Guide to Orthopaedics/myths And Facts Total Knee Replacement Tkr
Is Total Knee Replacement (TKR) right for you? Separate fact from fiction. This essential guide debunks common myths about knee replacement surgery and recovery.


Introduction
If knee pain and stiffness from osteoarthritis are keeping you from walking, sleeping, or enjoying family life, you’ve probably heard plenty of mixed messages about total knee replacement (TKR). In orthopaedics, myths can spread quickly about everything from “you’re too young” to “implants only last 10 years” or “robotic surgery is always better.” This guide separates myths from facts so you can make confident, informed decisions. We’ll cover what TKR is, who it’s for, how long implants really last, pain and recovery timelines, risks and safety, activity and sports after surgery, and practical steps to prepare. You’ll also find data from leading orthopedic organizations and registries, unique tips to improve recovery, and clear next steps if you’re still unsure.
Designed for the general public looking for health care advice, this article uses plain language, modern evidence, and real-world insights to help you navigate orthopaedics/myths and facts about total knee replacement (TKR). If you’re not ready for surgery, we’ll outline non-surgical options too and when to consult a clinician for tailored advice.
What Is Total Knee Replacement—and Who Benefits?
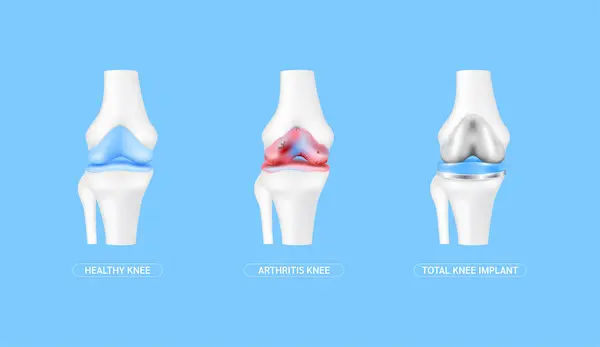
Total knee replacement (TKR) is a surgery that resurfaces the worn-out cartilage and bone of the knee with metal and
medical-grade plastic components to restore alignment, smooth joint motion, and relieve pain. It’s most commonly used to treat severe osteoarthritis when symptoms limit daily activities despite non-surgical treatments like physiotherapy, weight loss, bracing, pain relief, or injections.
During TKR, a surgeon removes a thin layer of damaged bone from the thighbone (femur) and shinbone (tibia), places metal caps on these surfaces, and inserts a polyethylene (plastic) spacer between them to create a smooth gliding surface. The patella (kneecap) may also be resurfaced. Implants are typically cobalt-chromium alloys, titanium, and ultra-high-molecular-weight polyethylene; modern designs aim to minimize wear and adapt to your knee’s natural kinematics.
Who benefits most? People with:
- Persistent pain and stiffness affecting walking, climbing stairs, and sleep
- Structural damage visible on X-ray (e.g., joint space narrowing, bone spurs)
- Limited function after trying conservative measures for months
- Knee deformity (varus “bow-legged” or valgus “knock-kneed”) causing imbalance
- Partial vs total knee replacement: If only one compartment of the knee is arthritic and ligaments are intact, a unicompartmental (partial) knee replacement may offer a smaller incision and faster recovery. But TKR is preferred when arthritis affects multiple compartments or stability is compromised. A shared decision with your surgeon will weigh anatomy, age, activity level, and goals.
- Unique insight: Think “function first.” Many patients wait for “perfect timing.” In reality, the best time is when your pain and disability limit what matters to you most—and non-surgical care has been given an honest try (often 3–6 months). If you can walk less than a few hundred meters, routinely need strong painkillers, or can’t sleep because of knee pain, it’s time to talk seriously about TKR. If symptoms persist beyond two weeks despite home measures, consult a doctor online with Apollo 24|7 for further evaluation.
Consult a Top Orthopaedics
Myth vs Fact: “There’s a right age for TKR”
- Myth: You’re either too young to risk an implant or too old to benefit.
Fact: Outcomes depend more on pain severity, function, overall health, and goals than age alone. Older adults often
gain substantial pain relief and mobility. Younger patients can also do well but may face a higher lifetime chance of
revision if they outlive the implant.
