Guide to Advanced Laser Treatment Piles
Get the essential guide to advanced laser treatment for piles (hemorrhoids). Learn about benefits, procedure, recovery, and effective relief.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
If you or a loved one is struggling with hemorrhoids—commonly called piles—you’ve likely seen ads and heard stories about “painless laser” solutions. Advanced laser treatment for piles has gained popularity for being minimally invasive, quick, and associated with faster recovery. But is it right for you? How does it compare with rubber band ligation, stapler surgery, or conventional hemorrhoidectomy? What about safety, cost, and long-term results?
This comprehensive guide brings you a clear, balanced overview of advanced laser treatment for piles. You’ll learn how laser procedures work, where they fit in among other options, who they’re best for, what to expect before and after surgery, and how to choose a qualified center. We’ll also summarize what top medical sources and hospital websites say, and share evidence, real-world examples, and practical recovery tips. If symptoms persist beyond two weeks or you’re unsure which treatment to choose, consult a doctor online with Apollo 24|7 for further evaluation.
What Are Piles? A Quick Refresher
Hemorrhoids (piles) are swollen vascular cushions inside the rectum (internal) or under the skin around the anus (external). They help with continence but can become symptomatic—bleeding, itching, pain, mucus discharge, or prolapse—when inflamed or enlarged. Internal hemorrhoids are graded:
• Grade I: bulge inside; bleeding possible, no prolapse
• Grade II: prolapse with straining but reduce spontaneously
• Grade III: prolapse needing manual reduction
• Grade IV: prolapse that cannot be reduced; may thrombose
Common triggers include chronic constipation or diarrhea, straining, prolonged sitting on the toilet, low-fiber diet, pregnancy, obesity, and aging. Many people first try conservative measures—fiber (25–35 g/day), increased fluids, stool softeners, topical agents, and sitz baths. If bleeding persists beyond two weeks or you notice protrusion, pain, or recurrent symptoms, consult a doctor online with Apollo 24|7 for further evaluation and a tailored plan.Consult a Top General Physician
For Grade I–II, office procedures such as rubber band ligation (RBL), sclerotherapy, or infrared coagulation are often effective. Grades III–IV or mixed hemorrhoids may need more definitive options, including advanced laser treatment for piles, stapled hemorrhoidopexy, Doppler-guided ligation, or conventional hemorrhoidectomy. Good news: most hemorrhoid conditions are treatable without hospital admission, and even surgical treatments are often daycare procedures with quick recovery.
Internal vs external hemorrhoids
• Internal: typically painless bleeding, prolapse, mucus; graded I–IV
• External: pain with thrombosis, skin tags, discomfort; not usually treated with laser shrinkage; sometimes requires excision
When to seek help?
• Persistent bleeding, prolapse, severe pain, or anemia symptoms (fatigue, dizziness)
• New or worsening rectal bleeding warrants evaluation to rule out other causes (polyps, fissures). If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7.
Why Consider Advanced Laser Treatment for Piles?
Advanced laser treatment for piles appeals to many patients because it targets hemorrhoidal tissue with controlled energy to shrink, scar, and reposition hemorrhoidal cushions while minimizing open wounds. Two primary laser concepts exist:
• LHP (laser hemorrhoidoplasty): a diode laser fiber (often 1470 nm radial fiber) is inserted into the hemorrhoidal cushion to coagulate and shrink it internally, reducing blood flow and bulk.
• HeLP (hemorrhoidal laser procedure): laser energy is used to coagulate feeding arteries, dearterializing the hemorrhoids, sometimes guided by Doppler to identify arterial branches.
Potential advantages:
• Less postoperative pain than conventional excisional hemorrhoidectomy
• Shorter procedure time, minimal bleeding, daycare discharge
• Faster return to work (often 3–7 days), less need for strong analgesics
• Fewer open wounds around the anus; often no sutures (LHP)
Who benefits most?
• Symptomatic internal hemorrhoids Grade II–III with bleeding and/or prolapse that failed office procedures
• Patients prioritizing faster recovery and minimal postoperative wound care
• Select Grade IV cases if combined with other techniques (e.g., mucopexy); however, many Grade IV still require conventional surgery
Who may not be ideal candidates?
• Large external hemorrhoids or significant skin tags (laser shrinkage has limited value externally)
• Complicated disease: strangulated or thrombosed hemorrhoids, anal fissure/fistula requiring different operations
• Severe prolapse requiring tissue removal (stapled hemorrhoidopexy or excisional techniques may be better)
Unique insight: Think of laser as a “tissue remodeler” rather than a “tissue remover.” It’s great for shrinking internal cushions and reducing blood flow while sparing sensitive anoderm, which explains the lower pain scores. But because tissue is not fully removed, recurrence risk can be modestly higher than with excisional hemorrhoidectomy in some series—an important trade-off to discuss with your surgeon.
