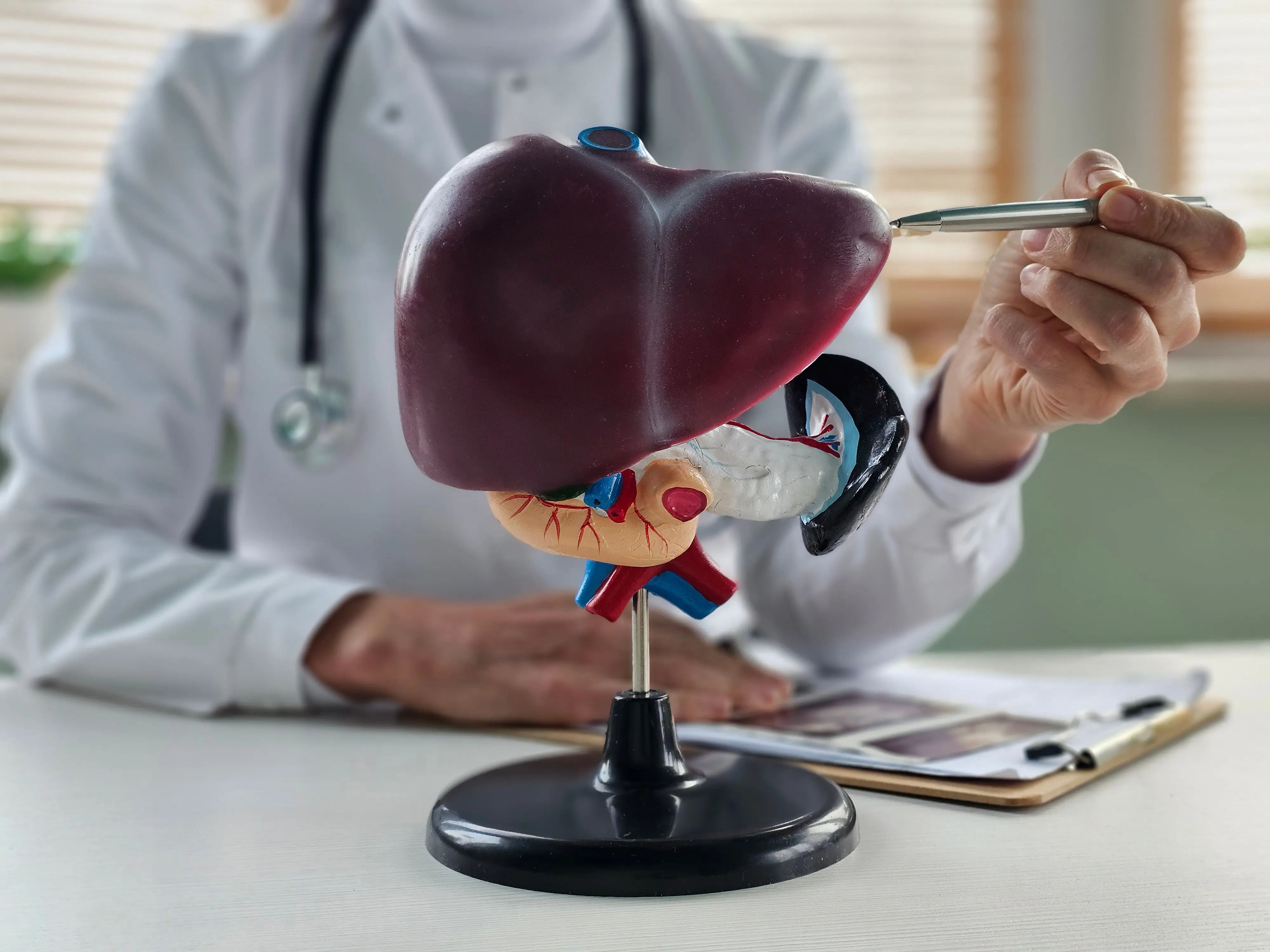
Liver Transplant Complications: Understanding the Risks and How to Manage Them
Learn about liver transplant complications, including organ rejection, infections, and blood clots. Discover how to manage risks and improve recovery for long-term health.

