Sex and Stroke A Comprehensive Guide to Risks and Recovery
Discover the connection between sex and stroke, including rare risks, recovery challenges, and how to rebuild intimacy after a stroke.


Introduction
The connection between sex and brain stroke is a topic often shrouded in worry and silence, yet it's a crucial aspect of both preventive health and post-stroke recovery. When we hear about a stroke occurring during sexual activity, it can understandably cause anxiety. However, the reality is more nuanced. For the vast majority of people, sex is a safe and healthy activity. The key is understanding the specific circumstances where risk may be elevated and, equally important, how a stroke can profoundly affect one's sexual health and intimate relationships. This guide aims to demystify this complex link. We will explore the rare instances where sexual activity can precipitate a stroke, identify who might be most vulnerable, and then shift focus to the more common challenge: navigating intimacy after a stroke has occurred. Our goal is to provide you with evidence-based information and compassionate advice to foster open communication and a fulfilling life. If you have specific concerns about your stroke risk or recovery, consulting a doctor online with Apollo24|7 can provide personalised guidance.
The Surprising Link: Can Sex Actually Cause a Stroke?
The short answer is that it's extremely rare, but possible. For a healthy individual with no underlying risk factors, the chance of suffering a stroke during or immediately after sex is minuscule. It's essential to distinguish between a cause and a trigger. Sexual activity does not cause a stroke in the way long-term high blood pressure or atherosclerosis does. Instead, it can act as a precipitating factor in someone who already has significant, undiagnosed vulnerabilities.
Understanding the "Precipitation" vs. "Cause"
Think of it like a fragile glass vase with a hidden crack. A slight bump might be enough to make it shatter, but the bump wasn't the root cause—the crack was. Similarly, a person may have a weakened blood vessel (like an aneurysm) or severe plaque build-up in their arteries. The physical exertion of sex can be the "bump" that leads to a rupture or clot dislodgement, resulting in a stroke.
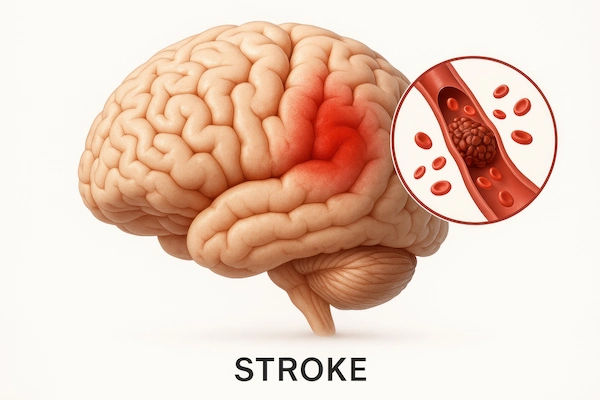
The Role of Sudden Blood Pressure Spikes
During sex, especially at orgasm, your heart rate and blood pressure rise significantly. This is a normal physiological response. For most, this temporary spike is harmless. However, for individuals with uncontrolled hypertension, this surge can put excessive strain on blood vessels in the brain. In the case of a haemorrhagic stroke (caused by a burst blood vessel), this pressure can be the final straw. For an ischaemic stroke (caused by a clot), the increased pressure could potentially dislodge a clot. Research suggests that this type of stroke trigger accounts for less than 1% of all cases, emphasising its rarity.
Who is Most at Risk During Sexual Activity?
Understanding your personal risk factors is the first step towards prevention. The individuals who need to be most mindful are those with pre-existing conditions that affect cardiovascular and cerebrovascular health.
Pre-existing Cardiovascular Conditions
The primary risk group includes people with:
• Uncontrolled High Blood Pressure: This is the single most important modifiable risk factor for stroke.
• Atherosclerosis: Hardened and narrowed arteries are more prone to blockages.
• Heart Conditions: Such as atrial fibrillation (AFib), which can cause blood clots to form in the heart that may travel to the brain.
• Known Brain Aneurysms or Vascular Malformations: These are structural weaknesses in the brain's blood vessels.
The Impact of Lifestyle Factors
Lifestyle choices compound these risks. Smoking, a sedentary lifestyle, obesity, and a poor diet all contribute to the underlying vascular disease that sets the stage for a stroke. Engaging in sexual activity after heavy alcohol consumption or using stimulant drugs dramatically increases the risk, as these substances can cause dangerous spikes in blood pressure and heart rate.Consult a Neurologist for the best advice
Recognising the Signs of a Stroke: Act F.A.S.T.
It's vital for everyone to know the signs of a stroke. If you or your partner experience any of the following during or after sex, seek emergency medical attention immediately.
• Face: Does one side of the face droop?
• Arms: Can the person raise both arms evenly?
• Speech: Is speech slurred or strange?
• Time: Time is critical. Call for an ambulance right away.
The Other Side of the Coin: How a Stroke Affects Your Sex Life
While the risk of sex causing a stroke is low, the impact of a stroke on sexual function is very common and can be one of the most challenging aspects of recovery. This affects both the survivor and their partner.
Physical Changes After a Brain Stroke
A stroke can damage the areas of the brain responsible for sexual response. This can lead to:
• Low Libido: A significantly decreased interest in sex is frequently reported.
• Erectile Dysfunction (ED) in Men: Difficulty achieving or maintaining an erection.
• Vaginal Dryness in Women: Making intercourse painful or uncomfortable.
• Fatigue: Extreme tiredness is common after a stroke, leaving little energy for intimacy.
• Physical Limitations: Paralysis or weakness on one side of the body can make certain positions difficult or affect sensation.
Emotional and Psychological Hurdles
The psychological impact is often more profound than the physical:
• Depression and Anxiety: These are common after a stroke and are major contributors to low libido.
• Changes in Body Image: A person may feel less attractive or confident due to physical changes.
• Fear and Anxiety: The survivor or their partner may fear that sex could trigger another stroke, creating a significant mental barrier.
The Impact on Relationships and Intimacy
Communication is key. Partners may be afraid to initiate sex for fear of hurting the survivor. The survivor might withdraw, feeling inadequate. This can lead to a cycle of misunderstanding and distance, where intimacy suffers not just physically, but emotionally as well. Rebuilding this connection is a critical part of the healing process.
Reclaiming Intimacy: A Guide to a Safe and Fulfilling Sex Life After a Stroke
Returning to a healthy sex life after a stroke is a journey that requires patience, communication, and often, medical guidance.
The First Step: Talking to Your Doctor and Partner
Before resuming sexual activity, it's crucial to have an open conversation with your healthcare provider. They can assess your cardiovascular health and give you the green light, ensuring it is safe sex after a brain stroke. They can also address issues like erectile dysfunction or vaginal dryness, possibly prescribing medications or treatments. Equally important is talking to your partner. Share your fears, desires, and limitations. This conversation is the foundation for rebuilding intimacy.
Practical Tips for Easing Back into Intimacy
• Choose a Time When You're Rested: Don't try to have sex when you're fatigued.
• Create a Relaxing Environment: Reduce stress and distractions.
• Start Slowly: Intimacy doesn't have to lead to intercourse. Focus on cuddling, kissing, and massage.
• Experiment with Positions: Find comfortable positions that accommodate any physical limitations.
• Use Lubricants: If vaginal dryness is an issue, a good water-based lubricant can make a big difference.
Focusing on Connection Beyond Intercourse
The goal is to reconnect, not just to perform. Emotional intimacy is the bedrock of a healthy sexual relationship after a stroke. Expressing affection, spending quality time together, and showing appreciation can rebuild the bond that the stroke may have strained. If communication is difficult, consider seeking help from a counsellor or therapist who specialises in post-stroke relationship dynamics.
Conclusion
The relationship between sex and brain stroke is multifaceted, encompassing both rare risks and common challenges in recovery. Understanding that sexual activity is a safe part of life for most people can alleviate unnecessary fear. However, being aware of your personal health status is crucial for prevention. For stroke survivors and their partners, the path back to intimacy requires compassion, communication, and often, professional support. The focus should shift from performance to connection, rediscovering intimacy in new and meaningful ways. Remember, you are not alone in this journey. If you have ongoing concerns about your cardiovascular health or are struggling with low libido after a brain injury, taking the step to consult a specialist is a sign of strength. Have you found this guide helpful? What other questions do you have about life after a stroke? We are here to support you with reliable information.
Consult a Neurologist for the best advice
Consult a Neurologist for the best advice

