What Causes PCOS Unpacking the Signs of Polycystic Ovary Syndrome
Know about PCOS, what it is, common signs and symptoms, diagnosis, risks and more.

Written by Dr. Siri Nallapu
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
Have you been struggling with irregular periods, unexpected weight gain, or acne that just won’t quit? You’re not alone. These frustrating signs are often the first clues pointing to Polycystic Ovary Syndrome (PCOS), a common but frequently misunderstood hormonal disorder affecting millions of women worldwide. PCOS is more than just a reproductive issue; it's a complex metabolic condition that can impact your entire well-being. But what exactly triggers these symptoms? Is it genetics, lifestyle, or something else entirely? This article will demystify the root causes of PCOS, break down the science behind its most common signs, and guide you through the steps toward diagnosis and effective management. Understanding the "why" is the first powerful step toward taking control of your health.
What Exactly is Polycystic Ovary Syndrome (PCOS)?
Polycystic Ovary Syndrome (PCOS) is one of the most prevalent endocrine disorders among women of reproductive age, affecting approximately 1 in 10 globally. Despite its name, the condition is defined by a set of symptoms rather than just the presence of cysts.
More Than Just Ovarian Cysts
The term "polycystic" refers to the appearance of the ovaries on an ultrasound scan, where numerous small, fluid-filled sacs (follicles) surround the eggs. However, it's crucial to note that some women with PCOS do not have these cysts, and having cysts doesn't automatically mean you have PCOS. The syndrome is primarily characterised by a hormonal imbalance that disrupts ovulation and leads to a variety of symptoms.
Consult a Gynaecologist for Personalised Advice
A Whole-Body Metabolic Condition
Modern medicine recognises PCOS as a metabolic disorder as much as a reproductive one. The core issue often lies in how the body processes insulin, the hormone that regulates blood sugar. This insulin dysregulation has a domino effect, disrupting other hormones and leading to the wide-ranging symptoms associated with the condition. This is why managing PCOS often involves addressing metabolic health through diet and lifestyle modifications.
The Most Common Signs and Symptoms of PCOS
The presentation of PCOS varies significantly from person to person, but most diagnoses are based on a combination of a few key signs.
Irregular Periods and Fertility Challenges
The most common sign is infrequent, irregular, or prolonged menstrual cycles (a condition known as oligomenorrhea). This happens because the hormonal imbalance prevents the ovaries from releasing an egg regularly (anovulation). This is why infertility in women with PCOS is a common concern, as predictable ovulation is essential for conception.
Signs of Excess Androgens (Hyperandrogenism)
High levels of male hormones (androgens) are a hallmark of PCOS. This can lead to:
1. Hirsutism: Excess facial and body hair (e.g., on the chin, chest, back).
2. Severe acne: Often persistent and on the lower face, jawline, and back.
3. Androgenic alopecia: Thinning of hair on the scalp, similar to male-pattern baldness.
Metabolic Symptoms: Weight Gain and Insulin Resistance
Up to 80% of women with PCOS are overweight or obese, and many find it exceptionally difficult to lose weight. This is closely tied to insulin resistance, where the body's cells don't respond effectively to insulin. The pancreas then produces more insulin to compensate, and this excess insulin is believed to boost androgen production, creating a vicious cycle. This often leads to weight accumulation, particularly around the abdomen ("PCOS belly").
The Root Causes: What Triggers PCOS?
The exact cause of PCOS remains unknown, but research points to several key interconnected factors.
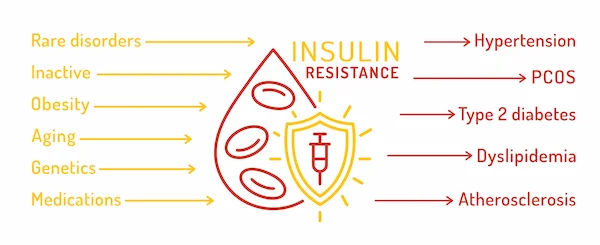
Insulin Resistance: The Fuel in the Engine
This is considered a primary driver. When cells become resistant to insulin, blood sugar levels can rise, and the body pumps out more insulin. High insulin levels are thought to:
1. Increase androgen production from the ovaries.
2. Disrupt the pituitary gland's signals that trigger ovulation.
3. Contribute to weight gain, further exacerbating insulin resistance.
Hormonal Imbalance: The Androgen Overproduction
The ovaries of women with PCOS often produce excess androgens. This is directly linked to the physical signs like hirsutism and acne, and plays a major role in preventing ovulation.
Low-Grade Inflammation: The Silent Spark
Women with PCOS often have chronic low-grade inflammation. This inflammation stimulates the ovaries to produce androgens and is also linked to insulin resistance and cardiovascular problems.
The Genetic Link: Is PCOS Hereditary?
PCOS often runs in families. If your mother, sister, or aunt has it, your risk is higher. Research is ongoing to identify specific genes linked to the condition, suggesting a strong hereditary component.
How is PCOS Officially Diagnosed?
There is no single test for PCOS. Diagnosis typically follows the Rotterdam Criteria, where a person must exhibit at least two of the following three features:
1. Irregular or absent periods.
2. Signs of high androgens (either from blood tests or physical symptoms like hirsutism).
3. Polycystic ovaries on an ultrasound scan.
Your doctor will also rule out other conditions that can cause similar symptoms, such as thyroid disease or elevated prolactin.
Potential Long-Term Health Risks of Untreated PCOS
Managing PCOS is crucial not only for immediate symptoms but also for preventing serious long-term health complications.
1. Type 2 Diabetes: Over 50% of women with PCOS will develop diabetes or pre-diabetes before age 40 due to insulin resistance.
2. Cardiovascular Disease: High insulin, cholesterol, and blood pressure levels increase the risk of heart disease and stroke.
3. Endometrial Hyperplasia: Without regular periods, the uterine lining can build up over time, increasing the risk of endometrial cancer.
4. Mental Health: The physical symptoms and hormonal fluctuations can contribute to anxiety, depression, and poor self-esteem.
Managing PCOS: Treatment and Lifestyle Strategies
While there's no cure, PCOS symptoms can be effectively managed through a combination of approaches.
1. Medical Interventions: Birth control pills can regulate cycles and reduce androgen levels. Metformin improves insulin sensitivity. Fertility medications like clomiphene can induce ovulation.
2. Diet and Nutrition: A low-glycemic index diet rich in whole foods, lean protein, and healthy fats helps manage insulin levels. If your condition does not improve after trying these methods, consult a doctor online with Apollo24|7 for a personalised nutrition plan.
3. Exercise: Regular physical activity, especially a mix of cardio and strength training, is a powerful tool for improving insulin sensitivity and aiding weight management.
Conclusion
Understanding the root causes of Polycystic Ovary Syndrome is empowering. It moves the conversation from blaming oneself for symptoms like weight gain to understanding the underlying metabolic and hormonal mechanisms at play. While the interplay of genetics, insulin resistance, and inflammation is complex, it also provides clear targets for management. A diagnosis of PCOS is not a life sentence of poor health; rather, it's a roadmap that highlights the areas where your body needs the most support. By adopting a proactive approach through informed lifestyle choices and working closely with healthcare professionals, you can effectively manage the signs of PCOS, significantly reduce your risk of long-term complications, and reclaim your health and well-being.
Consult a Gynaecologist for Personalised Advice
Consult a Gynaecologist for Personalised Advice

