Guide to Stroke Patient Should Be Rushed Immediately Hospital
Learn why immediate action is crucial during a stroke. Recognise the FAST signs, understand the golden hour, and know what to do before reaching the hospital to save lives.


Introduction: Every Minute Counts in a Stroke
A stroke is a medical catastrophe that strikes suddenly, often without warning. It occurs when the blood supply to a part of the brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. In this critical scenario, time is not just money; it is brain cells. For every minute a stroke goes untreated, a person can lose around 1.9 million neurons. This is why the single most important action you can take is to ensure a stroke patient is rushed to the hospital immediately. This guide is designed to be your clear, actionable roadmap for that exact moment. We will demystify what a stroke is, teach you how to spot the signs using the simple FAST acronym, explain exactly why speed is so critical, and walk you through what to do from the first second you suspect a stroke to the moment professional help takes over. Understanding this information can make the difference between a full recovery and permanent disability, or worse. Let’s empower you to act decisively and save a life.
What is a Stroke? A Brief Explanation of a Brain Attack
Often called a "brain attack," a stroke is analogous to a heart attack but occurs in the brain. It's a disruption of the vital blood flow that keeps our brain functioning. There are two primary types of strokes, and understanding the difference highlights why immediate hospital care is non-negotiable.
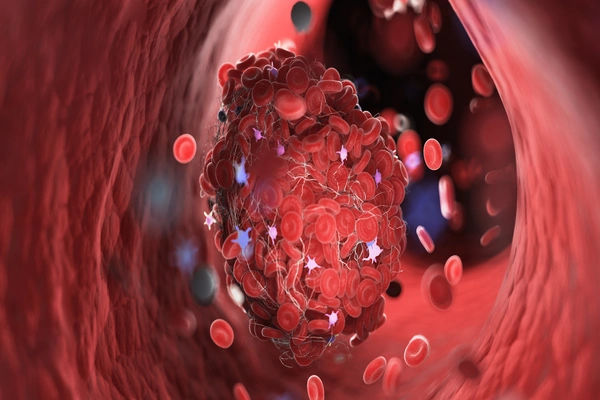
1. Ischaemic Stroke: The Clogged Artery
Accounting for about 87% of all strokes, an ischaemic stroke happens when a blood clot blocks or plugs an artery leading to the brain. The clot may form in the artery itself (thrombotic stroke) or travel from elsewhere in the body, such as the heart, and lodge in a narrower brain artery (embolic stroke). The goal of emergency treatment is to dissolve or remove this clot as quickly as possible to restore blood flow.
2. Haemorrhagic Stroke: The Burst Blood Vessel
A haemorrhagic stroke is less common but often more deadly. It occurs when a weakened blood vessel in the brain ruptures and bleeds into the surrounding tissue. The accumulated blood compresses brain structures, causing damage. Emergency treatment focuses on controlling the bleeding and reducing pressure on the brain.
Recognising a Stroke: The FAST Acronym and Beyond
Recognising the signs of a stroke is the first step to getting life-saving help. The FAST acronym is a globally recognised tool designed for quick public recall.
F - Face Drooping
Ask the person to smile. Does one side of the face droop or is it numb? An uneven smile is a classic red flag.
A - Arm Weakness
Ask the person to raise both arms. Does one arm drift downward? Weakness or numbness in one arm is a key sign.
S - Speech Difficulty
Ask the person to repeat a simple sentence, like "The sky is blue." Is their speech slurred, strange, or difficult to understand?
T - Time to Call Emergency Services
If you observe any of these signs, even if they seem to come and go, it is TIME to call your local emergency number (like 108 or 102) immediately. Note the time when the symptoms first appeared, as this is critical information for doctors.
Other Crucial Stroke Symptoms You Shouldn't Ignore
While FAST covers the major signs, a stroke can present in other ways. Be aware of:
- Sudden numbness or weakness in the leg.
- Sudden confusion, trouble understanding others.
- Sudden trouble seeing in one or both eyes.
- Sudden trouble walking, dizziness, loss of balance, or lack of coordination.
- A sudden, severe headache with no known cause, often described as "the worst headache of my life."
Why the Rush? The Critical Importance of the "Golden Hour"
The phrase "Time is Brain" is a fundamental principle in stroke care. The sooner a stroke patient receives treatment, the better their chances of survival and recovery. The first 60 minutes after symptom onset are often called the "golden hour"—a window of opportunity where interventions are most effective.
How Immediate Treatment Saves Brain Cells
Brain cells are incredibly sensitive to oxygen deprivation. When blood flow is cut off, they begin to die within minutes. The area where cells are irretrievably lost is called the infarct core. Surrounding this core is the "ischaemic penumbra," a region of brain tissue that is at risk but can still be saved with prompt treatment. The goal of rushing to the hospital is to rescue the penumbra.
The TPA Window: Restoring Blood Flow
For ischaemic strokes, a clot-busting drug called alteplase (tPA) can dissolve the clot and restore blood flow. However, this drug must be administered within a strict time window—typically within 4.5 hours of symptom onset, and the sooner, the better. In some cases, a procedure called a thrombectomy (physically removing the clot) can be performed up to 24 hours for select patients, but early action still leads to vastly better outcomes. Delaying treatment by even 15 minutes can significantly impact a patient's quality of life.
What to Do While Waiting for the Ambulance: A Step-by-Step Guide
Your actions in the minutes before professional help arrives are crucial. Stay calm and follow these steps.
Do’s: Crucial Actions to Take
When faced with a medical emergency, these immediate actions can make a critical difference:
- Call Emergency Services Immediately: Do not call a family doctor or drive the patient yourself. Paramedics can begin life-saving treatment en route to the hospital and alert the emergency room, saving precious time.
- Note the Time: Record when the symptoms first started. This is the single most important piece of information for the medical team.
- Keep the Person Calm and Comfortable: Have them lie down on their side with their head slightly elevated (if they are conscious) to aid breathing and prevent choking if they vomit.
- Loosen Tight Clothing: Such as a collar or belt.
- Be Ready to Inform: Tell the paramedics what happened, what symptoms you saw, and the time they started.
Don’ts: Common Mistakes to Avoid
In a stroke emergency, avoid these common mistakes at all costs:
- DO NOT give the person any food, drink, or medication. Aspirin, for instance, could be dangerous if the stroke is haemorrhagic.
- DO NOT let the person drive themselves to the hospital.
- DO NOT wait to see if the symptoms go away. Even if symptoms seem to fade, it could be a transient ischaemic attack (TIA or "mini-stroke"), which is a major warning sign of a full-blown stroke that requires immediate medical attention.
What Happens at the Hospital? The Stroke Response Protocol
Upon arrival at a certified stroke center, the medical team swings into a well-rehearsed, rapid-response protocol.
Rapid Diagnosis: Scans and Tests
The first priority is to determine the type of stroke. This is typically done with a CT scan or an MRI of the brain. These images can quickly show whether the stroke is ischaemic (caused by a clot) or haemorrhagic (caused by bleeding). This distinction dictates the entire treatment path.
Emergency Treatment Options
In the case of a stroke, the treatment approach depends on whether it is ischemic or hemorrhagic:
- For Ischaemic Stroke: If the patient is within the time window, they may receive tPA. They might also be a candidate for a thrombectomy.
- For Haemorrhagic Stroke: Treatment focuses on controlling the bleed. This may involve medication to reduce blood pressure or surgery to repair the broken blood vessel.
The complexity of diagnosis and treatment underscores why consulting specialists is vital. If you or a loved one experiences stroke symptoms, getting to a hospital with a dedicated neurology department is critical. For follow-up care and consultation, you can connect with experienced neurologists online through Apollo24|7.
The Road to Recovery: Life After a Stroke
Recovery is a marathon, not a sprint. It begins in the hospital and continues with long-term rehabilitation, which may include physical therapy to regain movement, occupational therapy to relearn daily skills, and speech therapy. The extent of recovery varies, but early and aggressive rehabilitation is key to maximising outcomes.
Conclusion: Acting FAST Can Save a Life
A stroke is a race against time, and every second truly matters. Recognising the warning signs, calling emergency services without delay, and getting the patient to a hospital can mean the difference between recovery and lifelong disability—or even life and death. The FAST approach is simple yet powerful: it equips anyone to act swiftly and confidently in a critical moment. Remember, strokes don’t wait, and neither should you. By staying alert and prepared, you can protect your loved ones, preserve precious brain function, and, most importantly, save a life.
Consult a Neurologist for the best advice
Consult a Neurologist for the best advice

