Understanding Neuroendocrine Tumors: Types, Causes, Symptoms, and Treatment
Neuroendocrine tumours (NETs) are a group of uncommon tumours that originate from neuroendocrine cells. These cells have traits similar to both nerve cells and hormone-producing endocrine cells. NETs can occur anywhere in the body but are most commonly found in the gastrointestinal tract, lungs, and pancreas. This article provides a comprehensive overview of the types, causes, symptoms, and treatment options for neuroendocrine tumours.

Written by Dr.Sonia Bhatt
Last updated on 3rd Jul, 2025
Types of Neuroendocrine Tumors
Neuroendocrine tumours are classified based on their location and whether they produce hormones:
Functional NETs: These tumours produce hormones that can lead to symptoms due to hormone overproduction (like insulin or serotonin).
Non-Functional NETs: These tumours don't produce hormones and often don’t show symptoms until they become quite large.
Common types of neuroendocrine tumours include:
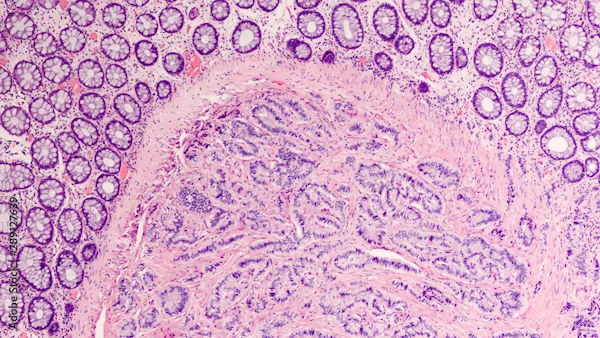
Gastrointestinal Neuroendocrine Tumors (GI-NETs): These tumours most commonly start in the intestines, rectum, or appendix. They were previously known as carcinoid tumours.
Lung Neuroendocrine Tumors: These tumours start in the lungs or bronchi and are the second most common type of NET.
Pancreatic Neuroendocrine Tumors (P-NETs): These tumours start in the pancreas and are a type of pancreatic cancer.
Causes of Neuroendocrine Tumors
The exact cause of neuroendocrine tumours is not well understood, but several factors may contribute to their development:
Genetic Mutations: Changes in the DNA of neuroendocrine cells can lead to uncontrolled cell growth and tumour formation.
Inherited Genetic Syndromes: Certain genetic syndromes, such as Multiple Endocrine Neoplasia (MEN) types 1 and 2, Von Hippel-Lindau disease, and Neurofibromatosis, increase the risk of developing NETs.
Environmental Factors: Exposure to certain environmental factors and chemicals may increase the risk of developing NETs, although more research is needed to confirm these associations.
Symptoms of Neuroendocrine Tumors
The symptoms of neuroendocrine tumours can vary depending on the type, location, and whether the tumour produces hormones. Common symptoms include:
Pain: Pain from a growing tumour, which may be localised or spread to other areas.
Lump: A growing lump that can be felt under the skin.
Fatigue: Feeling unusually tired without a clear reason.
Weight Loss: Unintentional weight loss.
For functional NETs that produce excess hormones, additional symptoms may include:
Skin Flushing: Episodes of skin flushing or redness.
Diarrhea: Frequent diarrhea.
Frequent Urination: Increased frequency of urination.
Increased Thirst: Feeling unusually thirsty.
Dizziness and Shakiness: Episodes of dizziness or shakiness.
Skin Rash: Development of a skin rash.
Diagnosis of Neuroendocrine Tumors
Diagnosing neuroendocrine tumours involves a combination of imaging studies, laboratory tests, and sometimes biopsy. Common diagnostic tools include:
Imaging Studies: X-rays, CT scans, MRI, and PET scans can help visualise the extent and location of the tumour.
Blood and Urine Tests: These tests can detect elevated levels of hormones and other markers associated with NETs.
Biopsy: A biopsy of the tumour may be performed to confirm the diagnosis and determine the type of NET.
Treatment of Neuroendocrine Tumors
The treatment of neuroendocrine tumours (NETs) depends on several factors, including the type of tumour, its location, whether it is functional (producing hormones), its stage, and the patient's overall health. Here is a detailed overview of the various treatment options available for neuroendocrine tumours:
1. Surgery
Surgery is often the primary treatment for neuroendocrine tumours, especially if the tumour is localised and can be completely removed. The type of surgery performed depends on the tumour's location and size:
Resection: Surgical removal of the tumour and some surrounding healthy tissue to ensure complete removal.
Debulking: In cases where the tumour cannot be entirely removed, debulking surgery aims to remove as much of the tumour as possible to reduce symptoms and improve the effectiveness of other treatments.
Liver Resection: For NETs that have spread to the liver, liver resection may be performed to remove metastatic tumours.
Liver Transplant: In rare cases, a liver transplant may be considered for patients with extensive liver involvement.
2. Radiation Therapy
Radiation therapy uses high-energy beams to target and destroy cancer cells. It is often used in combination with surgery for malignant NETs, especially in cases where the tumour is large, has spread to nearby tissues, or cannot be completely removed surgically. Types of radiation therapy include:
External Beam Radiation Therapy (EBRT): This is the most common form of radiation therapy, where radiation is delivered from a machine outside the body.
