Causes and Risk Factors of Pancreatic Cancer
Learn about the causes and risk factors of pancreatic cancer, helping you understand who is most at risk and how early detection can make a difference.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
Pancreatic cancer is often called a "silent" disease, not because it makes no sound, but because it typically reveals itself only in its later, more advanced stages. This daunting reality makes understanding its origins not just a matter of curiosity, but one of profound importance. What transforms healthy pancreatic cells into aggressive, cancerous ones? While a single, simple cause remains elusive, decades of medical research have pinpointed a clear set of risk factors that significantly increase the odds of developing this condition. This article will demystify the leading causes of pancreatic cancer, separating the factors beyond your control from those you can potentially influence. We'll explore everything from genetics and age to lifestyle choices and underlying health conditions, empowering you with knowledge about this complex disease.
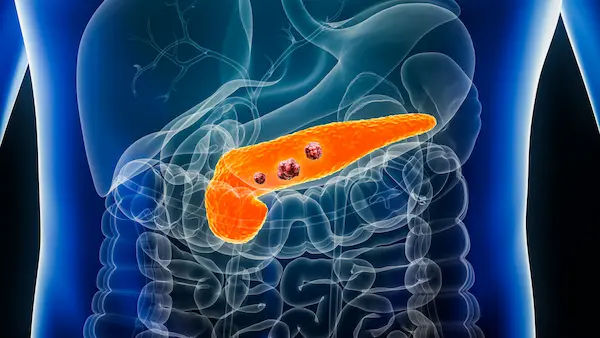
Understanding Your Pancreas: The Organ at Risk
Nestled deep within your abdomen, behind your stomach, is a six-inch-long, tadpole-shaped organ called the pancreas. Though small, its functions are critical to your survival. It operates as a dual-function gland, playing a key role in both your digestive and endocrine systems.
The Role of the Pancreas in Digestion
The pancreas produces pancreatic juice, which is packed with powerful enzymes. This juice is released into the small intestine to break down fats, proteins, and carbohydrates from the food you eat. Without these enzymes, your body couldn't absorb essential nutrients, leading to malnutrition and weight loss, a common symptom when a tumour blocks the pancreatic ducts.
The Role of the Pancreas in Blood Sugar Control
Scattered throughout the pancreas are clusters of cells called islets of Langerhans. These are the endocrine factories of the organ, producing vital hormones like insulin and glucagon. Insulin lowers blood sugar, while glucagon raises it. Together, they maintain the delicate balance of glucose in your bloodstream, providing energy to your cells. A malfunctioning pancreas can directly lead to diabetes, which is both a risk factor and a potential symptom of pancreatic cancer.
Consult an Oncologist for the best advice
The Main Types of Pancreatic Cancer
Not all pancreatic cancers are the same. The type is determined by the cell where the cancer originates, which greatly influences its behavior and treatment.
Pancreatic Ductal Adenocarcinoma (PDAC)
This is the most common type, accounting for over 90% of all cases. It begins in the lining of the ducts that carry digestive enzymes out of the pancreas. When people talk about the alarming statistics and challenges of pancreatic cancer, they are most often referring to PDAC. Its aggressive nature and late detection contribute to its high mortality rate.
Pancreatic Neuroendocrine Tumours (PNETs)
Also known as islet cell tumours, these are much rarer, making up less than 5% of cases. They originate in the hormone-producing endocrine cells. PNETs tend to be less aggressive than PDAC and can sometimes themselves produce hormones, leading to distinct syndromes like uncontrollable insulin production (causing hypoglycaemia) or gastrin overproduction (causing severe ulcers).
Primary Risk Factors You Can't Change
Several significant risk factors for developing pancreatic cancer are inherent and unchangeable. Awareness of these can help you and your doctor understand your personal risk profile.
Age and Demographic Factors
The risk of developing pancreatic cancer increases sharply with age. Most patients are diagnosed after the age of 65. Additionally, race plays a role; African Americans have a slightly higher incidence rate than other racial groups. The reasons for this disparity are complex and may involve a combination of socioeconomic factors, access to healthcare, and higher rates of other risk factors like diabetes.
The Role of Family History and Inherited Genes
While most cases are sporadic, about 10% are considered familial, meaning they cluster in families. Having a first-degree relative (parent, sibling, or child) with the disease doubles or even triples your risk. This points to the role of inherited genetic mutations.
Hereditary Syndromes Linked to Pancreatic Cancer
Specific inherited syndromes carry a significantly higher risk. These include:
BRCA2 Mutation: Known for its link to breast and ovarian cancer, this gene also increases pancreatic cancer risk.
Lynch Syndrome: A hereditary condition that predisposes individuals to colorectal cancer and other cancers, including those of the pancreas.
Familial Atypical Multiple Mole Melanoma (FAMMM) Syndrome: Characterized by multiple moles and melanomas, this syndrome, caused by a p16 gene mutation, also increases pancreatic risk.
Peutz-Jeghers Syndrome: A rare disorder that causes intestinal polyps and is linked to a high lifetime risk of various gastrointestinal cancers.
Lifestyle and Environmental Risk Factors You Can Influence
This is the category where individuals have the most agency. Modifying these factors can meaningfully reduce your overall risk.
Smoking and Tobacco Use
This is the most significant, consistent, and avoidable risk factor. Smokers are two to three times more likely to develop pancreatic cancer than non-smokers. It's estimated that 20-30% of pancreatic cancers are caused by cigarette smoking. The carcinogens in tobacco smoke enter the bloodstream and damage the pancreas. The good news? Quitting smoking reduces your risk, and after about 20 years, it can approach that of a never-smoker.
Obesity and Body Weight
Being overweight or obese, particularly in early adulthood, increases the risk. A body mass index (BMI) of 30 or higher is associated with a roughly 20% increased risk. The link is believed to be chronic inflammation and higher levels of insulin and growth factors that can stimulate cancer cell growth. Maintaining a healthy weight is a key strategy in pancreatic cancer prevention.
Diet and Alcohol Consumption
A diet high in red and processed meats, saturated fats, and sugary drinks may contribute to risk, likely through pathways involving obesity and inflammation. Conversely, a diet rich in fruits, vegetables, and whole grains appears to be protective. Heavy, long-term alcohol consumption is a leading cause of chronic pancreatitis, a known risk factor for pancreatic cancer.
Underlying Health Conditions That Increase Risk
Certain chronic diseases create an internal environment that is conducive to the development of cancer cells in the pancreas.
Chronic Pancreatitis
Long-standing inflammation of the pancreas, often caused by heavy alcohol use or genetic factors, is a well-established risk factor. The constant cycle of damage and repair can lead to genetic mistakes in cells, eventually leading to cancer. The risk is even higher in patients with hereditary pancreatitis.
Diabetes Mellitus
The relationship between diabetes and pancreatic cancer is complex and bidirectional. Long-standing type 2 diabetes is a known risk factor, likely due to high insulin levels and insulin resistance. More intriguingly, the sudden onset of type 2 diabetes in someone over 50 can sometimes be an early warning sign of an underlying pancreatic tumour that is disrupting insulin production. If you experience a sudden and unexplained diagnosis of diabetes and pancreatic cancer symptoms like jaundice or weight loss, it warrants a thorough medical evaluation.
Certain Bacterial Infections
Some research suggests a potential link between infection with Helicobacter pylori (the bacteria known for causing stomach ulcers) and an increased risk of pancreatic cancer. The theory is that the infection may cause systemic inflammation. However, this link is not as firmly established as other risk factors.
How These Factors Lead to Cancer: The Cellular Story
At its core, cancer is a disease of DNA. All the risk factors discussed ultimately contribute to genetic damage (mutations) in the DNA of pancreatic cells. These mutations disrupt the normal instructions for cell growth and division. Proto-oncogenes, which promote cell growth, can become stuck in the "on" position, while tumour suppressor genes, which repair DNA or tell damaged cells to die, can be turned "off." With these critical safeguards disabled, cells begin to multiply uncontrollably, forming a tumour. This tumour can then invade nearby tissues and spread (metastasize) to other parts of the body.
Conclusion
Understanding what leads to pancreatic cancer is a complex puzzle involving genetics, lifestyle, and environment. While certain risks like age and family history are beyond our control, this knowledge empowers us to be vigilant about our health and proactive in communicating our history to doctors. More importantly, it highlights significant areas where we can take action. Quitting smoking, achieving a healthy weight, and managing chronic conditions like diabetes are not just general health advice, they are concrete steps toward reducing your risk of this challenging disease. Knowledge is the first line of defense. If you identify with several of these risk factors, especially if you are experiencing any unusual symptoms, the most powerful step you can take is to seek professional medical guidance for a personalised evaluation.
Consult an Oncologist for the best advice
Consult an Oncologist for the best advice