Types of Laser Procedures for Hemorrhoids
Several laser modalities and techniques are used, often with diode lasers at 980 nm or 1470 nm wavelengths, chosen for their absorption profiles in water and hemoglobin.
Laser Hemorrhoidoplasty (LHP)
• Technique: A small puncture allows a side-firing or radial fiber to deliver laser energy within the hemorrhoidal cushion. The thermal effect collapses vascular channels and shrinks the tissue from inside.
• Indications: Grade II–III internal hemorrhoids with bleeding/prolapse; sometimes combined with mucopexy (lifting sutures) for better prolapse control.
• Benefits: Less postoperative pain, minimal wounds, quick recovery; can be repeated if needed.
• Considerations: May require adjuncts for significant prolapse; recurrence or need for reintervention can be higher than with full excision.
HeLP (Hemorrhoidal Laser Procedure)
• Technique: Laser coagulates distal branches of the superior rectal artery feeding the hemorrhoids. Some centers use Doppler to locate arterial points, similar in concept to HAL/THD but with laser energy instead of sutures.
• Indications: Primarily Grade II–III with bleeding; less suited for large external components.
• Benefits: Reduced bleeding by cutting the “fuel supply”
• Considerations: Prolapse control may be limited; adjunct mucopexy or additional procedures might be needed.
Laser excision and combined approaches
• Some surgeons perform limited laser-assisted excisions of external components or combine LHP/HeLP with other procedures (e.g., RBL, mucopexy, skin tag removal) to tailor treatment.
• Wavelengths and fibers: Diode 980 nm vs 1470 nm; radial fiber disperses energy more evenly, potentially reducing focal thermal injury.
Choosing the right technique
• Bleeding-predominant Grade II–III: HeLP or LHP
• Prolapse-predominant Grade III: LHP plus mucopexy, or consider stapled hemorrhoidopexy/THD
• -Prominent external disease: excision-based approaches
Laser vs Other Treatments: What the Evidence Shows
Comparing advanced laser treatment for piles with other options helps set expectations.
Laser vs office procedures (RBL, sclerotherapy, infrared)
• Office procedures are cost-effective and work well for many Grade I–II cases, but recurrence can occur, and multiple sessions may be needed.
• Laser is generally used for more advanced Grade II–III or failed office procedures. It shows quicker recovery than excision but is more invasive than RBL/sclerotherapy.
Laser vs conventional hemorrhoidectomy
• Pain and recovery: Studies and guidelines report lower postoperative pain scores and earlier return to work with LHP versus excisional hemorrhoidectomy (Milligan–Morgan/Ferguson).
• Complications: Lower risk of significant bleeding and anal stenosis with LHP; urinary retention and minor bleeding can still occur.
• Recurrence: Conventional excision removes tissue and has the lowest recurrence, but at the cost of more pain and longer downtime. LHP shows slightly higher recurrence/reintervention in some series at mid-term follow-up.
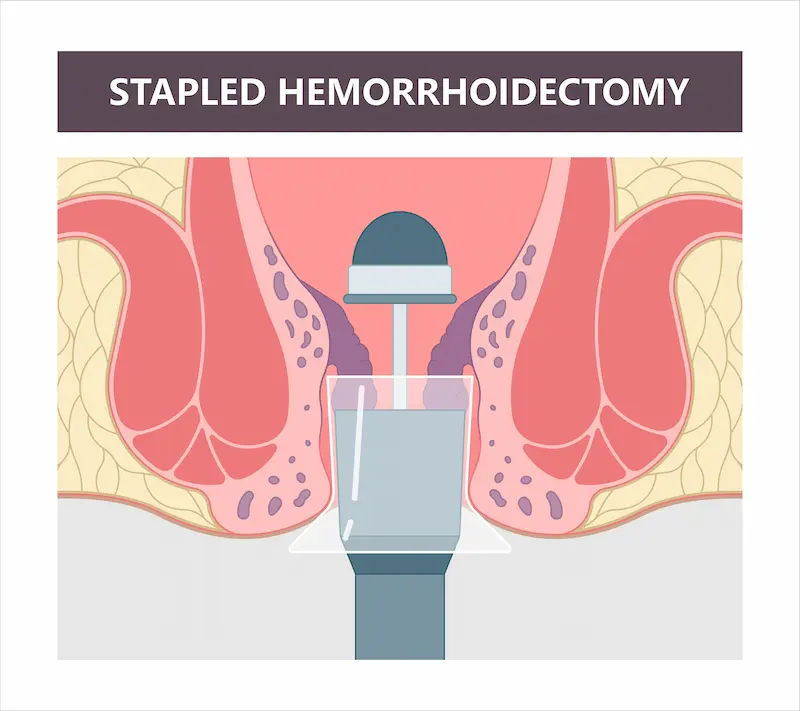
Laser vs stapled hemorrhoidopexy or Doppler-guided HAL/THD
• Stapled hemorrhoidopexy offers good prolapse correction with less pain than excision but can have unique complications (rare but serious) and costs more; recurrence varies.
