Say No to Tobacco: A Pulmonologist’s Guide
Know about the tobacco effect, what are the consequences, risks, steps to quit tobacco, second and third hand smoke, challenges of quitting and more.

.webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Introduction
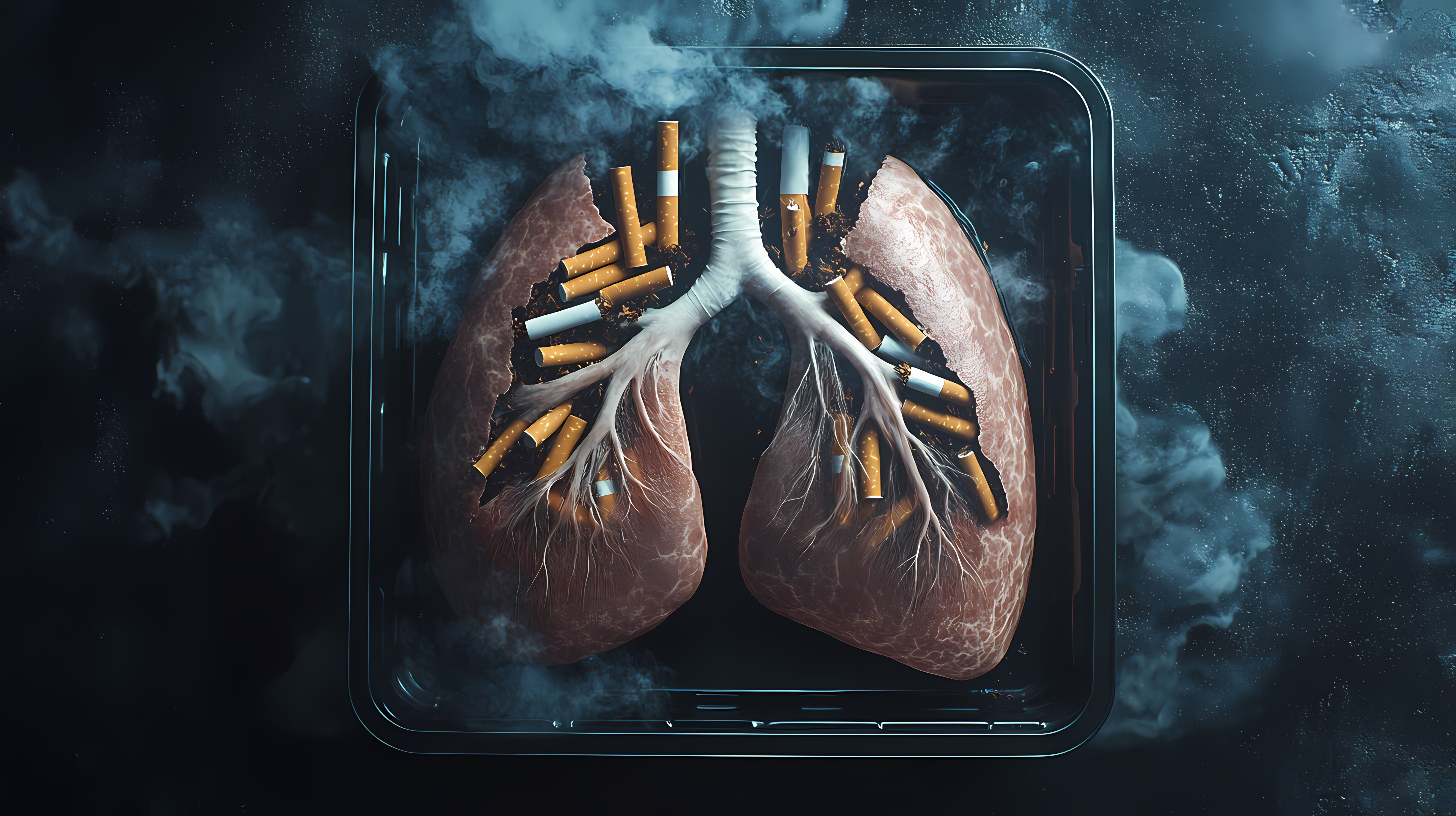
If you could watch the lungs of a regular smoker and a non-smoker side-by-side, you’d never think of tobacco the same way. As pulmonologists, we see tobacco damage daily: stubborn coughs, breathlessness that limits life, infections that linger, and cancers caught too late. The good news? It’s never too late to stop. Your lungs can heal more than you think, and powerful tools can help you quit for good.
This guide combines the best evidence with practical steps. You’ll learn exactly how tobacco harms the lungs, why secondhand and thirdhand smoke endanger your family, and what to expect when you quit—from the first 20 minutes to 10 years later. We’ll compare cigarettes, smokeless tobacco, and e-cigarettes, outline proven quitting strategies, and discuss when to see a pulmonologist. We’ll also cover community policies that reduce tobacco use and point you to trusted resources in India and worldwide. Let’s breathe easier together and say no to tobacco.
Consult Top Pulmonologist Doctors for Personalised Advice
What Pulmonologists See: The Lung Toll of Tobacco
The effects of tobacco on the lungs include:
Smoking and COPD: Why breathlessness creeps up
Chronic obstructive pulmonary disease (COPD) is the lung condition most closely tied to smoking—most cases are caused by long-term tobacco use. Cigarette smoke injures the airways and alveoli, leading to chronic bronchitis (inflamed, mucus-clogged airways) and emphysema (destroyed air sacs). Over time, you notice breathlessness on stairs, then on flat ground, then during daily chores—an insidious progression many mistake for “getting older.” Evidence shows smoking is the leading risk factor for COPD, and stopping smoking is the single most effective step to slow its progression. For the general public seeking pulmonologist advice for smokers, the message is simple: the earlier you quit, the more lung function you preserve.
Tobacco and lung cancer: Understanding risk and symptoms
Tobacco smoke contains dozens of carcinogens that damage DNA, fueling lung cancer. Risk rises with “pack-years” (packs per day × years smoked), but there’s no safe threshold. Early symptoms are subtle: a persistent cough, chest pain, coughing up blood, or recurrent pneumonia. Smoking also raises risks for other thoracic cancers and worsens outcomes for nearly every organ system [3].
Case perspective: Even for long-time smokers, quitting lowers risk over time. A decade after quitting, lung cancer risk drops to about half that of a continuing smoker [2][3]. For those asking about lung cancer screening criteria in India or elsewhere, read the screening section to see who qualifies for low-dose CT scans.
Asthma, infections, and poor healing: The hidden daily costs
Tobacco inflames the airways, making asthma harder to control and increasing the need for reliever inhalers. Smoke impairs the lungs’ cilia—tiny hair-like cleaners—so viruses and bacteria linger, leading to more colds, bronchitis, and pneumonia. Wounds heal more slowly, and surgeries carry higher complication risks [2]. If frequent chest infections or wheezing persist, book a physical visit to a doctor with Apollo 24|7 to optimise treatment and plan a cessation strategy.
What’s in Tobacco Smoke and Why It Harms
The tobacco smoke contains:
- 7,000 chemicals, 70 carcinogens: Tar, CO, oxidants
- Cigarette smoke is a toxic cloud of more than 7,000 chemicals; at least 70 are known carcinogens.
Key offenders:
1.Tar: A sticky residue that stains lungs, clogs airways, and carries carcinogens deep into tissues.
2.Carbon monoxide (CO): Displaces oxygen from red blood cells, straining your heart and starving tissues.
