Guide to All About Polycythemia Vera
Learn everything about Polycythaemia Vera (PV)—a rare chronic blood cancer. Understand symptoms, causes, diagnosis, treatment, and self-management for better health.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
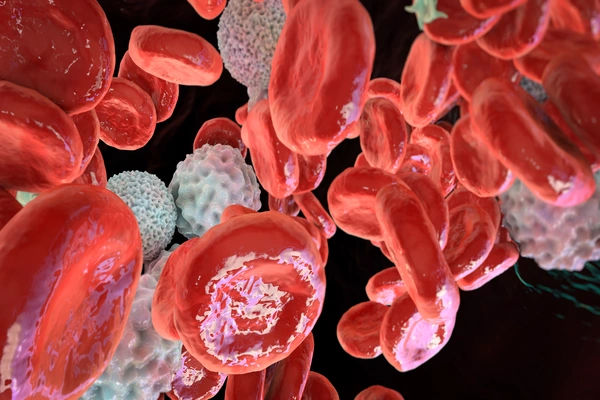
Imagine your body's production factory for blood cells going into overdrive, manufacturing too many red blood cells, and often white blood cells and platelets too. This is the reality of Polycythaemia Vera (PV), a rare and chronic type of blood cancer known as a myeloproliferative neoplasm. Unlike some cancers, PV is typically manageable with modern treatment, allowing most people to live a full and active life. However, understanding this condition is crucial because, if left untreated, the thickened blood can lead to serious complications like blood clots, stroke, or heart attack. This guide will walk you through everything you need to know—from decoding the often-misleading polycythaemia vera symptoms like debilitating itching after a warm shower to the latest diagnostic tests and treatment strategies. Our goal is to empower you with knowledge, reduce anxiety, and highlight the importance of partnering with your healthcare team for effective long-term management.
What is Polycythaemia Vera?
Polycythaemia Vera (PV) is a rare, slow-growing blood cancer where the bone marrow produces an excessive amount of blood cells, primarily red blood cells. This overproduction thickens your blood, slowing its flow and increasing the risk of clotting. It's one of a related group of blood disorders known as myeloproliferative neoplasms (MPNs), where the body's blood-forming cells malfunction.
Understanding Your Blood and Bone Marrow
To understand PV, it helps to know how blood is made. Your bone marrow, the spongy tissue inside your bones,
contains haematopoietic stem cells. These are "mother" cells that mature into red blood cells (carrying oxygen), white blood cells (fighting infection), and platelets (clotting blood). In PV, a genetic mutation causes one of these stem cells to reproduce uncontrollably, leading to a surplus of these cells, especially red blood cells.
Is Polycythaemia Vera a Cancer?
Yes, Polycythaemia Vera is classified as a cancer because it involves the uncontrolled growth of abnormal cells originating in the bone marrow. However, it's important to note that it is a chronic cancer, often managed successfully for decades. Many people think of cancer as always being rapidly progressive, but PV defies that stereotype, behaving more like a manageable chronic illness for most patients.
Recognising the Signs: Polycythaemia Vera Symptoms
Many people with PV have no symptoms initially, and it's sometimes discovered accidentally during a blood test for another reason. When symptoms do appear, they are often caused by the thicker, slower-moving blood.
Common Early Symptoms
- Headaches, Dizziness, and Weakness: Thick blood doesn't deliver oxygen as efficiently to the brain.
- Itching (Pruritus): A classic and distressing PV symptom is severe itching, especially after a warm bath or shower. This is believed to be related to abnormal histamine release.
- Ruddy Complexion: The excess red blood cells can cause a reddish or purplish appearance of the skin, particularly on the face, palms, and feet.
- Burning or Tingling Sensations: In the hands or feet.
- Fatigue: Severe and persistent tiredness is extremely common.
- Shortness of Breath: Especially when lying down.
- Blurred Vision or Blind Spots.
Serious Symptoms and Complications
- Enlarged Spleen (Splenomegaly): The spleen works to filter blood and remove old cells. In PV, it becomes overworked and enlarged, which can cause a feeling of fullness or pain under the left ribs.
- Bleeding Abnormalities: Despite having more platelets, some people experience unusual bleeding, like nosebleeds or bruising easily.
- Gout: High cell turnover can lead to elevated uric acid levels, causing painful gout attacks.
- Blood Clots (Thrombosis): This is the most serious risk, potentially leading to deep vein thrombosis (DVT), pulmonary embolism (PE), stroke, or heart attack.
What Causes Polycythaemia Vera?
The exact trigger for PV is unknown, but it almost always starts with a genetic mutation acquired during a person's
lifetime (it is not typically inherited from parents).
The Role of the JAK2 Gene Mutation
In over 95% of cases, the driver is a mutation in the JAK2 gene. This gene is like an "on switch" for blood cell
production. The mutation (most commonly JAK2 V617F) jams this switch in the "on" position, causing the bone
marrow to produce blood cells non-stop, regardless of the body's actual needs.
Other Associated Genetic Mutations
A small number of people without the JAK2 mutation have mutations in other genes, like CALR or MPL. Genetic testing helps confirm the diagnosis and can sometimes provide prognostic information.
Risk Factors: Who is Most Likely to Get PV?
- Age: Risk increases with age; most diagnoses occur around age 60.
- Sex: Men are slightly more likely to develop PV than women.
- History of Blood Clots: A personal or family history can be a factor, though not a direct cause.
How is Polycythaemia Vera Diagnosed?
