Sarcoidosis Symptoms: What Triggers This Inflammatory Condition?
Discover the symptoms, causes, and triggers of sarcoidosis—an inflammatory condition that forms granulomas in organs like the lungs, skin, and eyes. Learn about risk factors, diagnosis, treatment, and complications.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026
Introduction
Sarcoidosis is a complex and often misunderstood condition characterised by the growth of tiny collections of inflammatory cells, called granulomas, in various parts of the body. While these granulomas can form in any organ, they most commonly affect the lungs and lymph nodes. For the general public, the journey begins with noticing puzzling signs of sarcoidosis—a persistent cough, mysterious skin lesions, or overwhelming fatigue—that don't have an obvious cause. This article will demystify this condition, exploring not just the wide array of symptoms it can present but, crucially, delving into what researchers believe leads to its development. We'll break down the current theories on triggers, risk factors, and the steps you can take if you suspect you might be affected, providing a clear roadmap for understanding this inflammatory enigma.
What is Sarcoidosis? Understanding the Body's Misdirected Response
At its core, sarcoidosis is believed to be an autoimmune-like disorder. In simple terms, it's as if your body's defence system, your immune system, gets confused. Instead of only attacking foreign invaders like viruses and bacteria, it turns its fire on your own tissues and organs. This prolonged assault leads to inflammation and, eventually, the formation of the condition's signature feature: granulomas.
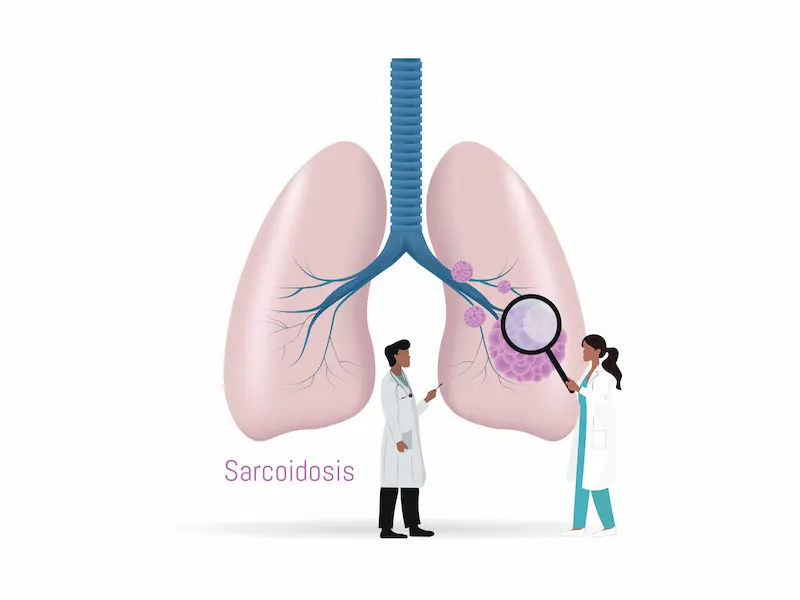
Granulomas: The Hallmark of Sarcoidosis
Think of a granuloma as a tiny, organised cluster of immune cells that wall off what the body perceives as a threat. In a healthy response, this is useful for isolating an infection, like in tuberculosis. However, in sarcoidosis, this process happens without a clear foreign substance to target. These granulomas can disrupt the normal structure and function of an organ. If they are small and few, you may have no symptoms. But if they grow, clump together, or are numerous, they can lead to significant organ damage and the wide range of sarcoidosis symptoms people experience.
The Primary Signs and Symptoms of Sarcoidosis
The presentation of sarcoidosis is incredibly varied. Some people have no symptoms at all (asymptomatic), and the condition is discovered incidentally on a chest X-ray taken for another reason. For others, symptoms appear suddenly and severely but resolve within a few years (acute). A third group develops symptoms gradually and suffer from a long-term (chronic) version of the disease.
General and Constitutional Symptoms
Often, the first clues are systemic and non-specific, meaning they affect the whole body. These include:
• Persistent fatigue: This is one of the most common and debilitating complaints, often disproportionate to the level of activity.
• Fever: Low-grade, unexplained fevers are common.
• Weight loss: Unintentional weight loss without dieting.
• Swollen lymph nodes: Particularly in the chest, neck, and armpits.
• Night sweats: Drenching sweats that disrupt sleep.
Symptoms by Affected Organ
Pulmonary Sarcoidosis (Lungs)
Over 90% of patients have lung involvement. Symptoms include:
• A persistent dry cough that won't go away.
• Shortness of breath (dyspnoea), especially during physical activity.