3.Free radicals and oxidants: Trigger chronic inflammation and oxidative stress, accelerating tissue damage and atherosclerosis.
This chemical mix explains the broad effects of tobacco on lungs and the cardiovascular system why smokers face heart attacks, strokes, and peripheral artery disease in addition to lung disease.
Nicotine and addiction: How your brain gets hooked
Nicotine is the “hook,” reshaping brain circuits for reward and stress. It spikes dopamine quickly, reinforcing the habit. Over time, your brain expects nicotine; without it, withdrawal symptoms irritability, cravings, poor concentration appear. The paradox: nicotine drives addiction, but it’s the smoke’s toxins that cause cancer and organ damage. That’s why nicotine replacement therapy India options (patches, gum, lozenges) are effective: they curb withdrawal without exposing you to smoke toxins.
Smokeless Tobacco and Vaping: Not Safe Alternatives
The alternatives include:
Chewing tobacco, gutkha, and oral cancers
Smokeless tobacco—chew, snuff, khaini, gutkha—often feels safer because there’s no smoke. It isn’t. These products contain nitrosamines and other carcinogens that increase risks of oral, oesophagal, and pancreatic cancers; they also cause gum disease, tooth decay, and nicotine addiction. In South Asia, smokeless risk of oral cancer risk is high due to early age of initiation and frequent use. Quitting aids and counselling are just as important for smokeless users as for smokers.
E-cigarettes and the lungs: What we know (and don’t)
E-cigarettes heat a liquid into an aerosol containing nicotine, ultrafine particles, heavy metals, and volatile compounds. They generally expose users to fewer toxic chemicals than cigarettes, but they are not harmless—especially for youth, pregnant people, and those with lung disease. In 2019, a severe outbreak of e-cigarette or vaping product use–use-associated lung injury (EVALI) was linked primarily to vitamin E acetate in illicit THC products. Most cases subsided after warnings and removals, but the event underscores safety uncertainties.
Secondhand and Thirdhand Smoke: Protecting Your Family
Risks for children and pregnancy
Secondhand smoke causes heart disease, lung cancer, stroke, and, in children, sudden infant death syndrome (SIDS), ear infections, asthma attacks, and respiratory infections. There is no safe level of exposure. Thirdhand smoke—the residue that clings to clothes, furniture, and car seats contains toxins that can be ingested or inhaled, posing risks to infants and children.
Making homes and cars smoke-free
- Make a house rule: No tobacco indoors or in the car, ever.
- Inform guests and family early; provide a designated outdoor area if needed.
- Use reminders: door signs, phone lock screens.
- Wash fabrics and deep-clean regularly to minimise residues.
- If you live in multi-unit housing, advocate for smoke-free policies.
The Benefits of Quitting: How Your Lungs Recover
A timeline of healing—from minutes to years
Your body begins healing within minutes of your last cigarette:
- 20 minutes: Heart rate and blood pressure drop.
- 12 hours: Carbon monoxide levels normalise.
- 2–12 weeks: Circulation improves; lung function starts to increase.
- 1–9 months: Coughing and shortness of breath decrease as cilia recover.
- 1 year: The Excess risk of coronary heart disease halves.
- 10 years: Lung cancer death rate drops to about half that of a continuing smoker.
This tobacco withdrawal symptoms timeline is encouraging—many people notice better taste and smell within days, more energy within weeks, and fewer colds within months.
Long-term risk reduction and quality of life
Quitting at any age adds years to life and life to years. COPD progression slows, asthma control improves, and surgeries and infections carry fewer complications. Even if you’ve smoked for decades, stopping now reduces risks of stroke, peripheral artery disease, and several cancers (mouth, throat, bladder, pancreas). Many people also save substantial money—funds you can redirect to fitness, family, or a celebratory trip.