Written by
Last updated on 13th Jan, 2026
Introduction
A liver transplant can offer new hope for people with severe liver conditions like cirrhosis, acute liver failure, or liver cancer. While it is often a life-saving procedure, it comes with challenges, including the risk of complications during recovery. Understanding these risks, how to manage them, and what steps you can take to reduce them is crucial for a smooth recovery and long-term health. By staying informed and proactive, you can significantly improve your chances of a successful outcome after your transplant.
In this article, we will walk you through the most common and serious complications following a liver transplant. We’ll also discuss how they can be managed and provide tips on how to enhance your recovery and quality of life.
Common Liver Transplant Complications
Although liver transplants are generally successful, complications can still arise. These may occur soon after surgery or develop later in the recovery process. Here are some of the most common complications:
1. Organ Rejection
After a liver transplant, your immune system may recognise the new liver as a foreign object and try to reject it. This is a normal immune response, but it can threaten the success of the transplant.
Types of Rejection:
Acute Rejection: Occurs within the first few months after surgery. It can cause symptoms like fever, jaundice (yellowing of the skin and eyes), and dark urine.
Chronic Rejection: Develops slowly, sometimes years after the transplant, leading to long-term liver damage.
Symptoms of Rejection may include:
Fever
Jaundice
Dark urine
Stomach pain
Itching
How to Manage Rejection: To prevent and treat rejection, you'll need to take medications that suppress your immune system (immunosuppressants). These medications help prevent rejection by lowering your immune system, but it's important to get the right dose. If the dose is too low, your body may reject the liver. If it's too high, you may get more infections. Regular check-ups and blood tests help your doctor adjust the treatment.
2. Infections
The immunosuppressive medications you take to prevent rejection also make you more vulnerable to infections. The surgical procedure itself can also introduce bacteria into the body, increasing the risk of infection.
Types of Infections:
Bacterial (e.g., pneumonia, urinary tract infections)
Viral (e.g., cytomegalovirus or CMV)
Fungal (e.g., candidiasis)
Symptoms of Infection may include:
Fever
Fatigue
Cough or difficulty breathing
Pain when urinating
Redness or swelling at the surgical site
How to Prevent and Manage Infections: Doctors will often prescribe antibiotics, antifungal, and antiviral medications as a precaution, particularly in the early stages of recovery. Good hygiene practices—like frequent hand-washing and avoiding sick people—are crucial. If you suspect an infection, it's important to get medical help right away. Early treatment can prevent more serious complications.
3. Bleeding and Blood Clots
Liver transplant surgery is complex, and bleeding can happen during or after the procedure. As your body heals, blood clots may form, which can affect blood flow and the function of your new liver. Your medical team will monitor you closely to manage these risks and adjust treatment as needed.
Symptoms of Bleeding may include:
Low blood pressure
Rapid heartbeat
Swelling or bruising
Blood in stools or vomit
Symptoms of Blood Clots include:
Pain, swelling, or redness in the arms or legs
Shortness of breath
Chest pain
How to Manage Bleeding and Blood Clots: If bleeding occurs, treatments like blood transfusions or additional surgery may be required. Blood thinners may also be prescribed to help prevent blood clots. Your healthcare team will monitor your condition closely to catch and treat any complications early.
4. Primary Graft Non-Function (PNF)
In rare cases, the transplanted liver may not function properly right away. This is called Primary Graft Non-Function (PNF) and is a serious complication that requires immediate attention.
Symptoms of PNF may include:
Jaundice
Abnormal blood clotting
Electrolyte imbalances
How to Manage PNF: If PNF occurs, you may need another transplant. Close monitoring in the days and weeks after surgery is essential to identify issues early.
