Guide to Signs Your Parkinsons Disease Progressing
Know about the signs of parkinsons disease. Understanding what it is, symptoms that progression of disease and practicing life monitoring.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
Living with Parkinson's disease means navigating a journey of change. While diagnosis often focuses on the well-known motor symptoms like tremors and stiffness, understanding how the condition evolves is crucial for effective management. Parkinson's is a progressive neurodegenerative disorder, meaning symptoms gradually change and new challenges can appear. This guide is designed to help you, your family, and your caregivers recognise the signs that Parkinson's disease may be progressing. We will move beyond simple stages to explore the specific motor and non-motor changes you might notice in your daily life. By knowing what to look for, you can take timely steps to adjust treatments and maintain your quality of life for as long as possible. If you notice consistent new or worsening symptoms, it's essential to consult a neurologist. You can book a consultation with a specialist online through Apollo24|7 to discuss your concerns.
Understanding Parkinson's as a Progressive Condition
Parkinson's disease is caused by the loss of dopamine-producing cells in the brain. Since this loss continues over the
years, the symptoms inevitably change. Progression is not a straight line; it's unique to each individual. Some people
experience slow changes over decades, while others may see a more rapid shift.
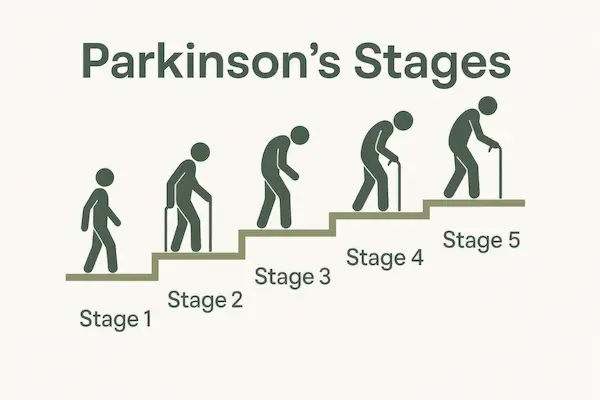
What Does "Disease Progression" Actually Mean?
"Disease progression" refers to the worsening of existing symptoms or the emergence of new ones. Initially, symptoms
are typically unilateral (affecting one side of the body) and respond well to medication. As the disease advances,
symptoms often become bilateral, medication effects may wear off sooner, and non-motor issues can become more
prominent. It's less about reaching a specific "stage" and more about recognising a pattern of change in your functional
abilities.
Consult a Top Neurologist for Personalised Advice
The Role of Levodopa and "On/Off" Periods
Levodopa, the primary medication for Parkinson's, replaces lost dopamine. In the early stages, its effect is smooth and long-lasting. A key sign of Parkinson's progression is the development of "motor fluctuations" or "on/off" periods. The "on" period is when the medication is working well, and mobility is good. The "off" period is when the medication wears off, and symptoms like stiffness and slowness return. These fluctuations indicate that the brain's ability to store and release dopamine smoothly is diminishing, a hallmark of advancing disease.
Key Motor Symptoms That Signal Progression
Motor symptoms are the most visible indicators of change. Tracking these helps in managing advanced Parkinson's
symptoms effectively.
Increased Tremors and Rigidity
While a tremor might have been the first sign, it may become more pronounced or spread to other limbs. Rigidity
(stiffness) often increases, making tasks like buttoning a shirt or turning over in bed more difficult. This isn't just normal
ageing; it's a distinct increase in resistance to movement.
Postural Instability and Balance Problems
This is one of the most significant markers of progression. In mid to late stages, balance reflexes weaken, leading to a
high risk of falls. You might notice a stooped posture, a tendency to lean to one side, or a feeling of being unsteady
when turning or walking on uneven surfaces. Postural instability is a primary reason for using assistive devices like a
cane or walker.
Changes in Gait and Freezing Episodes
Walking patterns often change. Steps may become shorter and shuffling (known as festination). A particularly
challenging sign is "freezing of gait," where your feet feel temporarily glued to the floor, especially when starting to
walk, navigating tight spaces, or turning. This freezing is a major cause of falls and a clear sign that the disease is
affecting more complex motor circuits.
Dyskinesia: The Challenge of Long-Term Medication
As a counterpart to "off" periods, dyskinesia—involuntary, writhing movements—can appear. This is often a side effect
of long-term levodopa use and becomes more common as the disease progresses and doses are adjusted to manage
worsening symptoms. It represents a delicate balancing act between controlling Parkinsonian symptoms and avoiding
medication-induced movements.
