What Leads to Signs of Skin Infections: A Complete Guide
Discover what leads to skin infections with this complete guide. Learn about causes, risk factors, common signs, and prevention tips to protect your skin and know when to seek medical help.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Your skin is an incredible organ, serving as a dynamic shield between your body and the outside world. But sometimes, this barrier is compromised, allowing microscopic invaders to sneak in and cause trouble. Recognizing what leads to signs of skin infections is the first step toward effective prevention and treatment. These infections can range from a minor, annoying itch to a serious medical condition requiring immediate attention. This comprehensive guide will walk you through the common causes, from bacteria and fungi to everyday risk factors, and equip you with the knowledge to identify the warning signs. We’ll explore how breaches in your skin’s integrity, your overall health, and even your environment can create the perfect storm for an infection to take hold. By understanding the "why" behind the redness, swelling, and pain, you can become proactive in protecting your skin’s health.
Understanding Skin Infections: The Basics
What is a Skin Infection?
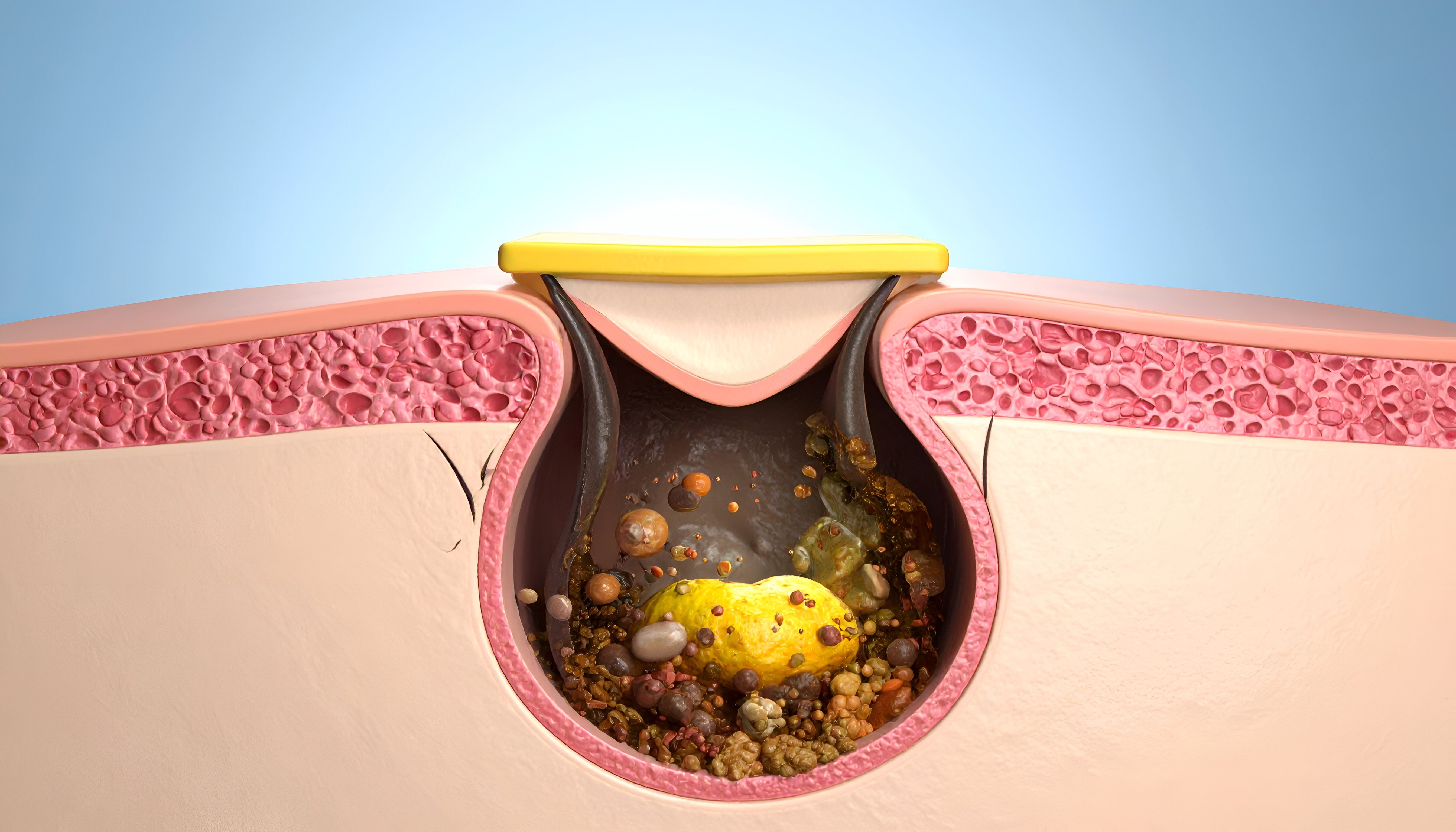
A skin infection occurs when pathogens, disease-causing microorganisms like bacteria, fungi, or viruses, penetrate the skin's protective outer layer and begin to multiply. This invasion triggers your body's immune response, leading to the classic signs of inflammation: redness, heat, swelling, and pain. The specific type and severity of the infection depend entirely on the kind of pathogen involved and the depth of the infection.