How to Quit Tobacco: A Step-by-Step Plan
The steps include:
Set a quit date, know your triggers, prepare your environment
1.Pick a quit date within the next 2–4 weeks and write it down.
2.List triggers: stress, tea/coffee, after meals, driving, social events.
2.Change the context: switch beverages, adjust routines, go for a brief walk after meals.
3.Remove tobacco, lighters, ashtrays. Clean your space to erase odors.
4.Tell your support circle; ask for specific help (daily check-ins, joining you for walks).
This is the foundation for how to quit smoking naturally—by reshaping your environment and habits.
Medications that work: NRT, varenicline, bupropion
Medication plus counseling roughly doubles to triples your chance of success. Options include:
1.Nicotine replacement therapy (patch + short-acting gum/lozenge): Combining a steady patch with on-demand gum for cravings works better than single products.
2.Varenicline: A partial nicotine receptor agonist that reduces withdrawal and blocks reward; among the most effective single agents.
3.Bupropion SR: Helps with cravings and weight control.
High-quality reviews show varenicline and combination NRT have the strongest evidence; bupropion is also effective. Discuss risks/benefits with your doctor, especially if you’re pregnant, have mental health conditions, or take other medications. For nicotine replacement therapy India access and prescriptions, consult a doctor online with Apollo 24|7 to tailor dosing.
Screening, Red Flags, and When to See a Doctor
Lung cancer screening eligibility
Annual low-dose CT (LDCT) screening is recommended for adults aged 50–80 years with a 20 pack-year smoking history who currently smoke or quit within the past 15 years, provided they’re healthy enough for curative treatment [8]. Screening detects cancers earlier, when they’re more treatable. If you’re close to these criteria, ask your doctor whether LDCT is right for you. Guidelines may vary by country; in India, many tertiary centres offer LDCT—your pulmonologist can advise.
Chronic cough and breathlessness: When to worry
Red flags:
1.Cough lasting more than 3 weeks, coughing up blood
2.Worsening breathlessness, chest pain
3.Unexplained weight loss, recurrent chest infections
4.New wheeze in an adult, voice changes
If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. You may need spirometry (to diagnose COPD or asthma), chest imaging, or specialist referral. For related labs like HbA1c or lipid profile, if you have co-existing conditions, Apollo 24|7 offers convenient home collection—useful when planning comprehensive risk reduction.
Conclusion
Tobacco steals breath quietly, one day at a time—but you can take it back. Understanding what tobacco does to your lungs, how quickly the body heals after quitting, and which tools make quitting more successful puts you in control. From proven medications and counseling to smoke-free home rules and supportive policies, help is within reach. If you’re unsure where to begin, start small: pick a quit date, tell someone you trust, and remove tobacco from your environment. Then layer in support—nicotine replacement, varenicline or bupropion if appropriate, and a quitline or app to keep you on track.
If nagging symptoms concern you—chronic cough, breathlessness, chest pain—or you might qualify for lung cancer screening, consult a doctor online with Apollo 24|7 for guidance. Your lungs are resilient; every tobacco-free day is a win for your health and your family’s wellbeing. Say no to tobacco today, and give your future self the gift of easy, comfortable breathing.
Consult Top Pulmonologist Doctors for Personalised Advice
Consult Top Pulmonologist Doctors for Personalised Advice