- Data snapshot: The Lancet meta-analysis of registry data found that about 90% of total knee replacements last at least 15 years, and roughly 82% last 25 years—a far cry from the “10-year” myth. These numbers apply across wide age ranges, though younger, more active patients have a slightly higher revision risk because they put more cycles on the implant.
- How function guides timing: If osteoarthritis significantly restricts daily activities despite non-surgical care, the balance often favors TKR—regardless of whether you’re 50 or 80. On the other hand, if pain is intermittent and you still function well, you may safely wait.
- Unique insight: Your “biologic age” (fitness, metabolic health, muscle strength) matters more than your birthday. Prehab—targeted strengthening and flexibility work before surgery—improves early function and confidence (related term: prehab before knee replacement exercises) and may shorten hospital stay. Ask your team about a prehab plan suited to you.
Myth vs Fact: “Knee replacements only last 10 years”
- Myth: All implants wear out quickly.
Fact: Modern implants frequently last 15–25 years and beyond. In robust analyses of national joint registries and long-
term studies, about 90% of TKRs last 15 years and roughly 82% last 25 years [3, 7]. Longevity has improved thanks to
better polyethylene, implant design, and surgical techniques.
What influences longevity:
- Alignment and soft-tissue balance: Precise positioning reduces uneven wear.
- Activity level: Low-impact activities are encouraged; repetitive high-impact may accelerate wear.
- BMI and bone quality: Excess load can stress implants and surrounding bone.
- Infection risk: A deep infection can necessitate revision; prevention is key (see risk section).
- Unique insight: Think of your TKR like a high-performance “mechanical cartilage.” It loves steady, controlled motion.
Activities such as cycling, swimming, walking, and doubles tennis keep you strong without punishing the joint (long-
tail: how long does a knee replacement last 20 years).
Myth vs Fact: “Pain after TKR is unbearable”
- Myth: Expect weeks of agony with little relief.
Fact: Pain is real, but modern ERAS (Enhanced Recovery After Surgery) protocols, regional nerve blocks, and multimodal non-opioid medications mean most patients walk the day of surgery and report significant improvement within weeks [4, 5]. Hospital stays are often 1–3 days; some centers offer same-day discharge for healthy patients [4].
Realistic timeline (typical, not guaranteed):
- Day 0–1: Stand and walk with a walker; start physiotherapy immediately.
- Week 1–2: Swelling and tightness common; pain manageable with ice, elevation, and medications.
- Week 3–6: Many resume driving (right leg TKR often 4–6 weeks after reaction times normalize) and light household
tasks [5]. - Month 3: Most patients report marked pain reduction and improved function.
- Month 6–12: Strength, balance, and endurance continue to improve.
Tips that help:
- Prehab strengthens quads and glutes, improving early steps.
- Ice, elevation, and compression reduce swelling.
- Good sleep hygiene and nutrition support healing.
- Set daily “minimums” for exercises; consistency beats intensity.
Unique insight: The single biggest early win is regaining extension (getting the knee straight) and functional flexion
(usually at least 100–110 degrees). Track range of motion daily during the first 6 weeks. If progress stalls or pain
escalates, consult your care team. If your condition does not improve after trying these methods, book a physical visit to
a doctor with Apollo 24|7.
Myth vs Fact: “Robotic TKR is always better”
- Myth: Robotics guarantees a superior knee.
Fact: Robotic or computer-assisted systems can help with alignment and planning, which may reduce outliers in
component positioning. However, evidence for consistently better pain scores, function, or long-term survivorship compared to well-executed conventional TKR remains mixed, and costs are often higher [1, 6]. Surgeon experience with their chosen technique (robotic or conventional) is a major determinant of outcomes.
Benefits robotics can offer:
- 3D planning tailored to your anatomy
- Potentially more consistent alignment and soft-tissue balance
- Intraoperative feedback and bone-sparing cuts
What it doesn’t guarantee:
- A pain-free knee
- Faster recovery
- Longer implant survival in all cases
Unique insight: Choose the surgeon, not just the tool. Ask about your surgeon’s personal outcomes (complication rates, revision rates, infection rates), their volume, and how they tailor technique—robotic or not—to your knee (long-tail: robotic knee replacement pros and cons).