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Raja T
Oncologist
20 Years • MBBS; MD; DM
Chennai
Apollo Hospitals Greams Road, Chennai
(200+ Patients)

Dr. Ruquaya Ahmad Mir
Surgical Oncologist
20 Years • MBBS, DNB
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Vishwanath S
Oncologist
8 Years • MBBS, MD, DM, Fellowship at MD Anderson Cancer Center
Bengaluru
Apollo Spectra Hospitals, Koramangala, Bengaluru

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
More articles from Pancreatic Cancer
Frequently Asked Questions
1. Can pancreatic cancer be prevented?
There is no guaranteed way to prevent pancreatic cancer, but you can significantly reduce your risk by adopting a healthy lifestyle. This includes avoiding tobacco, maintaining a healthy weight, exercising regularly, and eating a diet rich in fruits, vegetables, and whole grains.
2. Is pancreatic cancer always hereditary?
No, the vast majority (about 90%) of pancreatic cancer cases are sporadic, meaning they occur without a known family history. Only about 10% of cases are considered familial or hereditary, linked to specific inherited genetic syndromes.
3. What are the very first signs of pancreatic cancer?
Early signs are often vague and easily mistaken for other conditions. They can include new-onset diabetes, loss of appetite, unexplained weight loss, abdominal or mid-back pain that may worsen after eating or lying down, and digestive issues like nausea. Jaundice (yellowing of the skin and eyes) is a more specific but often later sign.
4. Does chronic pancreatitis always lead to cancer?
No, not always. However, it is a significant risk factor. The long-term inflammation associated with chronic pancreatitis increases the chance of cellular DNA damage over time. Managing the condition and avoiding alcohol are crucial for patients.
5. If a parent had pancreatic cancer, should I get genetic testing?
It depends on the family history. If you have two or more first-degree relatives with the disease, or one relative who was diagnosed at a very young age, it may be worth discussing genetic counseling and testing with your doctor or a genetic counselor to assess your risk and the potential value of testing.
.webp)