How Your Skin Normally Protects You
Your skin isn't just a passive wall; it's an active ecosystem. The acid mantle, a thin, slightly acidic film on the skin's surface, inhibits the growth of many harmful microbes. Additionally, a diverse community of harmless bacteria known as your skin microbiome acts as a living defense system, outcompeting potential pathogens for space and resources. When this delicate balance is disrupted, or the physical barrier is broken, the risk of infection rises significantly.
The Main Culprits: Types of Pathogens That Cause Infections
Bacterial Invaders (e.g., Staph, Strep)
Bacteria are among the most common causes of skin infections. Staphylococcus aureus (staph) is a frequent offender, often living harmlessly in the nose or on the skin but causing problems if it enters a wound. It can lead to infections like impetigo (honey-crusted sores), folliculitis (infected hair follicles), boils, and serious cellulitis. Streptococcus bacteria can also cause cellulitis and impetigo.
Fungal Foes (e.g., Ringworm, Yeast)
Fungi thrive in warm, moist environments. Dermatophytes cause infections like athlete's foot, jock itch, and ringworm (which is not a worm at all). These often present as itchy, red, scaly patches with a defined border. Yeasts like Candida can also cause infections, particularly in skin folds (armpits, under breasts, groin), leading to a red, raw rash with satellite pustules.
Viral Villains (e.g., Herpes, Warts)
Viruses cause infections by invading skin cells and using them to replicate. The herpes simplex virus (HSV) causes cold sores and genital herpes, characterized by painful, fluid-filled blisters. The varicella-zoster virus causes chickenpox and later, shingles—a painful, blistering rash. Human papillomavirus (HPV) leads to warts, which are rough, raised bumps on the skin.
Parasitic Pests (e.g., Scabies, Lice)
Though less common, tiny insects or parasites can burrow or bite into the skin, causing intense itching and a rash. Scabies is caused by microscopic mites that burrow under the skin, leading to a pimple-like rash and severe itch, often worse at night. Lice infestations on the head, body, or pubic area also cause significant itching from their bites and can lead to secondary bacterial infections from scratching.
Common Signs and Symptoms of a Skin Infection
Universal Red Flags: Redness, Swelling, and Pain
The body's inflammatory response is universal. Look for:
Redness (Erythema): The infected area often becomes red and inflamed.
Swelling (Edema): Fluid and immune cells rush to the area, causing puffiness.
Pain or Tenderness: The area may be painful to the touch or even without contact.
Warmth: The infected skin often feels warmer than the surrounding area.
When to Worry; Pus, Blisters, and Fever
More advanced signs indicate a progressing infection and require medical attention:
Pus or Discharge: A thick, white, yellow, or greenish fluid comprised of dead white blood cells, bacteria, and skin debris. This is a hallmark of a bacterial infection.
Blisters or Pustules: Small, fluid-filled bumps on the skin.
Skin Ulceration or Sores: Breaks in the skin that do not heal.
Itching and Rashes: Common with fungal and viral infections.
Systemic Symptoms: Fever, chills, swollen lymph nodes, or red streaks spreading from the wound are serious signs that the infection may be entering the bloodstream.
Top Causes and Risk Factors for Skin Infections
Breaks in the Skin: Cuts, Scrapes, and Surgical Wounds
The most straightforward cause is a break in the skin's barrier. This includes:
Minor injuries: Paper cuts, scrapes, insect bites, and burns.
Surgical incisions: Any surgery creates a potential entry point.
Chronic conditions: Eczema (atopic dermatitis) and psoriasis cause cracks and fissures in the skin.
Intravenous drug use: This carries a very high risk of introducing pathogens.
Weakened Immune System and Underlying Health Conditions
Your immune system is your army. If it's compromised, it can't fight off invaders effectively. Risk factors include:
Diabetes: High blood sugar can impair white blood cell function and reduce blood flow to the skin.
