A New Hope for Kidney Patients Beating Blood Type Barriers in Transplant
Know about the kidney patients who struggle with blood type barriers, transplantation, and how paired donor exchange works.learns about the transplantation procedure and desensitisation therapy.

Written by Dr. Md Yusuf Shareef
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026
Introduction
For thousands of people with end-stage kidney disease, a transplant from a living donor is the gold standard of treatment, offering a better quality of life and long-term survival compared to dialysis. But for decades, a fundamental biological hurdle stood in the way: blood type incompatibility. Imagine a loved one, a spouse, sibling, or friend, is willing and eager to donate a kidney, only to be told they are not a match because of their blood type. This heartbreaking scenario was once a dead end. Today, it is not. Medical science has advanced to a point where blood group incompatibility is no longer an absolute constraint for a kidney donor transplant. This article is your comprehensive guide to the revolutionary strategies, paired exchange and desensitisation that are turning willing donors into life-saving matches, offering new hope and expanding the pool of available organs for those in need.
Understanding the Blood Type Barrier
The blood type barrier includes:
The ABO System: Why Compatibility Matters
Your blood type (A, B, AB, or O) is determined by specific sugar molecules, called antigens, on the surface of your red blood cells and other tissues, including your kidneys. Your immune system is trained to recognise your own antigens as "self." If it encounters foreign antigens from an incompatible blood type, it will mount a powerful attack by producing antibodies. This is the same principle that makes matching blood types essential for blood transfusions. In the context of a kidney donor transplant, if a recipient with type A blood receives a kidney from a type B donor, their anti-B antibodies would immediately recognise the donor kidney as foreign and cause hyperacute rejection, destroying the organ within minutes.
Consult a Top Nephrologist for Personalised Advice
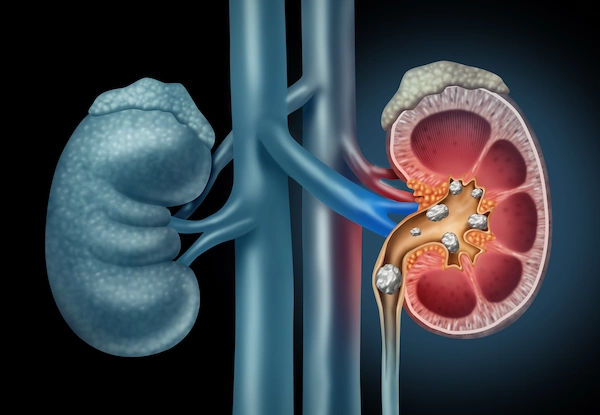
The Dangers of an Incompatible Transplant
Before modern solutions, attempting an ABO-incompatible transplant was futile and dangerous. The recipient's pre-existing antibodies would lead to rapid and irreversible organ failure. This biological barrier meant that a willing and healthy living donor could only donate to a recipient with a compatible blood type, drastically limiting the possibilities for many patients and forcing them to wait longer on the deceased donor list.
The Transplant Revolution: Overcoming Incompatibility
The past two decades have seen remarkable breakthroughs that effectively dismantle the blood type barrier. The two primary strategies are paired kidney exchange and medical desensitisation.
Paired Kidney Exchange: A Clever "Swap" System
This innovative approach doesn't change the biology of the donor or recipient; instead, it changes the pairing. It's often described as a "kidney swap."
How a Paired Donor Exchange Works?
In a simple scenario, consider two incompatible donor-recipient pairs:
Pair 1: Mr Sharma (Recipient, Type A) and his wife (Donor, Type B) - Incompatible.
Pair 2: Ms Patel (Recipient, Type B) and her brother (Donor, Type A) - Incompatible.
A paired exchange program facilitates a "swap." Mrs Sharma (Type B) donates her kidney to Ms Patel (Type B), who is a compatible match. In return, Mr Patel (Type A) donates his kidney to Mr Sharma (Type A). Both recipients get a compatible living donor kidney through the generosity of each other's donors.
The Power of Chain Transplants
These exchanges can become complex and powerful chains, often initiated by an altruistic or "Good Samaritan" donor—someone who wishes to donate to anyone in need. This single donor can start a chain of transplants that benefits multiple recipients across the country, with each recipient's willing donor "paying it forward" to the next person in the chain.
