Guide to Tuberculosis Myths And Facts
Separate TB facts from fiction. This guide debunks common tuberculosis myths, covering transmission, treatment, and prevention to help you understand this disease better.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
Tuberculosis, often shortened to TB, is a name that echoes through history, conjuring images of sanatoriums and a once-incurable illness. While modern medicine has made incredible strides, the shadow of tuberculosis myths continues to persist, often causing more harm than the disease itself. Misinformation fuels stigma, delays diagnosis, and prevents people from seeking the effective treatment that is available today. This article aims to clear the air by confronting these misconceptions head-on. We will sift through the folklore and fear to present the clear, evidence-based facts about TB. Whether you're concerned about your own health, that of a loved one, or simply want to be better informed, this guide will empower you with accurate knowledge about tuberculosis transmission, symptoms, and the reality of modern treatment. Understanding the truth is the first step towards eradicating both the disease and the stigma that surrounds it.
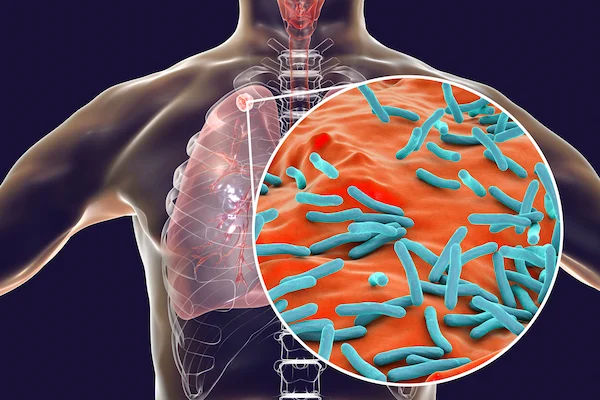
What exactly is Tuberculosis?
Tuberculosis is an infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs (pulmonary TB) but can also spread to other parts of the body, such as the kidneys, spine, and brain (extrapulmonary TB). It's crucial to understand that not everyone infected with the bacteria becomes sick, which leads to the critical distinction between two states of TB.
Latent TB Infection (LTBI) vs. Active TB Disease
This is the most important concept in understanding TB.
- Latent TB Infection (LTBI): In this state, the TB bacteria live in the body in an inactive form. They cause no symptoms and are not contagious. The person's immune system effectively "walls off" the bacteria. However, the bacteria are still alive and can become active later if the immune system weakens. An estimated one-quarter of the world's population has LTBI.
- Active TB Disease: This is when the bacteria multiply and make the person sick. People with active TB disease are symptomatic and can spread the bacteria to others. The lifetime risk of someone with LTBI developing active disease is 5-10%, with the highest risk in the first two years after infection.
Top 10 Tuberculosis Myths Debunked by Science
Let's dismantle the most common and damaging myths one by one.
Consult Top Specialists
TB is a Disease of the Past
Fact: TB remains one of the world's top infectious killers. According to the World Health Organization (WHO), in 2022, an estimated 10.6 million people fell ill with TB, and 1.3 million died from it. It is very much a present and significant public health challenge, especially in developing countries.
TB is Highly Contagious and Easy to Catch
Fact: TB is not as contagious as diseases like the flu or measles. It requires prolonged, close contact to spread. You cannot get TB by briefly shaking hands, sharing food, or touching a surface. It spreads through the air when a person with active pulmonary TB coughs, sneezes, or speaks, releasing tiny droplets containing the bacteria.
TB Always Makes You Cough Up Blood
Fact: While coughing up blood or sputum can be a symptom of advanced lung TB, it is not universal. Many people with active TB disease experience a persistent cough for three weeks or more, chest pain, fatigue, weight loss, fever, and night sweats. Relying solely on the expectation of coughing blood can lead to a dangerous delay in diagnosis.
TB is a Death Sentence
Fact: This is perhaps the most critical myth to dispel. Tuberculosis is curable with proper medical treatment. The vast majority of TB cases can be treated successfully with a standard course of antibiotics taken for 6-9 months. Adherence to the medication regimen is key to a complete cure.
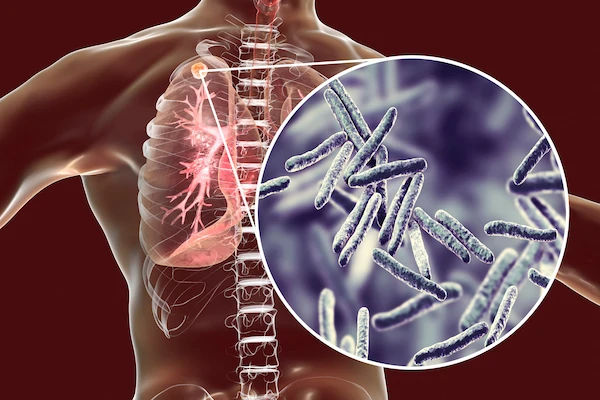
TB Only Affects the Lungs
Fact: While pulmonary TB is the most common form, the bacteria can travel through the bloodstream to other organs, causing extrapulmonary TB. This can affect the lymph nodes, bones, brain, kidneys, and spine. The symptoms of tuberculosis in these cases depend on the organ involved.