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. Vemula Sreekanth
Neurologist
18 Years • MD(Med), DM(Neuro)
Hyderabad
Apollo Hospitals Financial District, Hyderabad

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi
More articles from Stroke
Frequently Asked Questions
1. What is the difference between a stroke and a mini-stroke (TIA)?
A TIA (transient ischaemic attack) produces stroke-like symptoms that typically last only a few minutes and leave no permanent damage. However, a TIA is a major warning sign that a full-scale stroke may be imminent. It requires the same immediate medical response as a stroke.
2. Can young people have strokes?
Yes. While risk increases with age, strokes can occur at any age, including in children. Factors like congenital heart defects, clotting disorders, and lifestyle choices can contribute to strokes in younger adults.
3. What are the long-term effects of a stroke?
Long-term effects depend on the stroke's severity and location in the brain. They can include paralysis, speech and language problems, memory loss, emotional changes, and chronic pain.
4. What should I do if I live alone and think I'm having a stroke?
Call emergency services immediately. Unlock your door so paramedics can enter. Then, lie down in a position where you are visible from the doorway. Do not attempt to drive.
5. How can I reduce my risk of having a stroke?
Manage high blood pressure, quit smoking, control diabetes, maintain a healthy weight, eat a balanced diet low in sodium, exercise regularly, and limit alcohol consumption.