• HAL/THD (arterial ligation with mucopexy) addresses blood flow and prolapse with favorable pain profiles; laser HeLP is analogous in concept. Comparative data are evolving; choice often depends on surgeon expertise and patient priorities.
At-a-glance outcomes (typical trends)
• Pain: Laser < stapled/HAL < excisional
• Recovery time: Laser often 3–7 days to routine activities; excisional 1–2+ weeks
• Recurrence/reintervention: Laser modestly higher than excisional in some studies; similar to HAL/THD in others
• Cost: Laser and stapled procedures generally cost more than RBL; costs vary widely by region and center
Safety, Risks, and Side Effects of Laser for Piles
While advanced laser treatment for piles is considered safe in experienced hands, every procedure has risks.
Common, usually short-term:
• Mild to moderate pain or discomfort for a few days
• Minor bleeding or spotting, especially during bowel movements
• Swelling, mucus discharge, or sensation of fullness
• Urinary retention on the day of surgery (more common in men)
Less common:
• Secondary bleeding (typically 7–10 days post-op)
• Infection or abscess (rare)
• Anal fissure due to hard stools and straining
• Temporary urgency or frequency changes
Rare:
• Anal stenosis or incontinence (much rarer with LHP vs extensive excision since anoderm is spared)
• Thrombosis of external hemorrhoids if the external components are prominent
Recurrence and reintervention:
• LHP and HeLP have good symptom control for Grade II–III, but some studies show higher recurrence than conventional excision at 1–3 years. Reintervention might be needed in a minority of patients, often using office procedures or repeat laser.
How to minimize risks:
• Choose an experienced colorectal or proctology surgeon familiar with both laser and non-laser options
• Optimize bowel habits pre- and post-op: fiber, fluids, stool softeners
• Avoid straining and heavy lifting for 1–2 weeks
• Follow postoperative care closely; if bleeding increases, contact your surgeon. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7.
Cost, Insurance, and Value for Money
Cost varies by city, hospital type, surgeon expertise, grade of hemorrhoids, anesthesia, and whether combined procedures are needed.
Cost factors
• Grade and complexity (more bundles or combined mucopexy increase costs)
• Anesthesia (spinal vs general), operating time, disposables (laser fibers are single-use)
• Hospital type (corporate vs smaller centers), location, and insurance coverage
Typical price ranges in India
• As a broad ballpark, daycare laser treatment for piles may range from INR 45,000 to 120,000 or more in metro cities, depending on the factors above. This can be higher than rubber band ligation and comparable to or slightly more than stapled procedures in many centers.
• Insurance: Policies may cover medically indicated surgical treatment for hemorrhoids. Confirm pre-authorization and coding (e.g., laser hemorrhoidoplasty vs hemorrhoidectomy).
Is laser “worth it”?
• If your top priorities are lower pain and faster return to routine, laser offers value.
• If your priority is the lowest recurrence risk for very advanced disease (e.g., large Grade IV with external components), a conventional approach might be more definitive.
• A frank discussion about your symptoms, goals, and budget with a trusted surgeon is key.
Preparing for Laser Surgery
Good preparation ensures smoother recovery and better outcomes.
Pre-operative evaluation
• Clinical exam with anoscopy or proctoscopy to confirm grade and rule out other issues (fissure, fistula, polyps)
• Review of medical history (bleeding disorders, diabetes, heart disease), medications (blood thinners, antiplatelets)
• Lab tests as needed: CBC, coagulation profile, blood sugar. Apollo 24|7 offers convenient home collection for tests like CBC or HbA1c if you’re optimizing diabetes before surgery.
Bowel prep and medications
• Many surgeons recommend a gentle enema or laxative the night before/day of surgery
• Fasting as instructed (usually 6–8 hours)
• Adjust blood thinners with your physician’s guidance
• Begin fiber supplement and hydration a few days prior
What to arrange?
