Reduce Knee Pain in Old Age: Expert Guide for Everyday Relief
Discover practical tips, exercises, diet, and self-care strategies to reduce knee pain in older adults. Learn home remedies, footwear advice, and when to seek medical help.


Introduction
Knee pain in old age is common—but it doesn’t have to control your day. Whether you’ve been told you have “wear and tear” knee osteoarthritis or you’re dealing with morning stiffness, swelling after walks, or pain climbing stairs, the right mix of simple changes can make a big difference. In this guide, you’ll learn what causes knee pain, proven home strategies to relieve it, and when to seek medical help. We’ll translate the latest evidence into step-by-step actions: targeted exercises, smart self-care, footwear and braces, diet and weight tips, and mind-body techniques that lessen pain. You’ll also see exactly how to navigate medications, injections, and surgery if needed—plus how to keep your home safer and your routine steadier. If symptoms persist beyond two weeks or you notice red flags, consult a doctor online with Apollo24|7 for further evaluation. Ready to take confident steps again? Let’s start with what’s happening inside your knee—and what you can do today.
Understanding Knee Pain in Old Age
Here's an overview of why knee pain occurs in older adults:
As we age, knee pain most often stems from osteoarthritis (OA)—a gradual loss of cartilage with changes to bone and surrounding tissues. Other common causes in older adults include degenerative meniscal tears, patellofemoral pain behind the kneecap, bursitis, tendinopathy, gout or pseudogout, and referred pain from the hip or spine. Knowing which patterns fit your pain helps guide the right home strategies.
Consult Top Specialists
Common Causes in Older Adults
• Osteoarthritis
• Degenerative meniscal tear
• Patellofemoral pain syndrome
• Bursitis/tendinopathy
• Gout/pseudogout
• Referred pain (hip/spine)
How Aging Changes the Knee
• Cartilage thins and loses elasticity, making the joint less forgiving
• Muscles (especially quadriceps and hip abductors) weaken, increasing joint load
• Joint fluid changes and low-grade inflammation increase stiffness
When to See a Doctor
• Sudden severe swelling, warmth, or fever
• Inability to bear weight after a fall
• Locking of the knee or true buckling
• Night pain that doesn’t improve with position changes
Consult a doctor online with Apollo24|7 if pain persists beyond two weeks or red flags appear.
Immediate Relief: Self-Care Basics
Here's how to manage flare-ups and support joint health:
Heat vs Ice and How to Use Each
• Ice for swelling or after long walks—10–15 minutes, 1–3 times daily
• Heat for stiffness and tight muscles—10–15 minutes before activity
• Some people alternate based on comfort and mobility
Over-the-Counter Options
• Topical NSAIDs (e.g., diclofenac gel) applied up to four times daily for OA pain
• Oral NSAIDs for short-term use, with caution in older adults
• Acetaminophen for mild pain, do not exceed recommended doses
• Topical capsaicin may help some people
Gentle Movement vs Rest
• Avoid prolonged bed rest; use relative rest by reducing, not stopping, activity
• Try 2–5 minutes of easy knee bends or short hallway walks every hour
• Increase activity gradually using the “10% rule” to avoid overload
Exercise Therapy That Works
Here's a structured approach to strengthen and mobilise your knees:
Strengthening (3 Nonconsecutive Days/Week)
• Quadriceps: sit-to-stand (12–15 reps x 2–3 sets), wall sits (15–45 sec x 2–3 sets)
• Hips: side-lying leg lifts or banded side steps (12–15 reps x 2–3 sets), bridges (10–12 reps x 2–3 sets)
• Calves: heel raises (12–15 reps x 2–3 sets)
Flexibility and Balance (Daily)
• Calf, hamstring, quadriceps stretches (30 sec x 2 each)
• Single-leg balance near a countertop (20–30 sec x 2–3 per leg)
• Gentle kneecap and ankle mobility drills
Low-Impact Cardio and a Weekly Plan
• Walking, cycling, or aquatic exercise 20–30 minutes, aiming for 150 min/week
• Tai Chi classes or video sessions 1–2 times weekly
Weekly Sample Plan
• Mon: Strength A + 10-min walk
• Tue: 20–30 min cycling or pool
• Wed: Flexibility + balance + 10-min walk
• Thu: Strength B + 10–15 min walk
• Fri: Tai Chi 20–30 min
• Sat: 20–30 min outdoor walk
• Sun: Restorative stretch + 10-min easy walk
Weight, Diet, and Supplements
Here's why load management matters:
Even a 5–10% weight loss can meaningfully reduce knee pain and improve function. Prioritise fat loss while preserving muscle, focusing on protein intake (1.0–1.2 g/kg/day) from fish, eggs, dairy, tofu, or legumes.
Nutrition tips:
• Emphasise vegetables, fruits, whole grains, legumes, nuts, olive oil, and fatty fish
• Ensure vitamin D sufficiency through diet or testing
Supplements:
• Turmeric/curcumin and omega-3s may provide modest benefit
• Glucosamine/chondroitin and collagen peptides have mixed evidence
Consult Top Specialists
Smart Gear: Footwear, Insoles, Braces, and Canes
Here's how to reduce knee load and improve stability:
Shoes and Insoles
• Supportive, cushioned shoes with slight rocker soles
• Orthotics may help with foot deformities or overpronation
Braces and Sleeves
• Unloader braces reduce load in compartmental OA
• Elastic knee sleeves provide warmth and proprioceptive feedback
Using a Cane Correctly
• Hold opposite to painful knee, elbow bent 15–20 degrees
• Use on longer walks or uneven terrain
Daily Movement and Home Safety
Here's how to protect knees while moving around your home:
Stairs, Sitting, and Getting Up
• “Good up, bad down” rule: lead with stronger leg going up, painful leg going down
• Slide to chair edge, feet shoulder-width, push through heels using glutes
Joint Protection During Chores
• Break tasks into short bouts with micro-rests
• Avoid deep knee bends; lift with hips, keep items close
Fall Prevention at Home
• Improve lighting, remove loose rugs, secure cords
• Install grab bars, handrails, and raised chairs
• Review medications and vision/hearing regularly
Medical Treatments: From Meds to Surgery
Here's a guide to professional interventions:
Diagnosis and Imaging
• History and physical exam first; X-rays confirm OA changes
• MRI only for suspected meniscal or ligament injuries
• Labs if gout, pseudogout, rheumatoid arthritis, or infection suspected
Injections
• Corticosteroids: short-term relief for flares
• Hyaluronic acid: evidence mixed, not routine
• PRP: emerging evidence, variable results
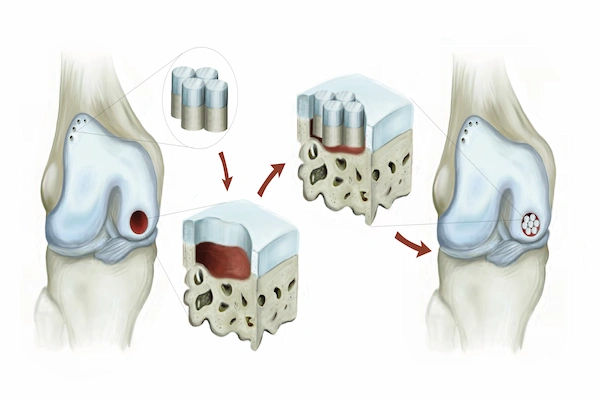
Surgery
• Arthroscopy usually not recommended for degenerative OA
• Total knee replacement for end-stage OA if conservative care fails
• Prehab and shared decision-making improve outcomes
Mind-Body, Sleep, and Pacing
Here's how lifestyle affects pain perception:
Sleep
• 7–8 hours, consistent schedule, cool/dark room
• Knee pillow or towel for support
Stress, CBT, and Mindfulness
• Reframe negative thoughts, use relaxation and breathing exercises
Pacing and Flare Management
• Spread activities throughout the day, follow “10% rule” for increases
• Use heat/ice during flares
Putting It All Together: A 6-Week Plan
Week 1–2: Calm and prime
• Heat in the morning, ice after walks
• Topical NSAIDs for flares
• Daily 10-min walk + flexibility/balance
• Strength A twice weekly
• Home safety tweaks
• Track pain and function
Week 3–4: Build
• Add Strength B
• Extend walks/cycling to 20–25 min
• Tai Chi 1–2 times weekly
• Consider cane for longer walks
• Improve diet quality, check vitamin D
Week 5–6: Progress and Personalise
• Increase strength intensity
• Add hill/stair session with hip mechanics
• Trial knee sleeve if needed
• Consult doctor if pain remains high
By six weeks, many notice easier sit-to-stands, better stair confidence, and less overall knee pain. Maintain habits that work; they compound over time.Consult Top Specialists
Conclusion
Knee pain in old age can feel discouraging, but it is highly manageable. The most effective relief comes from consistent, small actions—strengthening your hips and thighs, keeping joints moving, choosing supportive footwear, and pacing activity to avoid flares. Pair these with smart self-care such as heat, ice, and topical NSAIDs, along with better sleep and stress management to calm the nervous system’s pain signals. Nutrition and modest weight loss further reduce joint load, while devices like canes or braces offer immediate support when needed.
If progress stalls, your clinician may recommend options such as injections and, only if necessary, surgery. Using a structured six-week plan helps you track what works and build confidence step by step. Even with “old” knees, improvement is very possible. With the right approach, you can walk further, climb stairs with less strain, and return to the activities you enjoy. If symptoms persist despite these measures, book a physical visit to a doctor with Apollo24|7.
Consult Top Specialists

