Understanding Different Types of Thalassemia
Understand the different types of thalassemia, including alpha and beta variants. Learn about their genetic causes, symptoms, severity levels, and how they affect red blood cell production and overall health.

Written by Dr. Siri Nallapu
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Thalassemia is a blood disorder that affects the body’s ability to produce hemoglobin, the protein in red blood cells that carries oxygen. If you or a loved one has been diagnosed with thalassemia, you may have questions about what it means and how to manage it. This article will help you understand the different types of thalassemia, their symptoms, causes, and ways to manage the condition effectively.
What is Thalassemia?
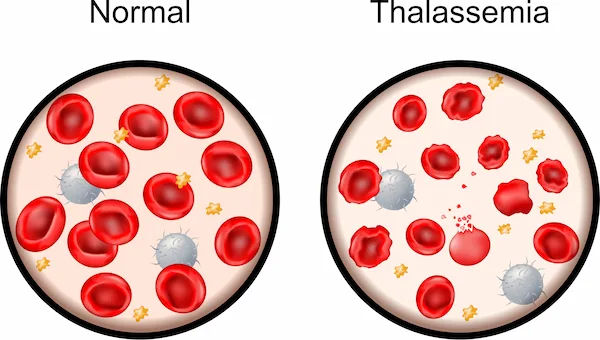
Thalassemia is an inherited blood disorder, which means it is passed down from parents to children through genes. It causes the body to produce fewer healthy red blood cells and less hemoglobin than normal. Without enough hemoglobin, red blood cells cannot function properly, leading to anemia, a condition where the body doesn’t get enough oxygen.
There are two main types of thalassemia:
1. Alpha Thalassemia – Occurs when there is a problem with the alpha globin protein chains in hemoglobin.
2. Beta Thalassemia – Occurs when there is a problem with the beta globin protein chains in hemoglobin.
Each type has different subtypes, ranging from mild to severe.
Types of Thalassemia
Below are the details about different types of Thalassemia,
1. Alpha Thalassemia
Alpha thalassemia occurs when one or more of the four genes needed to make alpha globin are missing or mutated. The severity depends on how many genes are affected:
Silent Carrier (1 gene missing) – No symptoms; the person is a carrier but does not have the disease.
Alpha Thalassemia Trait (2 genes missing) – Mild anemia, often mistaken for iron deficiency.
Hemoglobin H Disease (3 genes missing) – Moderate to severe anemia, requiring occasional blood transfusions.
Alpha Thalassemia Major (Hydrops Fetalis) (4 genes missing) – A severe, often fatal condition before or shortly after birth.
2. Beta Thalassemia
Beta thalassemia occurs when there are mutations in the genes that produce beta globin. The severity depends on how many genes are affected:
Beta Thalassemia Minor (Trait) (1 gene affected) – Mild anemia, usually no symptoms.
Beta Thalassemia Intermedia (2 genes partially affected) – Moderate anemia, may require occasional blood transfusions.
Beta Thalassemia Major (Cooley’s Anemia) (2 genes severely affected) – Severe anemia requiring lifelong blood transfusions and medical care.
Symptoms of Thalassemia
Symptoms vary depending on the type and severity of thalassemia. Common signs include:
Fatigue and weakness
Pale or yellowish skin (jaundice)
Slow growth in children
Bone deformities (especially in severe cases)
Enlarged spleen or liver
Dark urine
People with mild thalassemia may have no symptoms, while those with severe forms may experience significant health challenges.
Consult top Hematologist
Causes and Risk Factors
Thalassemia is inherited, meaning it is passed from parents to children through genes. If both parents carry the thalassemia gene, their child has a higher chance of inheriting a severe form.
Risk factors include:
Family history of thalassemia
Certain ethnic backgrounds (common in people of Mediterranean, South Asian, African, and Southeast Asian descent)
How Thalassemia Affects Health
Thalassemia can lead to complications such as:
Anemia – Low red blood cell count causing fatigue and weakness.
Iron Overload – Frequent blood transfusions can cause excess iron buildup, damaging organs.
Bone Problems – Thalassemia can weaken bones and increase fracture risk.
Heart and Liver Issues – Severe cases may lead to heart disease or liver problems.
Managing Thalassemia
While thalassemia is a lifelong condition, proper management can improve quality of life. Here are some ways to manage it:
Medical Treatments
Blood Transfusions – Needed for severe cases to maintain healthy hemoglobin levels.
Iron Chelation Therapy – Helps remove excess iron from the body caused by frequent transfusions.
Folic Acid Supplements – Supports red blood cell production.
Bone Marrow Transplant – A potential cure for some patients, but it carries risks.
Lifestyle and Diet Tips
Eat a Balanced Diet – Include iron-rich foods (if not overloaded), vitamin C (helps iron absorption), and calcium (for bone health).
Avoid Excess Iron – If undergoing transfusions, avoid iron supplements unless prescribed.
Stay Hydrated – Helps maintain healthy blood flow.
Exercise Moderately – Light activities like walking can boost energy levels.
Regular Check-ups
Regular visits to a hematologist (blood specialist) are crucial to monitor health and adjust treatments as needed.
When to See a Doctor
If you experience persistent fatigue, weakness, or symptoms of anemia, consult a doctor. If you have a family history of thalassemia, genetic testing can help determine your risk.
Need Help? Book a Consultation Today!
If you or a loved one is dealing with thalassemia, Apollo24|7 offers expert consultations and diagnostic tests to help manage the condition effectively. Schedule an appointment today for personalized care.
Conclusion
Thalassemia is a manageable condition with the right medical care and lifestyle adjustments. Understanding the different types, symptoms, and treatment options can help patients and families make informed decisions. If you suspect thalassemia, early diagnosis and proper management can lead to a healthier, more fulfilling life.
Consult top Hematologist
Consult top Hematologist

Dr Abilash Jain
General Physician/ Internal Medicine Specialist
12 Years • MBBS,DNB(FM),MNAMS,FIAMS,CCGMG(GERIATRICS),DGM (GERIATRICS),PGCD(DIABETES,BOSTON UNIVERSITY),FID(DIABETICS UK)CCEPC(PALLIATIVE CARE),CCCC(CRITICAL CARE)
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Ramalinga Reddy
General Physician
5 Years • MBBS MD General medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Niharendu Ghara
Paediatric Haematologist
20 Years • MBBS - Calcutta University , DCH- Calcutta University , MD Pathology - AllMS, New Delhi , MRCPCH- Royal College of Paediatrics & Child Health, UK , FRCPath (Haematology) - Royal College of Pathologists, UK , CCT (Haematology)- UK
Kolkata
Apollo Multispeciality Hospitals , Kolkata, Kolkata

.webp)