• A companion for same-day discharge
• Comfortable, loose clothing, sanitary pads, sitz bath setup at home
• Pain medications and stool softeners as prescribed
Step-by-Step: What Happens on the Day?
Knowing what to expect can ease anxiety.
Anesthesia options
• Spinal or short general anesthesia is common. Your anesthesiologist will advise based on health status and surgeon preference.
Procedure steps (example: LHP)
• Positioning and antiseptic prep
• Gentle dilation and identification of hemorrhoidal cushions (usually 3 main bundles)
• Tiny puncture to insert a radial laser fiber into each cushion
• Controlled delivery of energy to shrink tissue and reduce blood flow
• Compression, optional sutures if needed; typically, minimal open wounds
• Total time: roughly 20–45 minute,s depending on complexity
Daycare discharge
• Observation for a few hours
• Oral fluids, pain control, instructions on sitz baths and stool softeners
• Discharge the same day in most cases; avoid driving yourself
Unique insight: Ask your surgeon how many laser cases they perform monthly and whether they also offer non-laser options. The best choice is individualized—not every Grade III needs a laser, and not every Grade IV needs excision.
Recovery Timeline and Aftercare
A realistic recovery roadmap helps you plan and spot problems early.
Pain control and activity
• Most patients describe mild to moderate pain for 2–5 days; pain after laser treatment for hemorrhoids is often manageable with oral analgesics and local measures
• Start sitz baths (warm water) 2–3 times daily from day 1
• Walk gently the same day; avoid heavy lifting for 1–2 weeks
• Return to desk work in 3–7 days for many; strenuous activity after 2–3 weeks
Diet, stool softeners, and hydration
• High-fiber diet (25–35 g/day) with fruits, vegetables, whole grains; consider psyllium or methylcellulose
• 2–2.5 liters of water per day (unless restricted)
• Stool softener for 1–2 weeks; avoid straining; consider a footstool for optimal toilet posture
• Short course of topical anesthetic or anti-inflammatory as advised
What’s normal vs red flags
• Normal: scant bleeding or spotting, mucus, mild swelling, low-grade discomfort
• Call your surgeon if: heavy bleeding, fever, severe pain not controlled by meds, urinary retention, foul discharge
• If you experience persistent heavy bleeding or symptoms that don’t settle within a week, consult a doctor online with Apollo 24|7 or book a physical visit for review.
Laser hemorrhoidoplasty recovery time
• Many resume usual routines within a week; full healing continues over 3–4 weeks as tissue contracts and remodels.
Real-World Outcomes: Case Snapshots
Case 1: Grade II bleeding-predominant
Ritika, 34, had intermittent bright red bleeding for 6 months despite fiber and RBL. LHP was performed on three cushions. She went home the same day, reported mild discomfort for 3 days, and returned to work on day 5. At 6 months, no recurrent bleeding. Example illustrates laser’s strength for bleeding-predominant Grade II that failed office treatment.
Case 2: Grade III prolapse
Arun, 46, had prolapse requiring manual reduction and mucus discharge. He underwent LHP with limited mucopexy. Pain was tolerable on oral analgesics; he returned to desk work in a week. Mild prolapse persisted early but improved over 8 weeks as shrinkage continued. At 1 year, occasional fullness but no bleeding and no reintervention.
Case 3: Postpartum hemorrhoids with external tags
Meera, 29, had mixed hemorrhoids and large external tags after pregnancy. Laser alone was not ideal. She underwent a tailored plan: removal of symptomatic tags and internal laser shrinkage. Recovery included more external wound care, but pain was still less than full excision. Symptom relief was achieved; highlights the need for personalized combinations.
Lifestyle Changes to Prevent Recurrence
Even the best advanced laser treatment for piles works better when supported by healthy habits.
Fiber, fluids, and toilet habits
• Aim for 25–35 g fiber; add a soluble fiber supplement if diet falls short
• Hydrate well; avoid prolonged sitting on the toilet; respond promptly to bowel urges
• Use a footstool to straighten the anorectal angle and reduce straining
Managing constipation and comorbidities
• Review medications that cause constipation (iron, some painkillers)
• Regular activity improves bowel motility
• Control diabetes and weight; both influence healing and recurrence risk
• Consider a stool diary to track patterns and triggers
Pelvic floor care and soothing measures
• Sitz baths reduce spasm and discomfort
• Gentle pelvic floor relaxation techniques can reduce straining
• Avoid harsh wipes; choose lukewarm water cleanse and pat dry
How to Choose the Right Surgeon and Center?
