What Leads To Low Sperm Count Treatment
Discover the causes, diagnosis, and treatments for low sperm count (oligospermia). Learn about lifestyle changes, medical options, and fertility treatments that can help improve sperm health.

Written by Dr. Mohammed Kamran
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 2nd Feb, 2026

Introduction
Struggling to conceive can be frustrating and confusing—especially when test results point to low sperm count. Also called oligospermia, low sperm count means fewer sperm than expected are present in semen, which can make pregnancy less likely. The good news: many causes are reversible, and even when counts are very low, effective treatments and assisted reproduction options exist. In this guide, we’ll explain what low sperm count is, the most common causes, how it’s diagnosed, and the treatments that work—from lifestyle changes and supplements to medical procedures and fertility technologies. You’ll also learn how to interpret a semen analysis, which tests are truly helpful, timelines for improvement, and practical steps you can start today. If you’re worried about your count, this article will help you make a clear plan, ask better questions, and feel more in control of your fertility journey.
What Is Low Sperm Count (Oligospermia)?
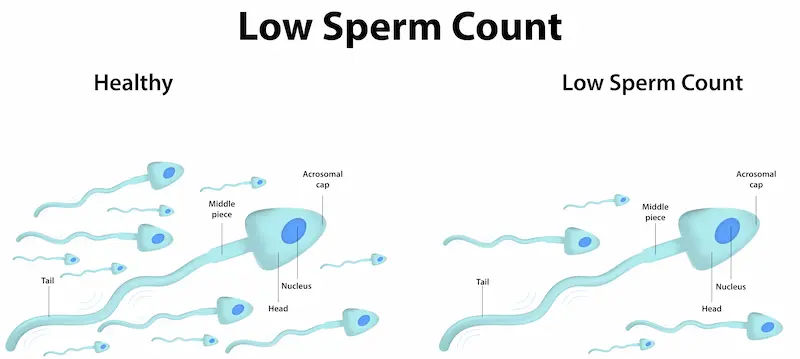
Low sperm count means the number of sperm in a man’s ejaculate is lower than typical reference levels. Doctors commonly use semen analysis standards informed by the World Health Organization (WHO). As a general guide, a sperm concentration below about 15 million per millilitre is considered “low,” though the latest WHO manual emphasises interpretation in clinical context rather than rigid cut-offs. Low count can exist on its own, or alongside other semen issues like low motility (movement) or abnormal morphology (shape).
How doctors define “low”
- Sperm concentration (per millilitre) and total sperm number (per ejaculate) are both considered.
- A single test is not definitive—because sperm production fluctuates, two or more semen analyses, at least 2–3 weeks apart, are recommended.
- Results are interpreted with other factors: time trying to conceive, female partner’s age, and other semen parameters.
How common is it?
- Infertility affects about 1 in 7 couples, and male factors are involved in roughly 30–50% of cases.
- Low sperm count is one of the most common male infertility findings, often due to a varicocele (dilated veins around the testicle), lifestyle factors, or hormonal issues.
Signs, Symptoms, and When to Test
Low sperm count itself rarely causes obvious symptoms. Many men feel healthy and only discover the issue after months of trying to conceive.
Clues that point to a sperm issue
- Difficulty conceiving after 12 months (or 6 months if the female partner is 35+).
- A history of undescended testicle(s), testicular torsion, chemotherapy, pelvic or groin surgery, or significant injury.
- Signs of hormone imbalance: low libido, erectile dysfunction, decreased shaving frequency, breast tenderness, loss of muscle mass.
- Pain, swelling, or a dragging sensation in the scrotum that worsens on standing (possible varicocele).
- Thick, low-volume semen or painful ejaculation (possible blockage or infection).
When to see a specialist
- If you’ve tried for 12 months without success (6 months if age ≥35) or have any of the above clues, get a semen analysis and talk to a urologist or reproductive specialist.
- If you have testicular pain, a palpable scrotal mass, or a sudden change in testicle size, seek care promptly.
- If symptoms persist beyond two weeks or you have concerns about fertility, consult a doctor online with Apollo 24|7 for further evaluation. Apollo 24|7 also offers convenient home collection for relevant lab tests like fasting glucose, thyroid profile, vitamin D, and reproductive hormones when clinically indicated.
How Sperm Are Made—and Where Things Can Go Wrong
Sperm are produced in the testicles, refined in the epididymis, mixed with seminal fluid, and ejaculated through the urethra. Each stage can affect count.
The 90-day sperm cycle in brief
- Spermatogenesis (production) takes about 64–74 days, plus 12–21 days of transit and maturation in the epididymis—roughly a 3-month cycle.
- This timeline explains why lifestyle changes today often show up in semen results about three months later.
Production, transport, and delivery
- Brain-hormone axis: The hypothalamus and pituitary release GnRH, LH, and FSH to stimulate the testes. Disruptions (pituitary disease, anabolic steroid or testosterone use) can suppress sperm production.
- Testes: Heat, toxins, varicocele, and certain infections can impair the germ cells that make sperm, lowering count.
- Transport: Blockages in the epididymis, vas deferens, or ejaculatory ducts can drastically reduce sperm count in semen, sometimes down to zero (azoospermia) despite normal production.
Causes and Risk Factors for Low Sperm Count
Medical causes
- Varicocele: Enlarged scrotal veins raise testicular temperature and oxidative stress, impairing sperm production.
- Hormonal disorders: Low LH/FSH or extreme obesity can suppress testicular function.
- Infections: Mumps orchitis, sexually transmitted infections, or prostatitis/epididymitis can damage or obstruct sperm pathways.
- Blockages: Congenital or acquired obstruction of the vas deferens or ejaculatory ducts lowers or eliminates sperm in semen.
- Systemic diseases: Severe liver/kidney disease, uncontrolled diabetes, thyroid disorders can impair sperm production.
Lifestyle and environmental factors
- Heat exposure: Frequent hot tubs, tight underwear, keeping a laptop on the lap, or prolonged cycling can reduce count.
- Smoking and vaping: Associated with lower sperm concentration and motility; quitting improves parameters.
- Alcohol and drugs: Heavy alcohol, cannabis, and opioids can impair the hormonal axis and sperm production.
- Weight and diet: Obesity correlates with lower sperm count and testosterone; improving weight can help.
- Toxins: Pesticides, solvents, phthalates, and BPA are linked to poorer semen quality.
Genetic causes and medications
- Genetic: Y chromosome microdeletions, Klinefelter syndrome, CFTR mutations can cause very low or zero sperm count.
- Medications: Testosterone therapy, finasteride, chemotherapy, spironolactone, cimetidine, and certain antifungals/antibiotics can reduce count.
