Silicosis: Causes, Symptoms and Prevention
Learn about silicosis, its causes, early symptoms, and effective prevention measures to protect your lungs and stay safe.

Written by Dr. Siri Nallapu
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
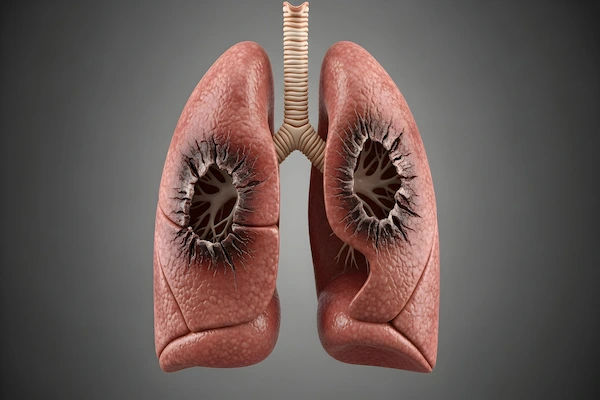
Silicosis is a serious and irreversible lung disease caused by breathing in tiny bits of silica, a common mineral found in sand, rock, and quartz. Often called a "hidden hazard," this disease primarily affects workers in industries like construction, mining, and manufacturing, but its signs can take years, even decades, to appear. Understanding what leads to the signs of silicosis disease is the first critical step toward prevention and early intervention. This article will guide you through the primary causes, detail the often-missed early symptoms, explain the different types of the disease, and, most importantly, outline how you can protect yourself. If you work in a high-risk field or have a persistent cough and shortness of breath, this information is vital for your long-term health.
What is Silicosis? The Basics of a Serious Lung Disease
Silicosis is a form of occupational pneumoconiosis, a group of lung diseases caused by inhaling certain dusts. In the case of silicosis disease, the culprit is crystalline silica dust. When these microscopic particles are inhaled, they travel deep into the lungs' air sacs (alveoli). The body's immune system recognizes them as foreign invaders and sends scavenger cells (macrophages) to engulf them. However, silica dust is toxic to these cells, causing them to die and release inflammatory substances. This process leads to inflammation and, over time, the formation of scar tissue (fibrosis) in the lungs. This scarring stiffens the lungs, making it increasingly difficult to breathe. Unlike some respiratory conditions, the lung damage from silicosis is permanent and progressive, meaning it continues to worsen even after exposure has stopped. It's a classic example of a preventable disease with no true cure, making awareness its most powerful antidote.
Consult a Pulmonologist for the best advice
The Primary Cause: How Silica Dust Damages Your Lungs
The root cause of silicosis disease is exclusively the inhalation of respirable crystalline silica (RCS) dust. This isn't about large, visible particles of dust but rather the fine, invisible dust that can be breathed deep into the lungs.
Understanding Crystalline Silica: The Invisible Threat
Crystalline silica is a common mineral found abundantly in the earth's crust. It becomes hazardous when materials containing it are cut, ground, drilled, crushed, or otherwise disturbed, creating dust. Common materials that contain silica include:
- Sand, sandstone, and topsoil
- Concrete and mortar
- Brick and block
- Granite, slate, and other natural stones
Artificial stone (engineered stone) used for countertops; this is particularly dangerous due to its very high silica content (often over 90%).
High-Risk Occupations and Industries
Any job that creates dust from these materials puts workers at risk.
Construction and Demolition Work
This is one of the largest at-risk sectors. Tasks like abrasive blasting (sandblasting), jackhammering, drilling into concrete, cutting bricks or blocks, and tunnelling operations generate enormous amounts of silica dust.
Mining and Quarrying Operations
Miners, drillers, and quarry workers are exposed to silica dust from breaking up rock and ore. This industry has a long and tragic history with silicosis disease.
Manufacturing and Fabrication Jobs
Workers who cut, grind, or polish natural or engineered stone countertops are at extremely high risk. Foundry workers, pottery and ceramics makers, and those involved in glass manufacturing also face significant exposure.
Recognising the Signs and Symptoms of Silicosis
The symptoms of silicosis disease can be subtle at first and are often mistaken for less serious conditions like a smoker's cough or general aging. This is why knowing the specific signs is crucial.
Early-Stage Symptoms: Don't Ignore the Warning Signs
In the earliest phases, particularly with chronic silicosis, symptoms may be mild or non-existent. As it progresses, the most common early signs include:
- A persistent, dry cough that doesn't go away.
- Shortness of breath (dyspnoea), initially only during physical exertion but eventually occurring at rest.
- Fatigue and general weakness.
- Occasional chest pain.
Many dismiss these as signs of being out of shape or a common cold, but for those with a history of exposure, they are critical red flags.
Progressive Symptoms: When the Disease Worsens
As lung scarring increases, symptoms become more severe and debilitating:
- Severe shortness of breath, even while sitting.
- A productive cough that may bring up phlegm.
- Fever.
- Weight loss and loss of appetite.
- Bluish discolouration of the lips (cyanosis) due to low oxygen levels.
The Three Types of Silicosis and Their Symptom Timelines
Understanding the types of silicosis is key to timely care.
Chronic Silicosis: The Most Common Form
This form occurs after 10+ years of low to moderate exposure. The progression is slow, and symptoms may take decades to become noticeable, often appearing after retirement.
Accelerated Silicosis: A Faster Progression