Medical Desensitisation: "Retraining" the Immune System
When a paired exchange isn't feasible or a recipient has a very specific donor in mind, desensitisation offers a direct solution. This advanced medical protocol aims to lower the level of harmful antibodies in the recipient's blood before the transplant, effectively "retraining" the immune system to accept the new organ.
The Process of Desensitisation Therapy
Desensitisation is a carefully managed process that typically involves:
1. Plasmapheresis: A procedure similar to dialysis where the patient's plasma (which contains the antibodies) is removed and replaced with donor plasma or a substitute.
2. Intravenous Immunoglobulin (IVIG): Administration of IVIG, which is a solution of antibodies from thousands of healthy donors. IVIG helps modulate the immune system and reduce antibody production.
3. Immunosuppressive Drugs: Patients receive powerful medications before and after the transplant to further suppress antibody production.
This process significantly reduces the risk of rejection, making a successful ABO incompatible kidney transplant a reality. A study published in the New England Journal of Medicine showed that the 8-year survival rate for patients who underwent desensitisation was nearly identical to those who received compatible transplants.
Choosing the Right Path: Paired Exchange vs. Desensitisation
The decision between these two options is complex and is made by a multidisciplinary transplant team in consultation with the patient and donor.
Pros and Cons at a Glance
Paired Exchange:
* Pros: Avoids the need for intense pre-transplant therapy, may lead to a better HLA tissue match, and can help multiple people.
* Cons: Requires coordination between multiple pairs, can involve logistical challenges if pairs are at different transplant centres.
Desensitization:
* Pros: Allows a specific donor to give to their intended recipient, and can be faster if no match is found in a paired pool.
* Cons: Involves a more complex medical regimen with a slightly higher initial risk of rejection and infection, and can be more expensive.
The Living Donor Transplant Journey: Step-by-Step
The phases include:
Phase 1: The Extensive Evaluation
Both the donor and recipient undergo rigorous medical and psychological testing to ensure they are healthy enough for the procedure and that the donation is safe. This includes blood tests, imaging scans, heart and lung evaluations, and meetings with social workers and transplant coordinators. If you are considering becoming a living kidney donor, consulting a specialist team at a hospital like those available through Apollo24|7 can provide clarity on the process and your eligibility.
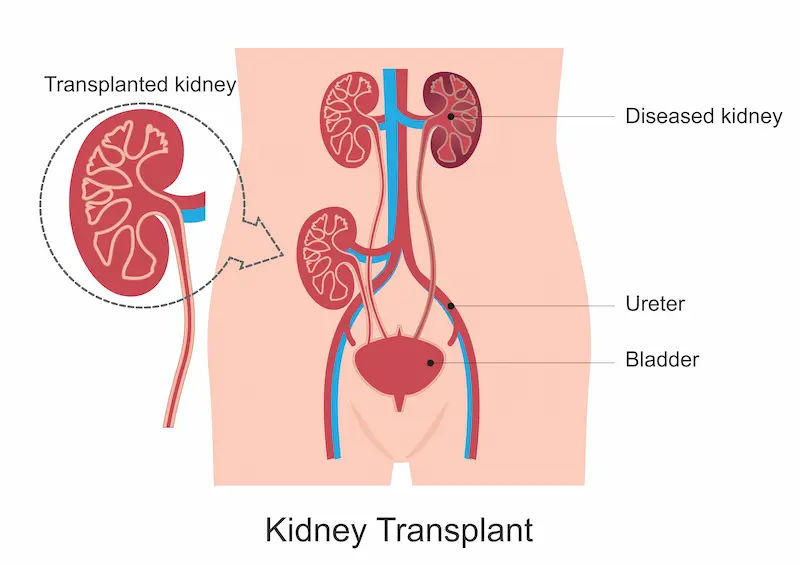
Phase 2: Preparation and the Procedure
Once approved, the path diverges based on the chosen strategy (exchange or desensitisation). The donor surgery (nephrectomy) is typically minimally invasive (laparoscopic), involving small incisions. The healthy kidney is removed and immediately transplanted into the recipient in a nearby operating room. The recipient's surgery involves placing the new kidney in the lower abdomen and connecting it to the blood vessels and the bladder.
