles include:
- Limit Sodium: To control thirst and prevent fluid overload and high blood pressure.
- Manage Potassium: High levels can be dangerous for the heart. Foods like bananas, oranges, and potatoes are often limited.
- Reduce Phosphorus: High levels can weaken bones. This means limiting dairy, nuts, and colas.
- Monitor Protein: Intake needs are carefully balanced—enough for strength, but not too much to create excess waste.
- Watch Fluid Intake: Because your kidneys aren't removing fluid, intake between sessions must be controlled to prevent swelling and shortness of breath.
A registered dietitian can create a personalised plan for you. For those monitoring their health through tests, Apollo24|7 offers convenient home collection for tests like electrolyte panels to track potassium and sodium levels.
Managing Fatigue and Staying Active
Fatigue is extremely common. Combat it by:
- Prioritising Sleep: Establish a regular sleep routine.
- Incorporating Gentle Exercise: Short walks or light stretching can boost energy levels.
- Planning Your Day: Schedule demanding tasks for when you have the most energy.
- Seeking Support: Talking to a counsellor or joining a patient support group can be invaluable for your mental health.
Conclusion: Taking Control of Your Kidney Health
A diagnosis that leads to dialysis is undoubtedly life-changing, but it is not the end of life—it's the beginning of a new chapter managed with care and knowledge. Understanding the types of dialysis, from in-centre haemodialysis to at-home peritoneal dialysis, empowers you to actively participate in your treatment decisions. Being vigilant about potential risks and complications, from infections to dietary challenges, allows for early intervention and better outcomes.
Remember, you are not alone on this journey. Your healthcare team, including your nephrologist, dialysis nurses, and dietitian, is your greatest ally. By adhering to your treatment plan, maintaining a kidney-friendly lifestyle, and prioritising your mental wellbeing, you can manage your health effectively and maintain a good quality of life. If you have any concerns about your symptoms or treatment plan, always reach out to your medical team. For ongoing management and consultations, you can easily book a physical visit to a doctor with Apollo24|7 to ensure continuous and comprehensive care.
Consult a Specialist for Personalised Advice
Consult a Specialist for Personalised Advice

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr Suseela
General Physician
5 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ritesh Motghare
General Practitioner
18 Years • MBBS PGCDM
Nagpur
HEALTH CENTRE VNIT NAGPUR, Nagpur

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult a Specialist for Personalised Advice

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr Suseela
General Physician
5 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ritesh Motghare
General Practitioner
18 Years • MBBS PGCDM
Nagpur
HEALTH CENTRE VNIT NAGPUR, Nagpur

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from Kidney Failure
Frequently Asked Questions
What are the stages of kidney failure before needing dialysis?
Kidney failure is categorized into five stages based on your Glomerular Filtration Rate (GFR). Dialysis typically begins in Stage 5, also known as End-Stage Renal Disease (ESRD), when kidney function is less than 15%.
What is the life expectancy on dialysis?
Life expectancy varies widely based on age, overall health, and the presence of other conditions like diabetes or heart disease. On average, patients can live for 5-10 years on dialysis, though many live for 20 or even 30 years.
Can you ever stop dialysis once you start?
Yes, but only if kidney function recovers sufficiently, which is rare in chronic kidney disease. Dialysis may be stopped if a patient receives a successful kidney transplant or, in some palliative care situations, if the patient chooses to discontinue treatment.
How do I know if I have a peritoneal dialysis infection?
The hallmark sign is cloudy dialysis drain fluid. Other symptoms include abdominal pain or tenderness, fever, nausea, and redness or swelling around the catheter site. If you notice these signs, contact your healthcare team immediately.
Is home dialysis vs center dialysis better?
There is no universal 'better' option. Home dialysis (like PD or home HD) offers more flexibility and independence, while in-center HD provides direct medical supervision. The best choice depends on your medical condition, lifestyle, personal motivation, and home environment.