This results from higher levels of exposure over a shorter period (5-10 years). Symptoms develop more quickly and worsen at a faster rate than the chronic form.
Acute Silicosis: A Rapid and Severe Onset
This is the most dangerous form, occurring after just weeks or a few years of exposure to extremely high concentrations of silica dust. It causes severe inflammation and fluid buildup in the lungs, leading to rapidly progressive shortness of breath, low blood oxygen, and severe cough. This is a medical emergency.
How is Silicosis Diagnosed?
If you experience any early symptoms of silicosis and have a history of exposure, seeking a medical evaluation is essential.
The Importance of a Thorough Occupational History
The single most important clue for a doctor is your work history. Be prepared to detail all past jobs, the specific tasks you performed, the materials you worked with, and what, if any, protective measures were used.
Key Diagnostic Tests: Imaging and Lung Function
A doctor will likely order:
- Chest X-ray or CT Scan: These imaging tests are crucial for revealing the nodular scarring and patterns characteristic of silicosis. A high-resolution CT scan is more sensitive and can detect the disease earlier than a standard X-ray.
- Pulmonary Function Tests (PFTs): These breathing tests measure how well your lungs are working, often revealing a restrictive pattern where the lungs can't hold as much air as they should.
- Other tests may be used to rule out other conditions like tuberculosis (TB), which individuals with silicosis are more susceptible to.
If you have a history of silica exposure and a persistent cough, consult a doctor online with Apollo24|7 for an initial assessment and to discuss if further testing is needed.
Get Your Health Assessed
Treatment and Management of Silicosis
Learn about effective treatment options and management strategies to ease symptoms and improve quality of life for silicosis patients.
Is There a Cure? The Reality of Treatment Options
There is no cure for silicosis. The lung damage is irreversible. Therefore, the goal of treatment is not to reverse the disease but to manage symptoms, prevent complications, and improve quality of life.
Managing Symptoms and Improving Quality of Life
Treatment plans are supportive and may include:
- Stopping Exposure: The absolute first step is to avoid any further exposure to silica dust.
- Medication: Bronchodilators may help open airways, and corticosteroids can sometimes reduce inflammation.
- Oxygen Therapy: For those with low blood oxygen levels, supplemental oxygen can ease shortness of breath and prevent complications.
- Pulmonary Rehabilitation: This program teaches breathing techniques and exercises to improve daily functioning.
- Lung Transplant: In very severe and advanced cases, a lung transplant may be considered.
Early diagnosis of silicosis is key to accessing these management strategies before the disease severely impacts your life.
Prevention is the Only Cure: How to Avoid Silica Exposure
Since silicosis cannot be cured, prevention is everything. This responsibility falls on both employers and workers.
Employer Responsibilities: OSHA Regulations and Controls
Employers in industries with silica exposure are legally required (under OSHA's silica standards) to:
- Use engineering controls like water systems to suppress dust (wet-cutting) or vacuum systems to capture dust at the source (local exhaust ventilation).
- Provide proper respiratory protection when engineering controls cannot limit exposure adequately.
- Offer medical surveillance, including lung function tests and chest X-rays, for workers who are exposed above certain limits.
- Train workers on the hazards of silica and how to use controls properly.
Personal Protective Equipment (PPE) for Workers
When engineering controls aren't enough, using the right PPE is critical:
- Respirators: A properly fitted, NIOSH-approved respirator (like an N95 mask or a more powerful supplied-air respirator for high-exposure tasks) is essential. A dust mask is not sufficient.
- Work Clothes: Use disposable or washable work clothes to avoid carrying silica dust home to your family.
- Hygiene: Wash hands and face before eating, drinking, or smoking, and shower and change into clean clothes before leaving the worksite.
Conclusion
Silicosis is a devastating but entirely preventable disease. The path to its signs and symptoms is clear: prolonged inhalation of silica dust leads to irreversible lung scarring. While industries and regulations have a major role to play in protecting workers, individual awareness is the first line of defense. Recognising the early warning signs, that persistent cough and unexplained shortness of breath, and connecting them to your work history can lead to earlier diagnosis and better management outcomes. If you work with materials like concrete, stone, or sand, insist on and use all available safety measures. Your long-term health depends on the precautions you take today. If you are experiencing any symptoms of silicosis, do not wait. Consult a doctor online with Apollo24|7 to discuss your concerns and exposure history. Your lungs are irreplaceable; protecting them is paramount.
Consult a Pulmonologist for the best advice
Consult a Pulmonologist for the best advice

