All About Alcohol-Related Liver Disease (ARLD)
Learn about Alcohol-Related Liver Disease (ARLD), its causes, symptoms, stages, diagnosis, and treatment. Discover ways to prevent liver damage from excessive alcohol consumption.

Written by
Last updated on 3rd Jul, 2025
Introduction
Alcohol-Related Liver Disease (ARLD) is a condition that affects millions of people worldwide. It refers to a range of liver problems caused by excessive and long-term alcohol consumption. While moderate drinking may not pose a significant risk to liver health, heavy drinking over time can lead to serious liver damage, including fatty liver disease, cirrhosis, and even liver failure. Understanding ARLD, its causes, symptoms, and treatment options is essential for anyone concerned about their liver health. In this article, we will explore the causes of ARLD, its stages, diagnosis, and the steps you can take to manage and prevent the disease.
What Is Alcohol-Related Liver Disease (ARLD)?
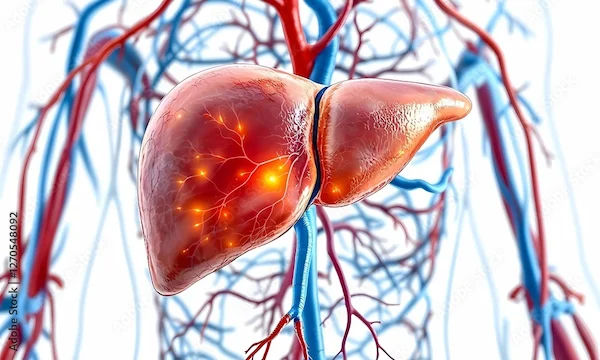
Alcohol-Related Liver Disease refers to liver damage caused by excessive alcohol consumption. The liver is a vital organ responsible for filtering toxins from the blood, producing proteins, and storing energy. Drinking alcohol in large amounts over a long period can overwhelm the liver, leading to inflammation, fat buildup, and eventually scarring or cirrhosis.
The liver is capable of repairing itself to some extent. However, prolonged heavy drinking can lead to irreversible damage. The severity of ARLD can range from fatty liver disease (a relatively mild condition) to cirrhosis (a more severe, irreversible scarring of the liver tissue) and liver failure.
What Causes Alcohol-Related Liver Disease?
The liver is responsible for breaking down and processing alcohol, but when alcohol is consumed in excess, it can damage liver cells. The key causes of ARLD include:
Excessive Alcohol Consumption: Drinking large amounts of alcohol regularly over time is the primary cause of ARLD. The more you drink, the greater the risk of developing liver problems.
Heavy drinking is defined as more than 14 drinks per week for men or more than 7 drinks per week for women, according to health guidelines.
Binge drinking, where large quantities of alcohol are consumed in a short period (defined as 5 or more drinks in 2 hours for men, or 4 or more drinks for women), also increases the risk of liver damage.
Alcohol Metabolism: When alcohol is consumed, the liver metabolises it into acetaldehyde, a toxic substance that can damage liver cells. Chronic heavy drinking leads to a buildup of acetaldehyde, contributing to liver inflammation and damage.
Genetic Factors: Some people may be more genetically predisposed to liver damage from alcohol. Certain genetic variations can make it harder for the liver to process alcohol and its byproducts, increasing the risk of ARLD.
Gender: Women tend to develop ARLD more quickly than men due to differences in alcohol metabolism and hormonal factors. Even moderate alcohol intake can pose a higher risk for women.
Underlying Health Conditions: Conditions such as obesity, diabetes, or viral hepatitis can increase the risk of developing ARLD. These conditions can make the liver more vulnerable to alcohol-induced damage.
Stages of Alcohol-Related Liver Disease
ARLD develops in stages, with each stage representing a more severe level of liver damage. These stages include:
Alcoholic Fatty Liver Disease (AFLD):
This is the earliest stage of ARLD and occurs when fat begins to accumulate in the liver cells due to excessive alcohol consumption. It can develop after just a few days of heavy drinking.
Symptoms: Most people with AFLD experience no symptoms, but some may experience mild fatigue, abdominal discomfort, or a sense of fullness.
Prognosis: In many cases, if alcohol consumption is reduced or stopped, the liver can recover, and the fat buildup will decrease.
Alcoholic Hepatitis:
Prolonged heavy drinking can lead to inflammation of the liver, known as alcoholic hepatitis. This is a more serious stage of ARLD and can lead to liver damage.
Symptoms: Symptoms of alcoholic hepatitis include nausea, vomiting, abdominal pain, fever, jaundice (yellowing of the skin and eyes), and fatigue. In severe cases, it can lead to liver failure.
Prognosis: If alcohol consumption is stopped, some liver function may improve, but the condition can also progress to cirrhosis if left untreated.
Cirrhosis:
Cirrhosis is the final stage of ARLD, characterised by severe scarring of the liver tissue. The liver becomes unable to function properly, leading to complications such as liver failure.
Symptoms: Symptoms of cirrhosis include severe fatigue, easy bruising, swelling in the abdomen (ascites), varicose veins in the oesophagus, and confusion (hepatic encephalopathy). Jaundice and bleeding can also occur.