• Chest pain or a feeling of tightness in the chest.
• Wheezing.
Cutaneous Sarcoidosis (Skin)
Skin manifestations affect about 25% of patients and can be a key diagnostic clue:
• Erythema nodosum: Tender, red bumps or nodules that typically appear on the shins. This is often associated with a good prognosis.
• Lupus pernio: Purplish, firm sores on the nose, cheeks, and ears, which are more common in chronic disease.
• Rashes, scars that become raised, or small bumps under the skin.
Ocular Sarcoidosis (Eyes)
Eye involvement (uveitis) occurs in about 25-50% of cases and can sometimes be the first sign. It may cause:
• Blurred vision.
• Eye pain.
• Severe redness.
• Light sensitivity.
If untreated, it can lead to blindness, making early ophthalmologist consultation critical.
Cardiac Sarcoidosis (Heart)
Although less common, heart involvement is serious. It can cause:
• Heart palpitations or a fluttering sensation (arrhythmias).
• Lightheadedness or fainting (syncope).
• Shortness of breath.
• Chest pain.
• In severe cases, heart failure.
Other organs like the nervous system (neurosarcoidosis), liver, and kidneys can also be affected, leading to a diverse range of other symptoms of sarcoidosis.
What Leads to Sarcoidosis? The Search for a Cause
The million-pound question remains: what starts this process? The exact cause of sarcoidosis is unknown. However, the prevailing theory among researchers is that it develops in genetically predisposed individuals after exposure to a specific environmental trigger.Consult a Rheumatologist for Personalised Advice
The Immune System Theory: Friend Turned Foe
The leading hypothesis is that sarcoidosis results from an exaggerated immune response to an unknown substance. This could be an infectious agent (like certain bacteria or viruses), a chemical, dust, or even something in the environment. The immune system launches a full-scale attack, but for unknown reasons, it doesn't "turn off," leading to chronic inflammation and granuloma formation. This explains why treatments often focus on suppressing the immune response.
Genetic Predisposition and Family History
Sarcoidosis isn't directly inherited like some genetic disorders, but your genetic makeup plays a significant role in susceptibility. Having a first-degree relative (parent, sibling, or child) with the condition increases your risk. Certain genes are believed to influence how your immune system recognises and responds to potential threats, making some people more likely to develop the disease upon exposure to a trigger.
Environmental Triggers: The Role of Exposure
Researchers are actively trying to identify the specific environmental antigens that kick-start the process. Potential triggers that have been studied include:
• Mycobacteria: Certain types of bacteria, similar to those that cause tuberculosis.
• Propionibacterium acnes: A bacteria commonly found on the skin.
• Inorganic particles: Exposure to metals like aluminium, zirconium, or talc.
• Organic dust: Mould, pesticides, or other agricultural exposures.
It's likely that a combination of these factors, a specific trigger inhaled by a person with a specific genetic profile, is what leads to sarcoidosis.
Who is at Risk? Understanding Sarcoidosis Demographics
While anyone can develop sarcoidosis, certain patterns are clear:
• Age: It most commonly occurs between the ages of 20 and 40.
• Sex: Women are slightly more likely to be diagnosed than men.
• Race and Ethnicity: People of African and Scandinavian descent have a significantly higher incidence. African Americans often experience more severe, chronic, and extrapulmonary forms of the disease.
• Family History: As mentioned, having a family member with sarcoidosis increases your risk.
How is Sarcoidosis Diagnosed?
Diagnosing sarcoidosis can be challenging because its symptoms mimic so many other conditions. There is no single definitive test. It is often a diagnosis of exclusion. Doctors will typically use a combination of:
• Medical history and physical exam.
• Chest X-ray or CT scan: To look for granulomas in the lungs and swollen lymph nodes.
• Pulmonary function tests: To measure how well your lungs are working.
• Biopsy: A small sample of tissue (e.g., from the lung, skin, or a lymph node) is taken to look for granulomas under a microscope. This is often the key to confirmation.
• Blood tests: To check for elevated angiotensin-converting enzyme (ACE) levels, signs of inflammation, or to assess organ function.
• Other organ-specific tests: Such as an ECHO for the heart, an eye exam, or an MRI for neurological symptoms.
If you are experiencing a cluster of these unexplained symptoms, consulting a doctor online with Apollo24|7 is a good first step to discuss your concerns and determine if you need a specialist referral for further evaluation.
Treatment and Management: Living with Sarcoidosis
The approach to treatment is highly individualised. Many cases of acute sarcoidosis, especially those with erythema nodosum, resolve on their own without any intervention. Treatment is typically reserved for people with:
• Symptoms that significantly affect quality of life (e.g., severe fatigue, pain).