The Often-Overlooked Non-Motor Symptoms of Advancing Parkinson's
Non-motor symptoms can be more disabling than motor issues and are critical indicators of Parkinson's worsening.
Cognitive Changes and Mood Disorders
Beyond movement, Parkinson's can affect cognitive functions. You might experience "brain fog," slowed thinking,
difficulty with multitasking, or problems with memory. Mood disorders like depression, anxiety, and apathy (a loss of
motivation) are very common and can significantly impact quality of life. These are not personal failings but part of the
disease's impact on brain chemistry.
Autonomic Dysfunction: Blood Pressure, Digestion, and Bladder
The autonomic nervous system controls automatic body functions. Progression can lead to orthostatic hypotension (a
sharp drop in blood pressure upon standing, causing dizziness), severe constipation, urinary urgency or frequency, and
excessive sweating. These non-motor symptoms require specific management strategies alongside motor treatment.
Sleep Disturbances and Daytime Fatigue
Sleep problems are pervasive. This includes insomnia, frequent waking, vivid dreams or nightmares (often a side effect
of medication), and a condition called REM sleep behaviour disorder, where people act out their dreams. The result is
often overwhelming daytime fatigue that isn't relieved by rest.
Practical Self-Monitoring: What to Track in Your Daily Life
Being proactive is your greatest tool. Instead of worrying about every change, systematic tracking provides concrete
data for your doctor.
Creating a Simple Symptom Diary
Keep a simple log. Note the time you take your medication, when you feel your symptoms are well-controlled ("on"
time), and when they return ("off" time). Also, jot down any non-motor issues like dizziness, mood changes, or sleep
quality. This diary is invaluable for your neurologist to fine-tune your treatment plan.
Knowing When to Talk to Your Doctor
You should contact your doctor if you experience: frequent falls, significant "off" periods that disrupt your day,
distressing dyskinesia, new or worsening confusion, hallucinations, or dramatic changes in mood or sleep. If your
condition does not improve after trying these methods of tracking and adjustment, book a physical visit to a doctor with
Apollo24|7 for a comprehensive evaluation. Early intervention can prevent complications.
Conclusion
Recognising the signs of Parkinson's disease progression is not about fostering fear, but about fostering control. This
journey is unique, and changes will occur. However, by understanding what to expect from the more obvious motor fluctuations to the subtle yet impactful non-motor symptoms you can transition from a passive patient to an active manager of your health. The key is consistent communication with your healthcare team. Use a symptom diary, report changes honestly, and work together to adjust your treatment plan, which may include medications, physical therapy, or even advanced options like Deep Brain Stimulation (DBS). Remember, the goal of management evolves, focusing not just on symptom control but on preserving your independence and quality of life. You are not alone on this path, and being informed is your first and most powerful step forward.
Consult a Top Neurologist for Personalised Advice
Consult a Top Neurologist for Personalised Advice

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Consult a Top Neurologist for Personalised Advice

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
More articles from Parkinsons Disease
Frequently Asked Questions
1. How fast does Parkinson's disease typically progress?
The rate of progression varies greatly from person to person. Factors like age at onset and overall health play a role. For some, significant changes may take 5-10 years; for others, the progression is slower. There is no definitive timeline.
2. What are the late-stage symptoms of Parkinson's disease?
In late stages, individuals often become significantly more dependent on caregivers due to severe mobility issues, requiring a wheelchair or being bedbound. Non-motor symptoms like dementia, hallucinations, and swallowing difficulties (dysphagia) become more common and require specialised care.
3. Can you slow down the progression of Parkinson's?
While there is no proven cure to stop progression, certain strategies are believed to be neuroprotective. Regular physical exercise (especially aerobic and balance training), a healthy diet, and staying mentally active are strongly recommended to potentially slow functional decline and maintain brain health.
4. What is the difference between Parkinson's progression and just having a bad day?
A 'bad day' is temporary and often linked to factors like stress, poor sleep, or dehydration. Progression is indicated by a consistent, noticeable trend over weeks or months where symptoms worsen or new ones appear despite maintaining healthy habits and a stable medication routine.
5. What should I do if I notice my symptoms are getting worse?
The most important step is to schedule an appointment with your neurologist. Come prepared with your symptom diary and a clear list of the changes you've observed. Do not adjust your medication dosage on your own. You can consult a doctor online with Apollo24|7 to discuss these changes and determine the best next steps.