What Leads To Signs Of Hepatomegaly?
Hepatomegaly, or an enlarged liver, can be a sign of underlying disease. Learn about the common causes like fatty liver, heart failure, and cancer, plus the key symptoms and treatment options.


Introduction
If you’ve been told you have hepatomegaly—medical shorthand for an enlarged liver—you probably have questions. Is it serious? What causes it? How do doctors find out why it’s happening, and what can you do next? Hepatomegaly isn’t a disease by itself. Instead, it’s a clue: your liver is larger than expected, and your body may be signaling conditions ranging from fatty liver and viral hepatitis to heart issues or problems with bile flow. Sometimes, hepatomegaly is silent; other times, it brings symptoms like right upper abdominal fullness, fatigue, or jaundice.
In this guide, written for the general public, we’ll explain what hepatomegaly is, the common signs and symptoms, how it’s diagnosed, and what usually causes it in adults and children. We’ll also cover what your test results may mean, the most effective treatments, and practical steps you can take today to protect your liver. If your symptoms are persistent or worrying, we’ll highlight when to seek urgent care and how to get timely help. By the end, you’ll understand the key drivers behind the signs of hepatomegaly—and the path to feeling better.
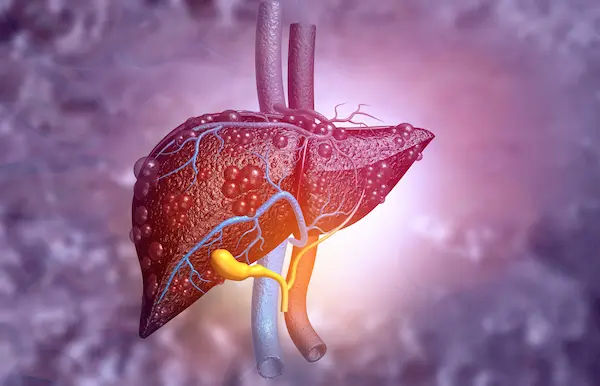
What Is Hepatomegaly?
Simple definition: hepatomegaly vs “enlarged liver”
• Hepatomegaly means the liver is bigger than normal. Doctors use “enlarged liver” interchangeably, but hepatomegaly is the precise medical term. It’s not a diagnosis; it’s a finding that needs context—your symptoms, lab tests, and imaging—to figure out the underlying cause .Many people with hepatomegaly have no symptoms, especially in early stages of fatty liver disease.
How big is “big”? Exam and imaging thresholds
• On a physical exam, clinicians gently press under the right ribcage, feeling for the liver edge. A soft, smooth edge a centimeter or two below the ribs can be normal in thin individuals, but a firm or markedly descended liver often suggests hepatomegaly. Percussion (tapping) helps estimate liver span. Imaging is more precise: ultrasound is typically first-line. A common reference is a craniocaudal liver measurement over about 15–16 cm in the midclavicular line, though normal ranges vary by body size and sex [8]. Radiologists also look at lobe proportions, contour, and echotexture, which can hint at fatty liver, congestion, or mass lesions.
Hepatomegaly vs fatty liver vs hepatosplenomegaly (what’s the difference?)
• Fatty liver (hepatic steatosis) refers to fat buildup in liver cells; it may or may not cause hepatomegaly. Many people have fatty liver without an enlarged liver.
• Hepatomegaly refers strictly to size and can happen with fatty liver, hepatitis, heart failure, tumors, or storage diseases.
• Hepatosplenomegaly means both the liver and spleen are enlarged—often seen with chronic liver disease and portal hypertension, certain infections, hematologic disorders, or infiltrative conditions.Consult a Top General Physician
Why Hepatomegaly Matters?
What an enlarged liver can signal about your health?
The liver is a busy hub for metabolism, detoxification, bile production, and immune function. Hepatomegaly can indicate:
• Fat accumulation (non-alcoholic or alcohol-related)
• Inflammation from viruses, autoimmune disease, or toxins
• Congestion from heart failure (blood backs up to the liver)
• Blocked bile outflow (cholestatic liver disease)
• Infiltrative/metabolic storage conditions (iron, copper, glycogen)
• Tumors, either primary liver cancers or metastases
• In short, hepatomegaly is your alert to look deeper. Addressing the root cause early often prevents progression.