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata

Dr. Somdutta Basu
Obstetrician and Gynaecologist
7 Years • MBBS, MS Obstetrics & Gynaecology
Bansdroni
Siddhita Healthcare., Bansdroni

Dr. Neetu Singh
Obstetrician and Gynaecologist
19 Years • MBBS , MD (Obstetrics & Gynaecology)
Ghaziabad
Mother And Kidz Clinic, Ghaziabad

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Barasat
Diab-Eat-Ease, Barasat

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli
Consult a Gynaecologist for Personalised Advice

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata

Dr. Somdutta Basu
Obstetrician and Gynaecologist
7 Years • MBBS, MS Obstetrics & Gynaecology
Bansdroni
Siddhita Healthcare., Bansdroni

Dr. Neetu Singh
Obstetrician and Gynaecologist
19 Years • MBBS , MD (Obstetrics & Gynaecology)
Ghaziabad
Mother And Kidz Clinic, Ghaziabad

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Barasat
Diab-Eat-Ease, Barasat

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli
More articles from Polycystic ovary syndrome
Frequently Asked Questions
1. Can you have PCOS without having cysts in your ovaries?
Yes, absolutely. According to the Rotterdam diagnostic criteria, you only need to exhibit two of the three key features. Many women are diagnosed with PCOS based on irregular periods and high androgen levels, without having the classic polycystic ovary appearance on an ultrasound.
2. What is the main difference between PCOD and PCOS?
The terms are often used interchangeably, but there is a subtle distinction. PCOD (Polycystic Ovarian Disease) is often used to describe a condition where the ovaries contain multiple cysts and may have mild symptoms. PCOS (Syndrome) is a more severe metabolic-endocrine disorder with a wider range of symptoms and long-term health implications, including stronger associations with insulin resistance.
3. Does PCOS mean I can never get pregnant?
No, a PCOS diagnosis does not mean you cannot get pregnant. It means you may face challenges with ovulation, which is necessary for conception. However, with proper management—including lifestyle changes, medications to induce ovulation (like clomiphene or letrozole), and sometimes IVF—many women with PCOS successfully conceive and have healthy pregnancies.
4. Can lifestyle changes alone reverse PCOS?
Lifestyle changes are the first-line and most effective treatment for managing PCOS, especially if driven by insulin resistance. For many, losing even 5-10% of body weight can restore ovulation, regulate periods, and significantly improve symptoms. However, 'reversal' is not always the goal; effective long-term management is key, and some may still require medical support.
5. At what age do PCOS symptoms typically start?
Symptoms often first appear in late adolescence or early adulthood, around the time of your first period or shortly after. However, they can also develop later in response to significant weight gain. Many women don't receive a diagnosis until they struggle to conceive in their 20s or 30s.