Dr. P Sravani
Pulmonology Respiratory Medicine Specialist
3 Years • MBBS, MD
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam

Dr. Kohena Roy
Pulmonology Respiratory Medicine Specialist
8 Years • MBBS, MD Respiratory Medicine
Rajpur Sonarpur
SRL Diagnostics Pvt. Ltd, Rajpur Sonarpur

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. K Prasanna Kumar Reddy
Pulmonology Respiratory Medicine Specialist
16 Years • MBBS, DTCD (TB&CHEST), DNB (PULM MED), FCCP
Hyderabad
Apollo Medical Centre Kondapur, Hyderabad
Consult Top Pulmonologist Doctors for Personalised Advice

Dr. P Sravani
Pulmonology Respiratory Medicine Specialist
3 Years • MBBS, MD
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam

Dr. Kohena Roy
Pulmonology Respiratory Medicine Specialist
8 Years • MBBS, MD Respiratory Medicine
Rajpur Sonarpur
SRL Diagnostics Pvt. Ltd, Rajpur Sonarpur

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. K Prasanna Kumar Reddy
Pulmonology Respiratory Medicine Specialist
16 Years • MBBS, DTCD (TB&CHEST), DNB (PULM MED), FCCP
Hyderabad
Apollo Medical Centre Kondapur, Hyderabad
More articles from Smoking Cessation
Frequently Asked Questions
Is vaping safer than smoking tobacco?
Vaping generally exposes you to fewer toxins than cigarettes but is not harmless, especially for youth and those with lung conditions. The goal should be complete cessation; discuss options with a pulmonologist. (e-cigarettes vs tobacco safety)
How long until my lungs improve after I quit?
Some benefits start within minutes. Within weeks, lung function begins to improve; within months, cough and breathlessness ease; and after a year, heart disease risk drops by about half [2]. (tobacco withdrawal symptoms timeline)
Do nicotine patches and gum really help?
Yes. Nicotine replacement therapy (especially a patch plus short-acting gum/lozenge), varenicline, and bupropion significantly increase quit success, especially when combined with counseling [7]. (nicotine replacement therapy India)
Is smokeless tobacco safer than cigarettes?
No. Smokeless products raise risks of oral, esophageal, and pancreatic cancers and cause gum disease and addiction [6]. (smokeless tobacco oral cancer risk)
Who should get lung cancer screening?
Adults 50–80 with a 20 pack-year history who currently smoke or quit within 15 years should ask about annual low-dose CT [8]. Criteria may vary; consult your doctor. (lung cancer screening criteria India)