Myth vs Fact: “You’ll be bedridden for months”
- Myth: Recovery is slow and immobilizing.
Fact: Most patients are up and walking the same day with a walker or crutches, and stair training begins within 24–48
hours. With a structured recovery timeline after knee replacement surgery, patients typically:
- Walk household distances within days
- Navigate stairs with support by week 1–2
- Return to desk work in 2–4 weeks (job-dependent)
- Drive at 4–6 weeks for right-sided TKR (once off narcotics and reaction times normalize)
- Return to low-impact sports over 2–3 months
Prehab and physiotherapy unlock mobility faster. Even modest prehab (2–6 weeks) improves early strength and confidence. After surgery, aim for short, frequent walks and prescribed exercises (heel slides, quads sets, straight-leg raises) to build a virtuous cycle: motion reduces stiffness, which reduces pain, which enables more motion.
Unique insight: Recovery is not linear. Expect plateaus and occasional “backwards” days. Use a weekly progress lens (steps per day, ROM goals) rather than obsessing over single-day setbacks.
Myth vs Fact: “Replace both knees at once—it’s faster”
- Myth: Simultaneous bilateral TKR halves the hassle.
Fact: Replacing both knees in one surgery can reduce total recovery time and anesthesia exposure. However, it
increases surgical stress, blood loss, transfusion rates, and early complication risk in some patients [1]. Staged TKR (separate surgeries weeks or months apart) often spreads out risk and rehab.
Who might qualify for same-day bilateral?:
- Good overall health (low cardiovascular and pulmonary risk)
- Strong prehab completion and home support
- No significant anemia, uncontrolled diabetes, or active infections
Who may benefit from staged?:
- Older adults or those with significant comorbidities
- Patients needing a gentler, more predictable recovery arc
Unique insight: Consider your home setup and caregiver capacity. Bathing, meal prep, and mobility support are twice as complex with both knees done concurrently (long-tail: bilateral knee replacement same day vs staged). A short phone consult can help clarify your best path; if unsure, consult a doctor online with Apollo 24|7.
Myth vs Fact: “High BMI means I can’t have surgery”
- Myth: Obesity automatically disqualifies you.
Fact: A higher BMI raises risks (infection, wound healing issues, blood clots), but it isn’t an absolute barrier. Many
patients with elevated BMI achieve major pain relief and better function after TKR [1]. Surgeons and hospitals may suggest a target BMI range or weight loss plan to reduce complications and improve long-term outcomes.
- Optimize your odds:
Weight management: Even a 5–10% loss reduces joint load.
- Diabetes control: Aim for an individualized HbA1c target; better control lowers infection risk.
- Smoking cessation: Improves wound healing and reduces respiratory risks.
- Nutrition: Adequate protein and vitamin D support bone and soft-tissue recovery; Apollo 24|7 offers a convenient home
collection for tests like vitamin D or HbA1c.
Unique insight: Focus on “metabolic fitness” (blood sugar, blood pressure, sleep, and activity) for 6–12 weeks pre-op. It’s not just the number on the scale—it’s the physiology behind it.
Myth vs Fact: “No sports or kneeling after TKR”
- Myth: You’ll have to give up active life.
Fact: Low-impact activities are not only safe, but encouraged—walking, cycling, swimming, elliptical, golf, and doubles
tennis are common choices [1]. High-impact activities (running, singles tennis, basketball) may increase wear and risk over time and are generally discouraged.
- Kneeling after total knee replacement: Many patients avoid kneeling due to discomfort or fear, but kneeling is not
harmful for most TKRs once tissues heal. Desensitization (gradual exposure), padding, and practice with a
physiotherapist can help. Some may always find it uncomfortable, but discomfort is different from danger. - Unique insight: Program your return to sport in phases—range of motion and balance first, then strength and endurance, then sport-specific drills. Treat your new knee like an athlete’s comeback (long-tail: return to work after TKR; kneeling after total knee replacement safety).
Myth vs Fact: “Cementless is better for everyone”
- Myth: Newer automatically means better.