Intensity-Modulated Radiation Therapy (IMRT): A more advanced form of EBRT that allows for precise targeting of the tumour while minimising damage to surrounding healthy tissue.
Peptide Receptor Radionuclide Therapy (PRRT): PRRT involves using radioactive substances to target and destroy cancer cells. It is a newer treatment option for certain types of NETs, particularly those that express somatostatin receptors.
3. Chemotherapy
Chemotherapy uses drugs to kill cancer cells or stop their growth. It is commonly used to treat malignant NETs that have spread to other parts of the body. Chemotherapy can help shrink tumours and kill cancer cells. Common chemotherapy drugs used for NETs include:
Streptozocin: Often used in combination with other drugs like doxorubicin or fluorouracil.
Temozolomide: Sometimes combined with capecitabine for treating pancreatic NETs.
Etoposide and Cisplatin: Commonly used for high-grade NETs, such as small cell lung cancer.
4. Targeted Therapy
Targeted therapy involves using drugs that specifically target cancer cells while sparing normal cells. These drugs work by interfering with specific molecules involved in cancer cell growth and survival. Targeted therapy is often used for certain types of malignant NETs. Examples of targeted therapy drugs include:
Everolimus (Afinitor): An mTOR inhibitor used to treat advanced pancreatic NETs and other types of NETs.
Sunitinib (Sutent): A tyrosine kinase inhibitor used to treat advanced pancreatic NETs.
5. Hormone Therapy
Hormone therapy can help manage symptoms caused by functional NETs that produce excess hormones. Somatostatin analogues are commonly used to control hormone-related symptoms and slow tumour growth. Examples include:
Octreotide (Sandostatin): A somatostatin analogue that helps control symptoms and slow tumour growth.
Lanreotide (Somatuline Depot): Another somatostatin analogue used to manage symptoms and inhibit tumour growth.
6. Immunotherapy
Immunotherapy is a type of treatment that harnesses the body's immune system to fight cancer. It is an emerging area of research for neuroendocrine tumours and may be considered for certain patients, particularly those with advanced or recurrent disease. Types of immunotherapy include:
Immune Checkpoint Inhibitors: These drugs, such as pembrolizumab (Keytruda) and nivolumab (Opdivo), block proteins that prevent the immune system from attacking cancer cells.
7. Peptide Receptor Radionuclide Therapy (PRRT)
PRRT is a targeted treatment that involves using radioactive substances to target and destroy cancer cells. It is particularly effective for NETs that express somatostatin receptors. The most commonly used PRRT agent is Lutetium-177 (Lu-177) DOTATATE. PRRT can help shrink tumours, relieve symptoms, and improve quality of life.
Living with Neuroendocrine Tumors
Living with neuroendocrine tumours can be challenging, but several strategies can help improve quality of life:
Pain Management: Work with your healthcare team to develop an effective pain management plan. This may include medications, physical therapy, and complementary therapies such as acupuncture.
Nutrition: Maintaining a balanced diet is crucial for overall health and recovery. If you experience difficulty eating or have specific dietary needs, a nutritionist can help you develop a diet plan that meets your nutritional needs.
Emotional Support: Coping with a diagnosis of neuroendocrine tumours can be emotionally challenging. Seek support from family, friends, and support groups to help manage stress and anxiety.
Regular Follow-Up: Regular follow-up appointments with your healthcare provider are essential to monitor your condition and detect any recurrence early.
Conclusion
Neuroendocrine tumours (NETs) are a rare but significant condition that can affect various parts of the body. Understanding the types, causes, symptoms, and treatment options for NETs is crucial for effective management and maintaining overall health. Early detection and appropriate treatment can improve the prognosis for many individuals with neuroendocrine tumours. If you experience persistent symptoms or notice a lump, it is important to consult a healthcare provider for proper diagnosis and treatment.
Consult Top Neurologists
Consult Top Neurologists

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Dr. Annakula Ramu
Neurologist
7 Years • MBBS, MD General Medicine, DM Neurology
Jagtial
Sairam Neuro and Children Hospital, Jagtial

Dr Rajashekar Mummadi
Neurologist
2 Years • MBBS, DNB General Medicine, DRNB Neurology
Hyderabad
Dr Ram's Neuro Clinic, Hyderabad

Dr Chandu Samba Siva Rao
Neurologist
7 Years • MBBS, MD GENERAL MEDICINE, DM NEUROLOGY
Vijayawada
Chandu Neuro Center, Vijayawada

Dr. Abhinav Gupta
Neurologist
18 Years • MBBS, MD (GENERAL MEDICINE), DM (NEUROLOGY)
Ghaziabad
Bhava Neurocenter, Ghaziabad