Potential complications if ignored (fibrosis, cirrhosis, cancer)
Prolonged injury can scar the liver (fibrosis), which may advance to cirrhosis (severe scarring). Cirrhosis elevates the risk of portal hypertension, ascites (fluid in the belly), variceal bleeding, hepatic encephalopathy, and liver cancer (hepatocellular carcinoma). Timely evaluation of hepatomegaly can interrupt this path and improve long-term outcomes
Signs and Symptoms of Hepatomegaly
Early, subtle signs
• Many people with hepatomegaly have no symptoms. When present, early signs include:
• Right upper quadrant fullness, pressure, or mild pain
• Bloating or early satiety (feeling full quickly)
• Fatigue and low energy
• Mildly abnormal liver function tests noted on routine screening
Red flags that need urgent care
• Seek urgent evaluation for:
• Jaundice (yellow eyes/skin), dark urine, pale stools
• Severe or persistent right upper abdominal pain
• High fever, confusion, severe nausea/vomiting
• Swelling of legs/abdomen (ascites), sudden weight gain from fluid
• Bleeding/bruising easily, black or bloody stools
• Mental status changes or extreme sleepiness (possible encephalopathy)
These signs can reflect acute hepatitis, biliary obstruction, severe infection, or decompensated cirrhosis. If you notice these, consider emergency care; if symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation.
Hepatomegaly with splenomegaly: what it suggests
An enlarged spleen with hepatomegaly points toward portal hypertension from chronic liver disease, certain infections (like mononucleosis), blood disorders (hemolytic anemia), or infiltrative diseases. It changes the differential diagnosis and often prompts additional tests (e.g., viral panels, blood films).
Major Causes of Hepatomegaly in Adults
Fatty liver disease (NAFLD/NASH) and alcohol-related liver disease
• Non-alcoholic fatty liver disease (NAFLD) affects roughly one in four adults globally, driven by obesity, type 2 diabetes, and metabolic syndrome. A subset develops inflammation and scarring (NASH), which raises the risk of cirrhosis and hepatocellular carcinoma. Alcohol-related liver disease similarly ranges from fatty change to hepatitis and cirrhosis. Either can cause hepatomegaly and mild to moderate right upper quadrant discomfort [1][6]. Long-tail keyword: signs of fatty liver and hepatomegaly.
Unique insight: Even 5–7% weight loss can significantly reduce liver fat; 7–10% weight loss can improve NASH histology. Focusing on sustainable lifestyle changes often reverses hepatomegaly from fatty causes.
Viral hepatitis (A, B, C) and autoimmune hepatitis
• Acute viral hepatitis can present with hepatomegaly, jaundice, dark urine, and fatigue. Chronic hepatitis B and C may be silent for years, with hepatomegaly discovered incidentally. Autoimmune hepatitis can cause fatigue, joint pain, and fluctuating LFTs; early treatment prevents progression.
Congestive hepatomegaly from heart failure
• Right-sided heart failure or constrictive pericarditis can cause blood to back up into the liver, leading to tender hepatomegaly (“congestive hepatomegaly”). Clues include leg swelling, shortness of breath, and jugular venous distention. Treating the heart condition often improves the liver findings [5]. Long-tail keyword: congestive hepatomegaly.
Blocked bile flow (PBC, PSC), tumors, and metastases
• Cholestatic conditions—primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC)—cause impaired bile flow, itching, jaundice, and hepatomegaly. Liver tumors (primary or metastatic) can enlarge the liver; alarm features include weight loss, persistent pain, and markedly elevated alkaline phosphatase with focal lesions on imaging [1][5][6].
Metabolic/infiltrative causes (hemochromatosis, Wilson disease, amyloidosis)
• Hemochromatosis (iron overload): can cause fatigue, joint pain, diabetes, skin darkening, and hepatomegaly. Phlebotomy is highly effective when started early.
• Wilson disease (copper overload): often in younger patients; neuropsychiatric features, Kayser–Fleischer rings, and hepatomegaly. Chelation therapy can prevent progression.
• Amyloidosis, sarcoidosis, and glycogen storage diseases also enlarge the liver by infiltration or storage.
Medications, toxins, and supplements
• Certain drugs (e.g., amiodarone, methotrexate), high-dose vitamin A, anabolic steroids, and some herbal supplements can cause hepatomegaly via fatty change, inflammation, or cholestasis. Always inform your clinician about over-the-counter and herbal products.
Hepatomegaly in Children: How Do Causes Differ?
Infections, storage/metabolic disorders, biliary atresia
In children, hepatomegaly often reflects infections (hepatitis viruses, EBV), metabolic/storage diseases (glycogen storage disease, lysosomal storage disorders), or cholestatic conditions like biliary atresia (a neonatal surgical emergency). Early detection is crucial; pale stools, dark urine, and prolonged jaundice in infants need urgent evaluation
Growth, feeding, and developmental clues
Pediatric clues include poor weight gain, feeding difficulties, developmental delays, or recurrent infections. Screening may include newborn panels, metabolic testing, and specialized imaging.
When to see a pediatric specialist?