Diagnosis involves piecing together clues from symptoms, blood tests, and sometimes bone marrow examination. If you're experiencing persistent symptoms like unexplained itching or headaches, consult a doctor online with Apollo24|7 for an initial evaluation and to see if blood tests are warranted.
Blood Tests: The First Step
- Complete Blood Count (CBC): This is crucial. It will show elevated haematocrit (percentage of red blood cells),
haemoglobin, and often elevated white blood cell and platelet counts. - Erythropoietin (EPO) Level: EPO is a hormone that stimulates red blood cell production. In PV, the level is usually very low because the body doesn't need to make more—it already is.
The Bone Marrow Biopsy
This procedure involves taking a small sample of bone marrow, usually from the hip bone, for analysis. It can show the hypercellularity (overcrowding) of the marrow, which is characteristic of PV, and help rule out other MPN blood
disorders.
Genetic Testing for JAK2
A blood test can confirm the presence of the JAK2 mutation, which is a major criterion for diagnosis. Apollo24|7 offers convenient home collection for a wide range of blood tests, including genetic panels, making the diagnostic process smoother.
Polycythaemia Vera Treatment Options
There is no cure for PV, but treatments are highly effective at controlling the disease, managing symptoms, and
preventing complications. The goal is to reduce the risk of thrombosis and improve quality of life.
Phlebotomy: The Cornerstone Therapy
This is the first line of treatment. Similar to donating blood, a pint of blood is removed from your body regularly to lower your red blood cell count and haematocrit. The goal is to keep the haematocrit below 45% for men and 42% for women.
Medications to Reduce Blood Cell Counts
For patients at high risk for clotting or who need frequent phlebotomies, medication is added:
- Hydroxyurea: A common oral chemotherapy drug that suppresses bone marrow production.
- Ruxolitinib (Jakafi): A targeted therapy that specifically inhibits the malfunctioning JAK2 pathway. It's used if hydroxyurea is ineffective or not tolerated and is excellent for controlling an enlarged spleen and severe itching.
- Interferon-alpha: A biologic therapy that can help normalise blood counts and may target the mutated stem cells.
Managing Symptoms and Itching (Pruritus)
Antihistamines are often tried first. Other options include SSRI antidepressants (like paroxetine) or phototherapy, which have been found to help with stubborn itching.
Low-Dose Aspirin Therapy
Almost all PV patients take a daily low-dose aspirin to reduce the risk of blood clots by preventing platelets from
sticking together.
Living with Polycythaemia Vera
A diagnosis can be overwhelming, but active self-management is key to thriving.
Diet and Lifestyle Modifications
- Stay well-hydrated to help keep blood from thickening.
- Exercise regularly to promote healthy blood flow (consult your doctor first).
- Avoid tobacco, which constricts blood vessels and increases clotting risk.
- Be cautious with activities that could cause injury and bleeding.
The Importance of Regular Monitoring
PV is a lifelong condition requiring consistent follow-up with a haematologist. Regular blood tests are essential to
ensure your counts are in the target range and to monitor for any potential progression of the disease.
Prognosis and Life Expectancy
With modern treatment, the life expectancy for many PV patients can be nearly normal. The key is diligent
management to prevent thrombotic events, which are the leading cause of illness.
Potential Complications of Untreated PV
Leaving PV untreated is dangerous. The primary risks are life-threatening blood clots (stroke, heart attack, pulmonary embolism). Over many years, a small percentage of cases can progress to more serious diseases like myelofibrosis (scarring of the bone marrow) or acute leukaemia.
Conclusion
Living with Polycythaemia Vera is a marathon, not a sprint. While the diagnosis of a chronic blood cancer can be daunting, it's important to focus on the highly effective management strategies available today. Through a combination of routine phlebotomy, modern medications, and proactive lifestyle choices, you can significantly reduce your risk of complications and maintain a high quality of life. The journey requires a strong partnership with your healthcare team and a commitment to regular monitoring. Remember, you are not alone. Connecting with support groups and patient advocacy organisations for myeloproliferative neoplasms can provide valuable resources and community. If you suspect you have symptoms or have been recently diagnosed, take the next step. Book a physical visit to a haematologist with Apollo24|7 to create a personalised and comprehensive management plan tailored to your specific needs.
More articles from Polycythemia vera
Frequently Asked Questions
What is the life expectancy for someone with polycythaemia vera?
With modern treatment and careful management, many people with PV have a life expectancy that is nearly normal. The prognosis is highly individual and depends on factors like age, overall health, and how well the disease is controlled to prevent clots.
Does polycythaemia vera always turn into leukaemia?
No, it does not always turn into leukaemia. Only a small percentage of PV cases (estimated at less than 10% over 20 years) may transform into acute leukaemia, which is often associated with later-stage disease or certain treatments. The primary focus is on preventing blood clots.
What is the most common first symptom of polycythaemia vera?
There is no single first symptom, and many are vague. However, persistent and severe itching after a warm shower or bath (aquagenic pruritus) is a classic and distinctive early sign that often leads to diagnosis.
Can polycythaemia vera be cured?
Currently, there is no cure for PV except for a potentially curative stem cell transplant. However, this procedure is high-risk and is only considered for a very small number of patients, typically those whose disease has progressed to leukaemia. For the vast majority, it is a chronic condition managed with long-term treatment.
What foods should be avoided with polycythaemia vera?
There's no specific 'PV diet,' but it's generally advised to avoid foods high in iron (like red meat and iron-fortified cereals) as iron helps produce red blood cells. Staying hydrated and maintaining a heart-healthy diet low in saturated fats is recommended to support overall cardiovascular health and reduce clotting risk.