HIV/AIDS, Cancer, or Autoimmune Diseases: These conditions directly weaken the immune response.
Certain Medications: Immunosuppressants (e.g., after an organ transplant) or long-term corticosteroid use.
Poor Hygiene and Skin Care Habits
While not the only cause, hygiene plays a key role:
Not cleaning wounds properly: Dirt and bacteria left in a cut can fester.
Sharing personal items: Towels, razors, or athletic equipment can spread fungi and bacteria.
Wearing damp clothing: Trapped moisture creates a perfect environment for fungal growth.
Environmental Exposures and Lifestyle Factors
Climate: Hot, humid weather promotes fungal and bacterial growth.
Community Settings: Gyms, locker rooms, swimming pools, and daycare centers are common places where infections like plantar warts and athlete's foot spread.
Close Contact: Sports like wrestling (ringworm is often called "mat herpes") or simply living in close quarters can facilitate the spread of pathogens.
Prevention: How to Keep Your Skin Healthy and Protected
The best treatment is always prevention. You can drastically reduce your risk by:
1. Cleanse Wounds Immediately: Wash any cut, scrape, or bite with soap and clean water. Apply an over-the-counter antibiotic ointment and cover with a sterile bandage.
2. Practice Good Hygiene: Wash your hands frequently with soap and water. Shower after sweating heavily.
3. Moisturize: Keep your skin hydrated to prevent cracking and flaking, especially if you have eczema.
4. Don't Share Personal Items: This includes towels, razors, clothing, and sports equipment.
5. Wear Protective Gear: Wear shoes in public pools and locker rooms to avoid fungal infections.
6. Manage Chronic Conditions: Keep conditions like diabetes well-controlled under a doctor's guidance.
When to See a Doctor; Don't Ignore These Signs
While some minor infections may clear on their own, it's crucial to see a healthcare provider if:
The infection is spreading rapidly.
You see red streaks emanating from the wound.
You have a fever or chills.
The pain is severe.
There is a large amount of pus or drainage.
You have an underlying condition that weakens your immune system.
The infection doesn't start to improve after a few days of home care.
Early medical intervention, which may include prescription antibiotics, antifungals, or antivirals, can prevent a simple infection from becoming a life-threatening one.
Conclusion
Understanding what leads to signs of skin infections empowers you to be an active participant in your health. Your skin's job is to protect you, and by supporting it with proper care, you can strengthen its defenses. Remember that infections are caused by a confluence of factors: a breach in the barrier, the presence of a pathogen, and sometimes a weakened immune response. By practicing vigilant wound care, maintaining good hygiene, and listening to your body's warning signs, you can effectively manage your risk. If an infection does take hold, don't hesitate to seek professional help. Prompt treatment is the quickest path to recovery and restoring your skin's vital role as your body's powerful shield.
Frequently Asked Questions (FAQs) About Skin Infections
Q1. How can I tell if my cut is infected or just healing?
A healing cut will gradually improve, with reduced redness, swelling, and pain. An infected cut will get worse—becoming more red, swollen, painful, and may start producing pus after a day or two.
Q2. Are skin infections contagious?
Many are. Bacterial infections like impetigo and fungal infections like ringworm are highly contagious through direct skin contact or sharing contaminated items. Viral infections like herpes and warts are also contagious.
Q3. What's the best way to treat a minor skin infection at home?
For a very minor infection, keep the area clean and dry, apply an over-the-counter antibiotic ointment (for bacterial concerns) or antifungal cream (for fungal concerns), and cover it with a bandage. Monitor it closely for signs of worsening.
Q4. Can a skin infection go away on its own?
Some very mild infections might resolve as your immune system fights them off. However, it is often a gamble. Many infections, especially bacterial ones, can worsen quickly without proper treatment, so it's usually best to consult a doctor.
Q5. Why are people with diabetes more prone to skin infections?
High blood sugar can impair the function of white blood cells, weaken the skin's barrier function, and cause poor circulation, which reduces the delivery of immune cells and nutrients to a wound, slowing healing and increasing infection risk.
Consult a Specialist for Personalised Advice
Consult a Specialist for Personalised Advice

Dr Suseela
General Physician
5 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ashita Kuruvilla
General Practitioner
7 Years • MBBS
Kolkata
KVC CLINIC, Kolkata

Dr. K Vijaya Kumar
General Practitioner
5 Years • MBBS, Fellowship in Diabetes Mellitus
Mottur
PADMAVATHI CLINIC, Mottur

Dr. Sujay Jagatap
General Practitioner
5 Years • MBBS
Bangalore Rural
Ashwini Clinic., Bangalore Rural