If a child has persistent jaundice, failure to thrive, abdominal swelling, or unexplained fatigue, seek pediatric evaluation promptly. A pediatric hepatologist may coordinate metabolic and genetic testing alongside imaging and labs.
How Doctors Diagnose Hepatomegaly?
What happens during the physical exam?
Expect a focused exam: doctors assess body weight, signs of chronic liver disease (spider angiomas, palmar erythema), fluid accumulation (ascites), and tenderness. They’ll palpate below the right ribs and may also feel for spleen enlargement on the left side. This clinical context narrows the differential.
Blood tests that matter (LFTs, viral markers, iron/copper tests)
Common labs include:
• Liver function tests: AST, ALT, ALP, GGT, bilirubin, albumin, INR
• Complete blood count (CBC) for anemia/platelets
• Viral hepatitis panels (HBsAg, anti-HCV, etc.)
• Iron studies (ferritin, transferrin saturation) for hemochromatosis
• Ceruloplasmin/urinary copper for Wilson disease
• Autoimmune markers (ANA, SMA, AMA, IgG)
• Metabolic screening as indicated
Apollo 24|7 offers convenient home collection for tests like liver function tests and viral hepatitis screening, which can speed up diagnosis.
Imaging: ultrasound first, then CT/MRI as needed
Ultrasound confirms hepatomegaly and can show steatosis, biliary dilation, vascular flow, and masses. If needed, CT or MRI further characterizes lesions, assesses vasculature, and distinguishes fat from fibrosis or tumor. Ultrasound elastography estimates liver stiffness (a surrogate for fibrosis).
Elastography and biopsy: when and why
Elastography helps risk-stratify patients with fatty liver or chronic hepatitis. Liver biopsy is reserved for unclear diagnoses, suspected autoimmune hepatitis/NASH activity, or staging fibrosis when it will change management.
A sample diagnostic pathway
• Step 1: History/exam (alcohol, meds/supplements, metabolic risks, family history)
• Step 2: Initial labs (LFTs, CBC, INR, viral hepatitis tests)
• Step 3: Ultrasound with Doppler; consider elastography in NAFLD/hepatitis
• Step 4: Targeted tests (iron/copper/autoimmune) based on pattern
• Step 5: CT/MRI for masses or complex cases
• Step 6: Biopsy if diagnosis remains uncertain or to stage disease severity
If your condition does not improve after initial steps or results are confusing, consult a doctor online with Apollo 24|7 for personalized guidance, and book home sample collection for follow-up tests.
Understanding Your Results
Hepatocellular vs cholestatic patterns
• Hepatocellular pattern: higher AST/ALT; think viral hepatitis, NAFLD/NASH, toxins, autoimmune hepatitis.
• Cholestatic pattern: higher ALP/GGT and bilirubin; think bile duct problems (stones, PBC/PSC), infiltrative disease, or mass compression.
• Albumin and INR reflect liver synthetic function; low albumin or high INR suggest advanced disease.
Tumor markers and what they can/can’t tell you
• Alpha-fetoprotein (AFP) can rise in hepatocellular carcinoma, but normal AFP doesn’t rule it out. CA 19-9 may be elevated in cholangiocarcinoma. Imaging remains central to cancer diagnosis; markers are supportive, not definitive.
Putting it together with symptoms and imaging
• Your clinician triangulates symptoms (e.g., pruritus + pale stools), labs (cholestatic vs hepatocellular), and imaging (duct dilation, masses, fatty change). For example, hepatomegaly with fatty echotexture and metabolic risk factors points to NAFLD; tender hepatomegaly with leg swelling and echocardiographic changes suggests congestive hepatomegaly.
Treatment and Management: Matching the Cause
Lifestyle therapy for fatty liver and alcohol-related disease
• Weight loss: Aim for 7–10% reduction to improve NASH; 5–7% reduces steatosis.
• Diet: Mediterranean-style eating pattern; limit sugary beverages and ultra-processed foods.
• Activity: At least 150 minutes/week of moderate exercise plus resistance training.
• Alcohol: If alcohol-related hepatomegaly, complete abstinence is key; even in NAFLD, minimize alcohol intake.
Long-tail keyword: hepatomegaly treatment at home.
Antivirals, immunosuppression, and chelation/phlebotomy
• Hepatitis B/C: Modern antivirals can suppress HBV and cure HCV in most cases, improving inflammation and size over time.
• Autoimmune hepatitis: Corticosteroids and azathioprine can normalize LFTs and reduce hepatomegaly.
• Hemochromatosis: Therapeutic phlebotomy removes excess iron.
• Wilson disease: Chelation (penicillamine or trientine) or zinc therapy reduces copper burden.