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Prof. Dr. Jambu N
Orthopaedician
23 Years • MBBS, M.S Ortho, FRCS ,FACS
Chennai
Apollo Speciality Hospitals Vanagaram, Chennai
(150+ Patients)
Consult Top Specialists

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Prof. Dr. Jambu N
Orthopaedician
23 Years • MBBS, M.S Ortho, FRCS ,FACS
Chennai
Apollo Speciality Hospitals Vanagaram, Chennai
(150+ Patients)
Consult Top Specialists

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Prof. Dr. Jambu N
Orthopaedician
23 Years • MBBS, M.S Ortho, FRCS ,FACS
Chennai
Apollo Speciality Hospitals Vanagaram, Chennai
(150+ Patients)
More articles from Knee pain
Frequently Asked Questions
1) What are the best exercises for knee pain in seniors?
Start with sit-to-stands, wall sits, bridges, side steps, and heel raises, along with daily flexibility and balance exercises. Add low-impact cardio such as walking, cycling, or aquatic exercise.
2) Is walking good for knee pain in older adults?
Yes—regular, comfortable-paced walking can reduce pain and stiffness. Increase gradually by no more than 10% per week to avoid flare-ups.
3) Should I use heat or ice for knee pain?
Use ice for swelling or after long walks, and heat before activity to relieve stiffness. Some people find alternating both helps; choose whichever improves comfort and motion.
4) Do knee braces or sleeves help?
Unloader braces can relieve pain in compartmental osteoarthritis by shifting load, while elastic sleeves provide warmth and confidence. They are most effective when combined with exercise and weight management.
5) Are hyaluronic acid injections effective for knee osteoarthritis?
Evidence is mixed. Corticosteroid injections may offer short-term relief during flares, but routine hyaluronic acid use is generally not recommended. Discuss with your clinician whether you are a suitable candidate.