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. Vemula Sreekanth
Neurologist
18 Years • MD(Med), DM(Neuro)
Hyderabad
Apollo Hospitals Financial District, Hyderabad

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi
Consult a Neurologist for the best advice

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(125+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. Vemula Sreekanth
Neurologist
18 Years • MD(Med), DM(Neuro)
Hyderabad
Apollo Hospitals Financial District, Hyderabad

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi
More articles from Stroke
Frequently Asked Questions
1. How long after a stroke is it safe to have sex?
There's no one-size-fits-all answer. Most doctors recommend waiting until your condition has stabilised, which is typically 4-6 weeks after the stroke. However, you must get clearance from your doctor, who will evaluate your heart health and overall recovery progress.
2. Can an orgasm cause a stroke in a healthy person?
It is exceedingly rare. In a person with no underlying risk factors (like undiagnosed aneurysms or severe hypertension), the temporary rise in blood pressure during orgasm is very unlikely to cause a stroke.
3. What are the signs of a stroke during sex?
The signs are the same as any other stroke: sudden numbness or weakness in the face, arm, or leg (especially on one side), confusion, trouble speaking or understanding speech, vision problems, dizziness, loss of balance, or a severe headache. If you experience these, call for emergency help immediately.
4. My partner had a stroke and now has no interest in sex. Is this normal?
Yes, this is very common. Low libido can result from the brain injury itself, fatigue, depression, or medication side-effects. It's important to be patient and understanding. Encourage open communication and consider discussing this with a doctor, as treating underlying depression can often help.
5. Are there medications to help with sexual problems after a stroke?
Yes, for issues like erectile dysfunction, medications like PDE5 inhibitors (e.g., Sildenafil) may be an option, but only if your doctor confirms they are safe for you, as they can interact with other heart medications. For low libido related to depression, antidepressants may help. A doctor can guide you to the safest choice.