Managing heart failure and cholestasis
• Congestive hepatomegaly: Optimize heart failure therapy (diuretics, guideline-directed medications), which reduces liver congestion.
• Cholestatic disease (PBC/PSC): Ursodeoxycholic acid and, in select cases, obeticholic acid for PBC; manage complications and consider transplant evaluation if advanced.
When is surgery, oncology, or transplant is considered?
• Hepatocellular carcinoma or large benign tumors may need ablation, resection, or transplantation. Advanced cirrhosis and refractory complications prompt liver transplant referral. A multidisciplinary team (hepatology, interventional radiology, oncology) tailors the approach.
If you’re navigating these options, book a physical visit to a doctor with Apollo 24|7 to review reports and decide next steps.
Prevention, Monitoring, and When to Seek Care?
Diet, activity, and vaccine strategies
• Dietary pattern: Emphasize vegetables, fruits, legumes, whole grains, nuts, and fish; limit refined carbs and saturated fats.
• Exercise: Start with brisk walking, build to 150–300 minutes/week.
• Vaccines: Hepatitis A and B vaccines help protect the vulnerable liver.
• Safe meds: Avoid unnecessary supplements; check doses of acetaminophen and avoid combining it with alcohol.
How often to recheck labs and imaging?
• Fatty liver with mild abnormalities: recheck LFTs every 3–6 months during lifestyle changes; elastography yearly if risk factors persist.
• Chronic hepatitis: periodic viral loads and fibrosis assessments per guidelines.
• Cirrhosis or high risk: ultrasound every 6 months for HCC surveillance
Emergency signs vs routine follow-up
• Emergency: new jaundice, confusion, severe pain, vomiting blood, black stools, high fever—seek urgent care.
• Routine: stable mild symptoms with improving labs—continue lifestyle measures and scheduled monitoring.
Getting help online or at home (tests and telehealth)
If symptoms persist beyond two weeks or new concerns arise, consult a doctor online with Apollo 24|7 for further evaluation. Apollo 24|7 also offers home collection for tests like liver function tests, hepatitis panels, ferritin, transferrin saturation, and ultrasound referrals—making follow-up more convenient.
Conclusion
Hepatomegaly—an enlarged liver—can feel like an intimidating finding, but it’s best understood as a helpful signal. It tells you and your care team to look beneath the surface for causes ranging from fatty liver and viral hepatitis to heart-related congestion or issues with bile flow. Most of the time, a structured approach—history and physical exam, targeted blood tests, and ultrasound—quickly clarifies the likely cause. From there, treatment can be highly effective: lifestyle changes for fatty liver, antivirals for hepatitis, phlebotomy or chelation for iron or copper overload, heart failure optimization, and specialist care for cholestasis or tumors.
Pay attention to red flags such as jaundice, confusion, or severe pain, and seek urgent care if these occur. Otherwise, steady, sustainable improvements in diet, weight, and activity, coupled with routine monitoring, can reduce liver size and improve long-term health. If you’re unsure about the next steps—or if symptoms persist beyond two weeks—consult a doctor online with Apollo 24|7 for personalized guidance. They can arrange home collections for key tests and help you plan follow-up. With the right information and support, most people can address the causes behind hepatomegaly and protect their liver in the long run.Consult a Top General Physician
Consult a Top General Physician

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(425+ Patients)

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult a Top General Physician

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(425+ Patients)

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from Liver disease
Frequently Asked Questions
1) What are the most common hepatomegaly symptoms in adults?
Early signs are often subtle—fullness or mild pain in the right upper abdomen, fatigue, and abnormal liver function tests. Red flags include jaundice, severe pain, swelling, or confusion. If these persist, consult a doctor online with Apollo 24|7.
2) How is hepatomegaly different from fatty liver?
Hepatomegaly refers to size; fatty liver is fat accumulation in liver cells. You can have fatty liver without an enlarged liver and vice versa. Ultrasound often distinguishes fatty change and measures liver size.
3) What causes hepatomegaly with splenomegaly?
Hepatosplenomegaly can reflect portal hypertension from chronic liver disease, certain infections, blood disorders, or infiltrative diseases. Your doctor may order viral tests, blood counts, and imaging to narrow the cause.
4) What tests diagnose hepatomegaly and its cause?
Liver function tests, viral hepatitis panels, iron and copper studies, autoimmune markers, and ultrasound are common. CT/MRI and elastography may follow. Apollo 24|7 offers home collection for many of these tests.
5) Can hepatomegaly be treated at home?
Home measures help when the cause is metabolic: weight loss, Mediterranean-style diet, regular exercise, and alcohol avoidance can shrink fatty liver. However, causes like viral hepatitis, heart failure, or cholestasis need medical treatment. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7.
.webp)