Fact: Cemented implants have decades of strong results and remain the most common worldwide. Cementless implants can bond biologically to bone and are increasingly used, especially in younger patients with good bone quality. Evidence suggests both approaches can work very well when matched to the right patient and technique [1].
Pros and cons:
- Cemented: Immediate fixation, proven track record; may be better in osteoporotic bone.
- Cementless: Potential long-term biological fixation; requires good bone quality and precise press-fit.
- Unique insight: The right choice is personalized. Ask how your bone quality, activity level, and anatomy inform implant selection (long-tail: cemented vs cementless knee implants).
Myth vs Fact: “Infections and clots are unavoidable”
- Myth: Complications are common and inevitable.
- Fact: Serious complications are uncommon—and rigorous prevention protocols cut risk further. Deep infection rates after primary TKR are typically around 1–2%, and blood clots (DVT/PE) are also low with modern prophylaxis.
Teams use antibiotics, antiseptic skin prep, optimized blood sugar control, early mobilization, and blood-thinning
medications to protect you.
Know the red flags:
- Infection: Increasing redness, warmth, drainage, fever, or worsening pain after an initial improvement
- Clots: Calf swelling, pain, redness; sudden chest pain or shortness of breath (urgent)
If you notice these symptoms, seek urgent medical attention. If symptoms persist beyond two weeks or you’re unsure, consult a doctor online with Apollo 24|7 for further evaluation (long-tail: deep vein thrombosis after knee surgery prevention; infection after knee replacement signs and symptoms).
Myth vs Fact: “Surgery is the only option that works”
- Myth: Nothing else helps advanced osteoarthritis.
Fact: Non-surgical care can meaningfully reduce pain and improve function for many: activity modification, weight
loss, physiotherapy, bracing, topical NSAIDs, oral pain relief, and injections (e.g., corticosteroids for short-term relief). That said, when severe pain and disability persist, NICE and other guidelines support TKR as a highly effective option with durable results in appropriately selected patients.
Try this progression:
- 6–12 weeks of supervised physiotherapy focusing on strength and mobility
- Weight loss (if needed), footwear/orthotics review, and sleep optimization
- Trial of medications and possibly an injection for symptom relief
- Reassess function and quality of life
If you continue to struggle, talk through risks, benefits, and expectations of TKR (long-tail: partial vs total knee replacement). If you need guidance on personalized options, consult a doctor online with Apollo 24|7.
Preparing for TKR: a step-by-step checklist
Medical optimization: Check blood pressure, blood sugar, anemia, and vitamin D. Review medications (blood thinners,
immunosuppressants). Apollo 24|7 offers a convenient home collection for tests like vitamin D or HbA1c. Stop
smoking and moderate alcohol.
- Prehab: 2–6 weeks of targeted strength and flexibility, focusing on quads, hip abductors, and hamstrings. Practice
transfers (bed/chair) and stair technique. - Home safety: Prepare a clear walking path, remove loose rugs, set up a firm chair with arms, arrange a bedside
commode if needed, and place frequently used items at waist level. - Caregiver plan: Identify who helps with meals, transport, and wound care for the first 1–2 weeks.
- Nutrition: Prioritize protein, hydration, and fiber to support healing and bowel regularity.
- Surgical planning: Discuss anesthesia options, DVT prevention, pain plan (nerve block, multimodal analgesia), and
discharge plan (home vs short rehab). - Choosing a surgeon: Ask about volume, outcomes (infections, readmissions, revisions), implant philosophy (cemented
vs cementless), and approach (robotic vs conventional).
Costs, insurance, and access: what to expect?
Costs vary by region, hospital, implant type, use of robotic systems, and length of stay. Factors that influence price
include:
- Implant design and brand (specialized implants may cost more)
- Robotic or navigation technologies
- Private room vs general ward; length of stay and rehab needs
- Pre-op tests, imaging, and post-op physiotherapy
Insurance: Many plans cover medically necessary TKR after documentation of failed conservative care.
Preauthorization is often required. Ask your insurer:
- Is TKR covered? What are my deductibles/copays?
- Are robotics covered or considered premium?
