What Leads To Signs Of Kidney Failure Management
Learn how to manage kidney failure effectively with treatment options like dialysis and transplant, diet and nutrition tips, medication guidance, fluid control, mental health support, and lifestyle changes for better outcomes.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

The kidneys are your body's master chemists, tirelessly filtering waste, balancing fluids and electrolytes, and releasing hormones that regulate blood pressure and produce red blood cells. Kidney failure occurs when these organs lose approximately 85-90% of their function and can no longer sustain life independently. This is a chronic condition, meaning it develops over time, often as a result of diabetes or high blood pressure. Understanding that kidney failure is a manageable condition, not an immediate end, is the foundational mindset for successful long-term care. The goal of management shifts from curing the disease to replacing lost function and preventing complications.
The Primary Causes Leading to Kidney Failure
Effective management begins with understanding the root cause, as it often informs ongoing care strategies. The two most common culprits are:
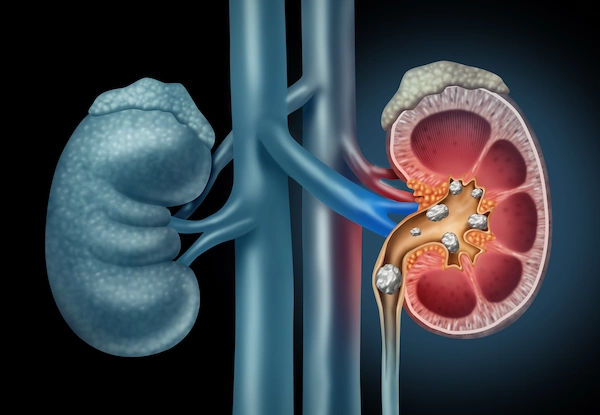
- Diabetes (Diabetic Nephropathy): Chronically high blood sugar levels damage the tiny blood vessels within the kidney's filtering units (glomeruli). This is the leading cause of ESRD globally.
- High Blood Pressure (Hypertensive Nephrosclerosis): Uncontrolled hypertension forces the heart to work harder and damages blood vessels throughout the body, including the delicate ones in the kidneys, impairing their filtering ability.
Other significant causes include autoimmune diseases like Lupus, genetic conditions such as Polycystic Kidney Disease (PKD), prolonged urinary tract obstructions, and recurrent kidney infections.
The Core Pillars of Kidney Failure Management
Managing kidney failure successfully rests on four interdependent pillars. Neglecting one can destabilise the entire treatment plan.
Medical Treatment Options: Dialysis and Transplant
This pillar involves the artificial replacement of lost kidney function.
- Dialysis: This treatment filters waste and excess fluid from your blood. There are two main types:
- Hemodialysis (HD): Blood is circulated outside the body through a machine (a dialyser) that acts as an artificial
kidney. This is typically done at a clinic 3-4 times a week. - Peritoneal Dialysis (PD): The inside lining of your own abdomen (the peritoneum) acts as a natural filter. A cleansing fluid (dialysate) is introduced and drained via a catheter, a process often done at home, offering more flexibility.
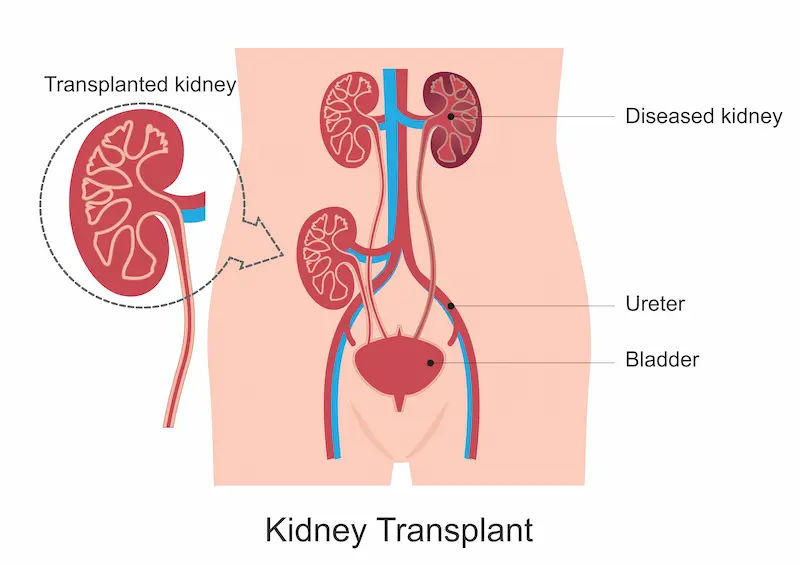
- Kidney Transplant: This is the closest treatment to a cure. A healthy kidney from a living or deceased donor is surgically placed into your body. While a transplant offers the best long-term outcomes and freedom from dialysis, it requires lifelong immunosuppressant medications to prevent organ rejection.
The Critical Role of Diet and Nutrition
A renal diet is a therapeutic diet designed to reduce the workload on your kidneys. It is not a suggestion but a prescription. Key components include:
- Sodium Restriction: To control blood pressure and prevent fluid overload and swelling.
- Potassium Management: High potassium levels can cause dangerous heart arrhythmias. Foods like bananas, oranges, potatoes, and tomatoes are often limited.
- Phosphorus Control: Damaged kidneys can't remove phosphorus, leading to weak bones and vascular calcification. This means limiting dairy, nuts, and dark sodas.
- Protein Monitoring: Protein intake must be carefully balanced—enough to maintain muscle mass but not so much that it creates excess waste products. Working with a renal dietitian is essential for creating a personalised and sustainable meal plan.
Medication Adherence and Management
Medications are crucial for managing the symptoms and consequences of kidney failure. Common prescriptions include:
- Phosphate Binders: Taken with meals to prevent phosphorus from food from entering the bloodstream.
- Erythropoiesis-Stimulating Agents (ESAs): To treat anaemia by stimulating red blood cell production.
- Blood Pressure Medications: Such as ACE inhibitors or ARBs, which also help protect the kidneys.
- Diuretics: To help the body eliminate extra fluid.
- Vitamin D and Calcium Supplements: To support bone health.
Skipping doses or incorrectly managing medications can lead to immediate and severe health setbacks.
Monitoring and Controlling Fluid Intake
With failed kidneys, urine output drops significantly, and fluid can quickly build up in the body. This fluid overload leads to swelling (edema), shortness of breath (as fluid fills the lungs), and high blood pressure, putting immense strain on the heart. Strict fluid management involves tracking all liquid intake (including foods like soup and ice cream) and adhering to the limit set by your nephrologist, which is based on your urine output and dialysis schedule.
The Importance of Mental and Emotional Health
A kidney failure diagnosis is a life-altering event that can trigger anxiety, depression, and significant stress. Mental health management is, therefore, a critical component of overall care. The relentless schedule of treatments, dietary restrictions, and fear of the future can be exhausting. Seeking support from therapists, counsellors, or social workers who specialise in chronic illness can provide powerful coping strategies. Additionally, connecting with others through kidney disease support groups (in-person or online) can reduce feelings of isolation and provide practical advice from those who truly understand the journey.
Lifestyle Modifications for Better Outcomes
Beyond diet, other lifestyle choices play a supportive role in management.
- Smoking Cessation: Smoking damages blood vessels, further reducing kidney blood flow and increasing cardiovascular risk—already high in ESRD patients. Quitting is one of the most beneficial actions you can take.
- Physical Activity: Regular, gentle exercise (as approved by your doctor) can help control blood pressure, improve mood, boost energy levels, and maintain muscle mass.
- Sleep Hygiene: Chronic illness is exhausting. Prioritising quality sleep helps the body repair itself and manage stress.
Building Your Healthcare Team
You are the CEO of your health, but you need a skilled executive team. This includes your nephrologist (kidney specialist), dialysis nurses, renal dietitian, transplant coordinator, pharmacist, and a primary care physician. Open, honest communication with every member of this team is essential for coordinated and effective care.
Conclusion
Kidney failure management is a lifelong commitment that requires diligence, education, and support. It's a challenging path, but it is one defined by empowerment, not limitation. By embracing the four pillars of treatment, diet, medication, and fluid control, and by prioritising your mental and emotional well-being, you can stabilise your condition and reclaim a sense of normalcy. Remember, you are not a passive patient but an active participant in your care. Ask questions, voice your concerns, and lean on your support network. With the right knowledge and tools, you can navigate this journey successfully and focus on living a full and meaningful life.
Consult a Nephrologist for Personalised Advice
Consult a Nephrologist for Personalised Advice
Dr Gayatri Pegu
Nephrologist
15 Years • MD (General Medicine) DM(Nephrology)
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
Dr Ch Sashidhar
Nephrologist
20 Years • MBBS, MD General Medicine, DNB, Nephrology
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad

Dr. Pardha Saradhi
Nephrologist
9 Years • MBBS, MD-DNB (Gen. Med.), DNB (Nephro)
Hyderabad
Apollo Hospitals D R D O kanchanbagh, Hyderabad
(75+ Patients)

Dr Praveen Kumar Etta
Nephrologist
10 Years • MBBS,MD DM(SGPGI) FORMER ASST(PIMS)
Hyderabad
Apollo Spectra Ameerpet, Hyderabad

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly
More articles from Kidney Failure
Frequently Asked Questions
Q1. What is the first sign of kidney failure that requires management?
- Often, the earliest signs are non-specific, like fatigue, nausea, and swelling in the ankles and feet. However, a significant change in urination patterns or severe shortness of breath requires immediate medical attention and signals the need to begin active management strategies.
Q2. Can you ever stop dialysis once you start?
- The need for dialysis is typically permanent unless you receive a successful kidney transplant. In very rare cases of acute kidney injury (which is different from chronic failure), kidney function may recover, allowing dialysis to be stopped. For ESRD, this is not the case.
Q3. How strict does my renal diet really need to be?
- Extremely strict. The renal diet is a medical treatment, not a casual suggestion. Deviating significantly can lead to dangerous electrolyte imbalances, fluid overload, and heart problems, often requiring emergency hospitalisation. Consistency is key to stability.
Q4. Is a kidney transplant a cure for kidney failure?
- A transplant is considered a treatment, not a complete cure. While it replaces failed kidney function and offers much greater freedom and longevity, recipients must take immunosuppressant drugs for life to prevent rejection, and these medications come with their own set of side effects and management needs.
Q5.How can I support a loved one undergoing kidney failure management?
- Educate yourself about their condition, offer to attend appointments, and help with meal prep according to their dietary restrictions. Most importantly, provide emotional support—listen without judgment and encourage them to seek out mental health resources or support groups. Practical help and emotional understanding are invaluable.