Prognosis: Cirrhosis is irreversible, but with proper medical care and lifestyle changes (such as stopping alcohol consumption), some complications can be managed. In severe cases, a liver transplant may be required.
Liver Failure:
Liver failure occurs when the liver is no longer able to perform its essential functions, such as detoxifying the blood and producing vital proteins. This is a life-threatening condition.
Symptoms: Symptoms include confusion, swelling in the legs and abdomen, severe jaundice, and bleeding.
Prognosis: Liver failure often requires a liver transplant to save the patient’s life.
Symptoms of Alcohol-Related Liver Disease
In the early stages of ARLD, symptoms may be subtle or absent. However, as the disease progresses, symptoms become more noticeable. Common signs of ARLD include:
Fatigue and weakness
Unexplained weight loss
Nausea and vomiting
Abdominal pain or discomfort (especially in the upper right side)
Swelling in the abdomen (ascites) or legs
Jaundice (yellowing of the skin and eyes)
Dark urine or pale stools
Itchy skin
Easy bruising or bleeding
Diagnosis of Alcohol-Related Liver Disease
If you are concerned about your liver health or suspect ARLD, a healthcare provider will perform a thorough evaluation. This may include:
Medical History: Your doctor will ask about your alcohol consumption, family history of liver disease, and other risk factors.
Physical Exam: Your doctor will check for signs of liver damage, such as jaundice, abdominal tenderness, or swelling.
Blood Tests: Liver function tests (LFTs) are commonly used to assess liver health. Elevated levels of liver enzymes (such as ALT and AST) may indicate liver damage.
Imaging: Ultrasound, CT scans, or MRIs may be used to assess the liver’s size, shape, and presence of fatty tissue or scarring.
Liver Biopsy: In some cases, a biopsy may be performed to confirm the extent of liver damage and identify the stage of ARLD.
Get Your Liver Health Checked
Treatment and Management of Alcohol-Related Liver Disease
While the liver has a remarkable ability to regenerate, severe liver damage from ARLD cannot be undone. However, with early intervention and lifestyle changes, the progression of ARLD can be slowed or even reversed in its early stages.
Stop Drinking Alcohol: The most important step in managing ARLD is to stop drinking alcohol entirely. This can help prevent further liver damage and may allow the liver to heal, especially in the early stages of the disease.
Diet and Nutrition:
A healthy, balanced diet is essential for liver health. Focus on eating fruits, vegetables, whole grains, lean proteins, and healthy fats. Avoid excessive salt, sugar, and processed foods.
Adequate hydration is important, so drink plenty of water to support liver function.
Exercise: Regular physical activity can help maintain a healthy weight and improve liver function. Aim for at least 30 minutes of moderate exercise most days of the week.
Medications: In cases of alcoholic hepatitis, medications such as corticosteroids may be prescribed to reduce inflammation. For those with cirrhosis or liver failure, specific medications may be used to manage complications.
Liver Transplant: In cases of severe cirrhosis or liver failure, a liver transplant may be the only option for survival.
Prevention of Alcohol-Related Liver Disease
The best way to prevent ARLD is to avoid excessive alcohol consumption. Here are some steps you can take to reduce your risk:
Follow Recommended Drinking Guidelines: Limit alcohol consumption to no more than one drink per day for women and two drinks per day for men.
Take Breaks from Alcohol: Avoid drinking every day and take regular breaks from alcohol consumption to give your liver time to recover.
Monitor Your Health: Regularly check in with your healthcare provider, especially if you have a history of heavy drinking or liver disease.
Manage Other Health Conditions: Conditions like obesity, diabetes, and hepatitis can increase the risk of ARLD. Work with your healthcare provider to manage these conditions.
Conclusion
Alcohol-Related Liver Disease (ARLD) is a serious condition that can happen when you drink too much alcohol for a long time. It's important to know what causes it, how it develops, the symptoms to watch for, and how to treat it. By making healthier choices and getting the right medical help, you can lower your risk of ARLD and keep your liver healthy. Remember, the liver is a resilient organ, and with the right steps, it is possible to halt the progression of ARLD and lead a healthier, more fulfilling life.
Consult Top Hepatologists
Consult Top Hepatologists

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(125+ Patients)

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(100+ Patients)

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(125+ Patients)

Dr U V U Vamsidhar Reddy
Hepatologist
10 Years • MBBS, MD (JIPMER), DM (Hepatology, PGIMER)
Chennai
Apollo Hospitals Greams Road, Chennai
(100+ Patients)