Phase 3: Recovery and Long-Term Health
1. Donor: Hospital stay is typically 1-3 days. Full recovery takes 4-6 weeks. Donors can live a normal, healthy life with one kidney.
2. Recipient: Hospital stay is longer, often 5-10 days. Lifelong immunosuppressive medications are crucial to prevent rejection. Regular monitoring of kidney function through tests like creatinine levels is essential. Apollo24|7 offers convenient home collection for these vital post-transplant tests, making ongoing care more manageable.
Success Rates and Long-Term Outcomes
Living donor transplants have excellent success rates. According to the Organ Procurement and Transplantation Network (OPTN), the 5-year survival rate for living donor kidney transplants is over 90%. While ABO incompatible kidney transplant and paired exchange programs have success rates that are nearly comparable to compatible transplants, especially at experienced centres.
Conclusion
The landscape of kidney donor transplant has been transformed. The once-insurmountable wall of blood type incompatibility has been breached by medical ingenuity and collaborative programs. These advances mean that a willing, healthy donor is a potential match for their intended recipient more often than not. If you or a loved one is facing kidney failure and has a potential donor, it is crucial to seek evaluation at a major transplant center experienced in these advanced protocols. The question is no longer "Are we a match?" but rather "What is the best path to make this transplant happen?" This new era offers profound hope, ensuring that the gift of life is within reach for many more patients waiting for a second chance. If you have questions about kidney health or the transplant process, consulting a nephrologist online with Apollo24|7 can be a valuable first step.
Consult a Top Nephrologist for Personalised Advice
Consult a Top Nephrologist for Personalised Advice
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr Praveen Kumar Etta
Nephrologist
10 Years • MBBS,MD DM(SGPGI) FORMER ASST(PIMS)
Hyderabad
Apollo Spectra Ameerpet, Hyderabad

Dr Ajay Kumar Sharma
Transplant Specialist Surgeon
39 Years • MBBS, MS, DNB, FRCS (Glas), FRCS (Edin), FRCS (General Surgery), MSc Medical Education
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly
Consult a Top Nephrologist for Personalised Advice
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr Praveen Kumar Etta
Nephrologist
10 Years • MBBS,MD DM(SGPGI) FORMER ASST(PIMS)
Hyderabad
Apollo Spectra Ameerpet, Hyderabad

Dr Ajay Kumar Sharma
Transplant Specialist Surgeon
39 Years • MBBS, MS, DNB, FRCS (Glas), FRCS (Edin), FRCS (General Surgery), MSc Medical Education
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly
More articles from Kidney Failure
Frequently Asked Questions
1. What is the cost difference between a compatible and an ABO incompatible kidney transplant?
Desensitisation therapy adds significant cost due to the medications (especially IVIG) and additional procedures like plasmapheresis. An ABO-incompatible transplant can be 20-50% more expensive than a compatible one. However, many insurance providers now cover these protocols as they are considered standard of care. A paired exchange typically does not incur these extra costs.
2. How long does the desensitisation process take before the actual transplant?
The process usually begins several weeks before the scheduled transplant date. It involves multiple sessions of plasmapheresis/IVIG over a period of 2-4 weeks, followed by the transplant surgery once antibody levels have been successfully reduced to a safe threshold.
3. Are the long-term risks higher for a recipient who had a desensitisation protocol?
Initially, the risk of rejection is slightly higher, but with close monitoring and modern immunosuppression, long-term outcomes are now very similar to those of compatible transplants. The key is adherence to medication and lifelong follow-up care.
4. Can a person with O blood type receive a kidney from any other blood type?
No. People with type O blood can only receive kidneys from type O donors because they have antibodies against both A and B antigens. However, a type O donor is a 'universal donor' and can donate to recipients of any blood type (A, B, AB, or O).
5. What happens if a desensitised patient's antibody levels rise again after the transplant?*
This is a managed risk. Patients are monitored very closely. If antibody levels rise, doctors may administer additional doses of IVIG or adjust immunosuppressive medications to control the response and protect the transplanted kidney.

_2.webp)