- How many PT sessions are included?
- What are preferred hospital networks?
Unique insight: Consider the total episode cost—prehab, surgery, and rehab—not just the operating room fee. A center with strong ERAS and low complications may reduce overall costs.
Unique perspectives: what most guides don’t tell you
- Your at-home scorecard: Track daily ROM (aim for near-full extension and 90+ degrees flexion by 2–3 weeks), steps
per day, and pain at rest vs activity. Weekly trends matter more than single days. - The second-month slump: Around weeks 4–8, many feel “stuck.” Normal. Swelling lingers, and gains are subtler.
Introduce variety (stationary bike intervals, pool therapy) and celebrate small wins. - Pain medication taper: Plan a gradual reduction with your team. Combine scheduled non-opioid meds (unless
contraindicated) with ice/elevation. If you’re still reliant on opioids beyond 2–3 weeks, discuss a taper plan and
alternative strategies with your clinician.
Conclusion
Total knee replacement is one of the most successful procedures in orthopaedics, with decades of data showing durable pain relief and meaningful improvement in daily life. While myths abound—from age limits to inevitable complications—the facts paint a more hopeful picture: most implants last far longer than 10 years, recovery protocols are gentler, and you can return to an active lifestyle with the right plan. The best outcomes come from informed, shared decisions grounded in your goals, overall health, and the specifics of your knee. Use this guide to benchmark your expectations, prepare your home and support team, and have productive conversations with your surgeon about options such as cemented vs cementless implants or robotic assistance. If you’re uncertain whether you’re ready for surgery—or want to maximize non-surgical care first—consult a clinician. If symptoms persist beyond two weeks or your function continues to decline, consult a doctor online with Apollo 24|7 for further evaluation or to book a physical visit. With clear information, a strong prehab-rehab approach, and a team you trust, you can move from “Can I?” to “I did.”
Consult a Top Orthopaedics
Consult a Top Orthopaedics

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
Consult a Top Orthopaedics

Dr. Anil Pradeep Jadhav
Orthopaedician
23 Years • MBBS MS (Ortho)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr. Rupam Chowdhury
Orthopaedician
10 Years • MBBS, DNB (Ortho.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Suraj Prakash
Orthopaedician
5 Years • MBBS, MS (Ortho)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru

Dr. Padam Singh Gautam
General Physician/ Internal Medicine Specialist
43 Years • M.B.B.S (WARDHA M. S.), F.A.G.E. (MANIPAL), F.A.I.M.S. (Pb.), M.A.I.M.S. (Pb.), M.R.S.H. (LONDON)
Noida
Dr Padam Singh Gautam Fracture Clinic, Noida

Dr. Susheel B
Orthopaedician
13 Years • MBBS, MS, Ortho Fellowship in Trauma ( Germany) Fellowship in Arthroscopy and Arthroplasty ( Switzerland)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
More articles from Total Knee Replacement
Frequently Asked Questions
How long does a knee replacement last on average?
Many last 15–25 years; around 90% survive at least 15 years and roughly 82% at 25 years, depending on factors like alignment, activity, and BMI (how long does a knee replacement last 20 years).
When can I drive after TKR, especially if it’s my right leg?
Typically 4–6 weeks for right-leg TKR, after you’re off narcotics and your reaction time is back to normal. Left-leg TKR may be sooner for automatic transmissions. Confirm with your surgeon.
3) Is robotic knee replacement worth it?
Robotics may improve alignment and consistency, but doesn’t guarantee better pain relief or function than skilled conventional surgery. Discuss robotic knee replacement pros and cons relative to your anatomy and cost.
4) Can I kneel after total knee replacement?
Yes, kneeling is often safe after healing, though some find it uncomfortable. Gradual desensitization, padding, and guided practice can help (kneeling after total knee replacement safety).
What are the major risks and how are they prevented?
Infection (~1–2%), blood clots, stiffness, and rare anesthesia complications. Teams use antibiotics, careful sterile technique, DVT prophylaxis, and early mobilization to reduce risk. If you notice redness, warmth, drainage, calf swelling, chest pain, or shortness of breath, seek urgent care.