5. Graft Dysfunction
Graft dysfunction happens when the transplanted liver isn’t working properly. This can be caused by factors like infection, rejection, or issues with blood flow or bile duct function. Early detection and treatment are key to improving the chances of a positive outcome.
Signs of graft dysfunction:
Jaundice
Dark urine or pale stools
Abdominal swelling or discomfort
Decreased liver function (identified in lab tests)
Prevention and Management :
Regular Monitoring: Regular blood tests, ultrasounds, and other imaging studies are used to monitor liver function and detect any signs of graft dysfunction early.
Medications: Adjusting the immunosuppressive drugs or using additional medications may help address graft dysfunction.
Treatment of Underlying Causes: If infection or bile duct issues are contributing to graft dysfunction, treatment will be tailored accordingly.
How to Improve Recovery and Minimise Risks After a Liver Transplant?
Recovering from a liver transplant can take time and effort, but there are several steps you can take to help speed up your recovery and lower your chances of complications:
Follow Your Medication Plan
Taking your medications exactly as your doctor prescribes is crucial for preventing organ rejection and managing infections. Be sure to follow your doctor's instructions closely and never skip doses.
Keep Up with Regular Check-Ups
It's important to stay on top of your follow-up appointments so your healthcare team can monitor your liver function and catch any potential problems early. These visits play a big role in your long-term health.
Eat a Healthy, Balanced Diet
A nutritious diet helps your liver heal and supports overall recovery. Focus on eating plenty of fruits, vegetables, lean proteins, and whole grains. Be sure to avoid alcohol, as it can damage your new liver. Your doctor may have specific dietary guidelines for you, so be sure to follow those.
Stay Active, but Listen to Your Body
Physical activity is important for your recovery, but it's essential to start slowly. Begin with light activities, like walking, and gradually increase your activity level as you regain strength. Always check with your doctor before starting new exercises.
Drink Plenty of Water
Staying hydrated is key for kidney function and overall health. Try to drink lots of water and avoid sugary drinks, caffeine, and alcohol to keep your body in good shape.
Practice Good Hygiene to Prevent Infections
Washing your hands often and keeping your environment clean is essential to reducing the risk of infection. Avoid large crowds and follow any preventive treatments your doctor suggests.
Watch for Signs of Rejection or Infection
Pay attention to any changes in your body, like fever, jaundice (yellowing of your skin or eyes), tiredness, or pain. If you notice anything unusual, contact your healthcare provider right away.
Take Care of Your Emotional Well-Being
Recovery can be emotionally tough, so it’s important to take time for relaxation and self-care. Lean on your family and friends for support, and if needed, consider joining a transplant support group or talking to a professional counsellor.
Quit Smoking and Manage Stress
If you smoke, quitting is crucial for your recovery. Smoking can harm your liver and increase the risk of complications. Managing stress is also key to staying healthy—try relaxation techniques like mindfulness, deep breathing, or yoga to help you stay calm and positive.
Conclusion
A liver transplant is a complex and life-saving procedure with the potential for various complications. Understanding these complications and their management is crucial for transplant recipients and their families. Through regular monitoring, adherence to immunosuppressive therapy, a healthy lifestyle, and emotional support, patients can navigate the challenges of the post-transplant journey and achieve a better quality of life.
If you or a loved one is undergoing a liver transplant, it is essential to work closely with the healthcare team, follow their recommendations, and stay informed about potential complications and their management. With proper care and support, the journey to recovery and a healthier life is possible.
Consult Top Transplant Hepatologists
Consult Top Transplant Hepatologists

Dr. Srinivasa Reddy
Hepatologist
12 Years • MBBS, MD (General Medicine), DM (Hepatology),ASGE
Hyderabad
Myra Liver & Gastro Care, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr U V U Vamsidhar Reddy
Hepatologist
10 Years • MBBS, MD (JIPMER), DM (Hepatology, PGIMER)
Chennai
Apollo Hospitals Greams Road, Chennai
(75+ Patients)