Dr. P Sravani
Pulmonology Respiratory Medicine Specialist
3 Years • MBBS, MD
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam
Dr. Ambuj Kumar
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS, MD (Pulmonary Medicine)
New Delhi
Smriti Gynaecology and Lung Centre, New Delhi

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. K Prasanna Kumar Reddy
Pulmonology Respiratory Medicine Specialist
16 Years • MBBS, DTCD (TB&CHEST), DNB (PULM MED), FCCP
Hyderabad
Apollo Medical Centre Kondapur, Hyderabad
Consult a Pulmonologist for the best advice

Dr. P Sravani
Pulmonology Respiratory Medicine Specialist
3 Years • MBBS, MD
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam
Dr. Ambuj Kumar
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS, MD (Pulmonary Medicine)
New Delhi
Smriti Gynaecology and Lung Centre, New Delhi

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. K Prasanna Kumar Reddy
Pulmonology Respiratory Medicine Specialist
16 Years • MBBS, DTCD (TB&CHEST), DNB (PULM MED), FCCP
Hyderabad
Apollo Medical Centre Kondapur, Hyderabad
Get Your Health Assessed
₹3229(₹8072)60% off
More articles from Silicosis
Frequently Asked Questions
Is silicosis fatal?
Yes, silicosis can be fatal, especially in its acute and advanced forms. It severely damages the lungs, leading to respiratory failure. It also significantly increases the risk of other deadly conditions like tuberculosis, lung cancer, and heart failure.
What is the life expectancy of someone with silicosis?
Life expectancy varies greatly depending on the type of silicosis, the level of exposure, overall health, and whether further exposure is stopped. Someone with mild chronic silicosis may have a near-normal life span if they avoid further dust exposure and manage their health, while acute silicosis can be fatal within months.
Can you get silicosis from one exposure?
It is highly unlikely. Silicosis is typically the result of repeated, long-term exposure. However, acute silicosis can develop after just a few weeks or months of exposure to extremely high concentrations of silica dust.
What is the difference between silicosis and COPD?
While both cause breathing difficulties, they have different causes. Silicosis is specifically caused by silica dust exposure. COPD (Chronic Obstructive Pulmonary Disease) is most commonly caused by smoking or long-term exposure to air pollutants. They can look similar on tests, so a detailed work history is key for a correct silicosis diagnosis.
Is silicosis the same as black lung?
No, they are similar but different diseases. Silicosis is caused by silica dust. Black lung disease (coal workers' pneumoconiosis) is caused by inhaling coal dust. However, coal dust often contains silica, so miners can suffer from a mix of both conditions.