Your outcome depends heavily on skill, case selection, and aftercare.
Questions to ask
• Do I need a laser, or would RBL/stapled/THD/excision be better for my grade?
• What are my realistic risks of recurrence vs pain and recovery time?
• How many laser procedures do you perform monthly? What are your outcomes?
Credentials and technology
• Colorectal or proctology training, experience across multiple modalities
• Modern equipment (e.g., 1470 nm radial fiber) and adherence to safety protocols
• Transparent discussion on costs, disposables, and contingency plans
Apollo network and access
• Many large hospital networks, including the Apollo system, offer minimally invasive proctology services. If you need a personalized opinion or second look at imaging and test results, consult a doctor online with Apollo 24|7. They can also arrange referrals for in-person evaluation when needed.
Myths and Facts about Laser Treatment for Piles
“Laser is completely painless”
• Myth. It’s usually less painful than excision, but mild to moderate discomfort for a few days is typical.
“Laser guarantees no recurrence”
• Myth. Recurrence can occur, especially with higher grades or if habits don’t change. Laser’s strength is lower pain and quick recovery; excision can have lower recurrence for severe disease.
“Laser is the only modern option”
• Myth. Stapled hemorrhoidopexy and HAL/THD are also minimally invasive. The best choice depends on your anatomy, symptoms, and goals.
Consult a Top General Physician
Conclusion
Advanced laser treatment for piles offers a compelling blend of lower pain, minimal wounds, and rapid recovery—especially for Grade II–III internal hemorrhoids that haven’t responded to conservative care or office procedures. Laser techniques like LHP and HeLP work by shrinking hemorrhoidal cushions and reducing blood flow, which often means faster return to normal life with less need for strong painkillers. That said, they’re not a one-size-fits-all solution. For very large prolapse or significant external disease, stapled procedures, HAL/THD, or conventional hemorrhoidectomy may offer more definitive results, albeit with more discomfort and downtime.
The best choice depends on your symptoms, anatomy, priorities, and budget. Partner with an experienced colorectal or proctology surgeon who offers multiple modalities and can walk you through risks, benefits, costs, and realistic outcomes. If symptoms persist beyond two weeks or you want a second opinion, consult a doctor online with Apollo 24|7 for personalized guidance and, if needed, coordinated in-person care. With the right plan and support, most people achieve lasting relief and can prevent recurrence with smart lifestyle changes.
Consult a Top General Physician

Dr. Ajay K Sinha
General Physician/ Internal Medicine Specialist
30 Years • MD, Internal Medicine
Delhi
Apollo Hospitals Indraprastha, Delhi
(200+ Patients)

Dr. Sudhashree R
General Physician/ Internal Medicine Specialist
13 Years • MBBS, MRCEM
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Dr P Sai Avinash
General Physician/ Internal Medicine Specialist
7 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(425+ Patients)
Consult a Top General Physician

Dr. Ajay K Sinha
General Physician/ Internal Medicine Specialist
30 Years • MD, Internal Medicine
Delhi
Apollo Hospitals Indraprastha, Delhi
(200+ Patients)

Dr. Sudhashree R
General Physician/ Internal Medicine Specialist
13 Years • MBBS, MRCEM
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Dr P Sai Avinash
General Physician/ Internal Medicine Specialist
7 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(425+ Patients)
More articles from Piles
Frequently Asked Questions
1) Is advanced laser treatment for piles painful?
Most patients report less pain than with conventional hemorrhoidectomy. Expect mild to moderate discomfort for a few days, managed with oral analgesics and sitz baths.
2) What is the laser hemorrhoidoplasty recovery time?
Many return to routine activities within 3–7 days; full tissue remodeling continues for 3–4 weeks. Avoid heavy lifting for 1–2 weeks.
3) What are common piles of laser treatment side effects?
Minor bleeding, swelling, or mucus discharge for a few days; urinary retention on the day of surgery; rare complications include secondary bleeding or infection.
4) How does a laser compare with rubber band ligation?
Rubber band ligation is effective and cheaper for many Grade I–II cases but may need multiple sessions. Laser is more suitable for Grade II–III or failed office procedures, offering faster recovery than excision.
5) What is the recurrence after laser piles surgery?
Recurrence can occur, particularly with higher grades or if bowel habits don’t improve. Some studies show slightly higher reintervention rates versus excision, but laser balances lower pain with acceptable control for many Grade II–III cases.


.webp)