Temporary drops after fever or illness
- High fevers and severe illnesses can temporarily lower count and motility, usually recovering over 1–3 cycles.
Consult Top Specialists Here
Diagnosing Low Sperm Count: Tests You Actually Need
Semen analysis fundamentals
- The semen analysis evaluates volume, sperm concentration (count), total sperm number, motility, morphology, and vitality.
- Collection basics: 2–7 days of abstinence; masturbate into a sterile container; keep it warm and deliver within 1 hour, or use an approved at-home collection kit.
- Repeat testing: Because counts fluctuate, repeat at least once after 2–3 weeks under similar conditions.
Hormone tests, imaging, and genetics
- Hormones: FSH, LH, total testosterone (morning), prolactin, and sometimes estradiol help identify pituitary/testicular issues.
- Imaging: Scrotal ultrasound confirms varicocele or testicular abnormalities; transrectal ultrasound can assessejaculatory ducts in suspected obstruction.
- Genetics: Karyotype and Y-chromosome microdeletion testing for very low counts or azoospermia; CFTR testing if vas deferens is absent.
- Additional: STI screening, urinalysis post-ejaculation (retrograde ejaculation), and in select cases, sperm DNA fragmentation testing.
Interpreting your results (beyond a single number)
- Look at total motile sperm count (TMSC): volume × concentration × motility.
- Morphology varies by lab method; avoid overemphasising it in isolation.
- A borderline low count with excellent motility/morphology may still yield pregnancy, especially with well-timed intercourse.
If you’re arranging tests in India, Apollo 24|7 offers guided test booking and home collection for many related labs, and you can consult a urologist or andrologist online to interpret results and plan next steps.
Evidence-Based Treatments That Raise Sperm Count
Treating varicocele
- Men with a palpable varicocele on exam, abnormal semen parameters, and infertility often see improved semen quality after repair.
- Microsurgical varicocelectomy is preferred for lower recurrence; embolisation is a minimally invasive alternative.
- Studies note higher spontaneous pregnancy rates after correction in appropriate candidates.
Hormone-related therapies
- Gonadotropin therapy (hCG, sometimes with FSH) can restart sperm production in hypogonadotropic hypogonadism.
- Clomiphene or letrozole may improve endogenous testosterone in selected men; use under specialist care.
- Stop exogenous testosterone; fertility-safe alternatives exist for men who wish to conceive.
Treating infections and stopping offending drugs
- Targeted antibiotics can help for bacterial infections like epididymitis or prostatitis.
- Review all medications with your doctor for possible fertility effects.
Supplements
- Antioxidants (CoQ10, L-carnitine, vitamins C/E, zinc) may improve semen parameters; evidence for live birth benefit is limited.
- Choose high-quality supplements and use as part of a comprehensive plan.
Lifestyle Strategies to Boost Sperm Health
Diet, exercise, and weight
- Eat a Mediterranean-style diet with fruits, vegetables, whole grains, nuts, olive oil, and fish.
- Achieve a healthy BMI; weight loss improves testosterone and sperm parameters.
- Exercise moderately and regularly; avoid high-heat endurance activity before testing.
Heat, toxins, timing, and supplements
- Keep laptops off laps, wear breathable underwear, and limit saunas.
- Avoid smoking and heavy drinking; discuss cannabis with your doctor.
- Reduce toxin exposure by avoiding microwaving plastics and using glass/stainless.
- Have intercourse every 1–2 days in the fertile window for best chances.
- Consider CoQ10, L-carnitine, and zinc if deficient.
Fertility Options If Counts Stay Low
Timed intercourse and IUI
- Works best when total motile sperm count (TMSC) is adequate and female partner factors are favourable.
- IUI success rates drop with very low TMSC; clinics often recommend a minimum threshold to proceed.
IVF and ICSI
- IVF fertilises eggs in the lab; ICSI injects a single sperm into an egg.
- Useful in severe male factor infertility and can achieve fertilisation even with very low count.
Surgical sperm retrieval, donor sperm, and preservation
- TESE/micro-TESE and PESA/TESA retrieve sperm directly from the testicle or epididymis when none are in ejaculate.
- Donor sperm is an option when counts are extremely low or genetic risk is high.
- Bank sperm before starting treatments like chemotherapy that may reduce count.
Prevention, Timelines, and When to Seek Help
The 90-day fertility sprint plan
- Commit to 12 weeks of lifestyle optimisation—sleep, diet, exercise, stress, and substance moderation.
- Align with medical interventions like varicocele repair for maximum benefit.
When to seek help
- If you’ve tried for 12 months (or 6 months if the female partner is 35+) or low sperm count is confirmed twice, see a reproductive urologist.
- If your condition doesn’t improve after these steps, book a physical visit with Apollo 24|7.
Conclusion
Low sperm count can feel like a setback, but it’s often a solvable problem with a clear plan. Start by understanding the basics—what “low” means, how sperm are made, and which factors most commonly reduce count. Then, get the right tests: at least two semen analyses and targeted labs. With your clinician, address correctable causes such as varicocele, medication effects, or hormonal issues, and pair that with a 90-day lifestyle sprint that optimises sleep, nutrition, weight, exercise, and heat hygiene. If counts remain low, modern fertility treatments—from IUI to IVF with ICSI and surgical sperm retrieval—offer strong paths to parenthood. Throughout the process, set checkpoints so you can adapt quickly instead of losing time. If you’re unsure where to start or progress stalls, consult a doctor online with Apollo 24|7; if lab work is needed, home collection can make it simple to stay on track. With a thoughtful, stepwise approach, most couples can move from uncertainty to action—and often, to success.
Consult Top Specialists Here
Consult Top Specialists Here
Dr Debanga Sarma
Urologist
10 Years • MBBS, MS (GENERAL SURGERY)M.Ch (UROLOGY)
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
Dr S K Singhanina
Urologist
25 Years • MBBS/MS/DNB AND MCH UROLOGY
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati

Dr. Pavan Kumar S K
Urologist
11 Years • MBBS, MS , Mch( Urology) DNB (Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Pradeep Champawat
Urologist
10 Years • MBBS, MS, DNB Urology
Delhi
Apollo Hospitals Indraprastha, Delhi
(175+ Patients)

Dr. Ramesh H
Urologist
16 Years • MBBS, MS , Mch( Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Consult Top Specialists Here
Dr Debanga Sarma
Urologist
10 Years • MBBS, MS (GENERAL SURGERY)M.Ch (UROLOGY)
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
Dr S K Singhanina
Urologist
25 Years • MBBS/MS/DNB AND MCH UROLOGY
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati

Dr. Pavan Kumar S K
Urologist
11 Years • MBBS, MS , Mch( Urology) DNB (Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Pradeep Champawat
Urologist
10 Years • MBBS, MS, DNB Urology
Delhi
Apollo Hospitals Indraprastha, Delhi
(175+ Patients)

Dr. Ramesh H
Urologist
16 Years • MBBS, MS , Mch( Urology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
More articles from Low sperm count
Frequently Asked Questions
1) What is considered a low sperm count?
A sperm concentration below about 15 million per millilitre is generally considered low, but results must be interpreted alongside motility, morphology, and clinical context. Repeat testing is recommended before making decisions.
2) How long does it take to improve low sperm count naturally?
About three months. Sperm take roughly 74 days to develop, plus time in transit, so lifestyle changes and treatments usually show on semen analysis after one full cycle.
3) Do supplements like CoQ10 or L-carnitine really help?
Some studies show modest improvements in semen parameters with antioxidants, but evidence for improving live birth is limited. Use supplements as an adjunct to medical and lifestyle treatment.
4) Can IUI work with low sperm count?
It depends on total motile sperm count (TMSC). IUI success declines with very low TMSC; IVF with ICSI may be recommended if TMSC is too low.
5) Does testosterone therapy lower sperm count?
Yes. Exogenous testosterone suppresses the hormonal signals needed for sperm production, often causing very low count or azoospermia. Men trying to conceive should avoid testosterone therapy and discuss fertility-safe alternatives with a specialist.
.webp)