• Progressive lung or other organ involvement.
• Dangerous heart or nervous system involvement.
The mainstay of treatment is corticosteroids (like prednisolone) to reduce inflammation and suppress the overactive immune response. For chronic cases or those who can't tolerate steroids, other immunosuppressive medications (e.g., methotrexate) are used. Apollo24|7 offers convenient home collection for tests like those monitoring inflammation (ESR, CRP) or organ function, making it easier to manage your condition long-term.
Potential Complications of Untreated Sarcoidosis
When inflammation is severe and persistent, it can lead to permanent scarring (fibrosis) and organ damage. Key complications include:
• Pulmonary fibrosis: Irreversible lung scarring leading to chronic breathing problems.
• Vision loss: From untreated uveitis.
• Heart arrhythmias and failure: From cardiac scarring.
• Kidney failure: Due to high calcium levels or direct involvement.
• Neuropathy: Nerve damage from neurosarcoidosis.
This underscores the importance of proper diagnosis and monitoring, even in mild cases.
Conclusion
Understanding what leads to the signs of sarcoidosis is a journey into the complexities of the human immune system. While the precise trigger remains elusive, the medical community agrees it's a perfect storm of genetics meeting the right environmental factor. The wide array of symptoms means it can often be overlooked or misdiagnosed. If you are experiencing a constellation of unexplained, persistent symptoms—especially respiratory, skin, or eye issues coupled with deep fatigue—it is essential to seek medical advice. Early recognition and proper management are key to controlling inflammation, preserving organ function, and maintaining a good quality of life. If your condition does not improve after trying over-the-counter remedies, book a physical visit to a doctor with Apollo24|7 for a thorough evaluation and personalised care plan.Consult a Rheumatologist for Personalised Advice
Consult a Rheumatologist for Personalised Advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Ramineni Naga Tejaswini
Rheumatologist
3 Years • MBBS, DNB(Internal Medicine), DrNB ( Clinical Immunology and Rheumatology)
Hyderabad
Apollo Hospitals Jubilee Hills Hyderabad, Hyderabad

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Brig K Shanmuganandan
Rheumatologist
27 Years • MBBS, MD (Med.), DNB (Med.), Fellow (Rheuma.)
Chennai
Apollo Hospitals Greams Road, Chennai
(475+ Patients)

Dr. Sundeep Kumar Upadhyaya
Rheumatologist
30 Years • MBBS, MD, DM
Delhi
Apollo Hospitals Indraprastha, Delhi
(225+ Patients)
Consult a Rheumatologist for Personalised Advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Ramineni Naga Tejaswini
Rheumatologist
3 Years • MBBS, DNB(Internal Medicine), DrNB ( Clinical Immunology and Rheumatology)
Hyderabad
Apollo Hospitals Jubilee Hills Hyderabad, Hyderabad

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Brig K Shanmuganandan
Rheumatologist
27 Years • MBBS, MD (Med.), DNB (Med.), Fellow (Rheuma.)
Chennai
Apollo Hospitals Greams Road, Chennai
(475+ Patients)

Dr. Sundeep Kumar Upadhyaya
Rheumatologist
30 Years • MBBS, MD, DM
Delhi
Apollo Hospitals Indraprastha, Delhi
(225+ Patients)
More articles from Sarcoidosis
Frequently Asked Questions
1. Is sarcoidosis a form of cancer?
No, sarcoidosis is not cancer. It is an inflammatory disease. While both can cause masses or tumours, the granulomas of sarcoidosis are made of immune cells, not cancerous cells.
2. Can sarcoidosis be cured?
There is no known cure for sarcoidosis. However, many cases, especially acute ones, may resolve spontaneously. For chronic cases, the goal of treatment is to manage symptoms, control inflammation, and prevent organ damage, effectively putting the disease into remission.
3. What is the life expectancy for someone with sarcoidosis?
For the vast majority of people, sarcoidosis does not affect life expectancy. Most people with the disease have a normal lifespan. The prognosis is worse only in a small minority of cases where there is severe, progressive damage to vital organs like the heart or lungs.
4. Are the skin rashes from sarcoidosis contagious?
No, the skin manifestations of sarcoidosis are a result of an internal inflammatory process and are absolutely not contagious. You cannot catch it from or spread it to another person through contact.
5. Does having sarcoidosis make me immunocompromised?
Not exactly. The disease itself involves an overactive, not underactive, immune system. However, the medications used to treat it (like corticosteroids) are immunosuppressants and can make you more susceptible to infections.