Myth 6: TB is Genetic and Runs in Families
Fact: TB is an infectious disease, not a genetic one. It spreads through bacteria, not genes. However, families living in close quarters are at higher risk of transmission if one member has active TB. What may appear to be a "family history" is actually a history of exposure.
Myth 7: If You Have TB, You Must Be Isolated Forever
Fact: Isolation is typically temporary. Patients with active pulmonary TB are often advised to isolate themselves initially to prevent spread. However, after being on effective treatment for a few weeks, they usually become non-contagious and can resume normal activities. This underscores the importance of starting treatment immediately.
Myth 8: TB Medicine is Always Toxic and Ineffective
Fact: Modern TB drugs are highly effective when taken as prescribed. While all medications can have side effects, most are manageable. The biggest threat to treatment is not the medicine itself but non-adherence, which can lead to drug-resistant TB (MDR-TB), a much more complex condition to treat.
Myth 9: Only People with HIV Get TB
Fact: While HIV significantly weakens the immune system and greatly increases the risk of progressing from LTBI to active TB disease, anyone can get TB. Other risk factors include diabetes, malnutrition, smoking, and being on immunosuppressive therapy.
Myth 10: There's a Vaccine, So I'm Fully Protected
Fact: The Bacille Calmette-Guérin (BCG) vaccine is used in many countries to protect infants and young children from severe forms of TB, like TB meningitis. However, it is not very effective at preventing pulmonary TB in adults. The BCG vaccine is not a guarantee against infection.
The Real Facts About TB Transmission and Symptoms
How TB is Actually Spread
Transmission requires an infected source and susceptible host. The process is straightforward: an individual with active pulmonary TB releases bacteria into the air by coughing. Another person nearby inhales these bacteria-laden droplets. The risk is highest in enclosed, poorly ventilated spaces over a long period (e.g., living in the same household).
Recognizing the Signs: Common Symptoms of Active TB
Knowing the signs and symptoms of tuberculosis is vital for early diagnosis. General symptoms include:
- A persistent cough lasting more than three weeks
- Chest pain, or pain with breathing or coughing
- Unintentional weight loss
- Fatigue and weakness
- Fever and chills
- Night sweats
If you experience a persistent cough accompanied by any of these other symptoms for more than two weeks, it is essential to consult a doctor. You can book a quick online consultation with a specialist on Apollo24|7 to discuss your concerns and determine if further testing is needed.
Diagnosis and Modern Treatment for Tuberculosis
How is TB Diagnosed?
Diagnosis involves a few key steps:
1. Medical History and Physical Exam: A doctor will ask about symptoms and potential exposure.
2. Tuberculin Skin Test (TST) or IGRA Blood Test: These tests determine if you have been infected with TB bacteria (LTBI). They cannot distinguish between latent and active infection.
3. Chest X-ray: This can reveal signs of active TB in the lungs.
4. Sputum Tests: The definitive diagnosis for pulmonary TB involves examining sputum (phlegm) under a microscope and culturing it to identify the bacteria. Apollo24|7 offers convenient home collection for lab tests, including sputum samples, making the diagnostic process smoother.
The Road to Recovery: TB Treatment Protocols
Treatment depends on whether a person has LTBI or active disease.
- Latent TB Infection (LTBI): Treatment with one or two antibiotics for 3-9 months is often recommended to prevent the infection from becoming active.
- Active TB Disease: The standard treatment for tuberculosis is a combination of several antibiotics taken for 6-9 months. It is absolutely crucial to take every dose exactly as prescribed for the full duration, even after you start feeling better. Stopping early can lead to relapse and drug resistance.
Programs like Directly Observed Therapy (DOT), where a healthcare worker watches the patient take each dose, can ensure success.
Key Takeaways: Tuberculosis Myths and Facts
- TB is a current, curable disease, not a relic of the past.
- It requires prolonged close contact to spread; it's not highly contagious like the flu.
- A persistent cough for more than 2 weeks, with weight loss or fever, warrants a doctor's visit.
- The critical difference is between non-contagious Latent TB Infection and contagious Active TB Disease.
- Completing the full course of medication is essential for a cure and preventing drug-resistant TB.
- Stigma, fueled by myths, is a major barrier to treatment and must be overcome with facts.
Conclusion
Navigating the world of health information can be challenging, especially with a disease like tuberculosis that carries historical baggage. By separating the tuberculosis myths from the life-saving facts, we empower ourselves and our communities. The reality is that TB is a manageable and curable disease with timely diagnosis and consistent treatment. The most powerful tools we have are accurate knowledge, reduced stigma, and access to quality healthcare. If you have any concerns about tuberculosis symptoms or potential exposure, do not let fear or misinformation prevent you from seeking help. Modern medicine offers clear paths to diagnosis and recovery. Taking action early is the best step towards protecting your health and the health of those around you.
Consult Top Specialists
Consult Top Specialists

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. P Sravani
Pulmonology Respiratory Medicine Specialist
3 Years • MBBS, MD
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam
Dr. Ambuj Kumar
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS, MD (Pulmonary Medicine)
New Delhi
Smriti Gynaecology and Lung Centre, New Delhi

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. K Prasanna Kumar Reddy
Pulmonology Respiratory Medicine Specialist
16 Years • MBBS, DTCD (TB&CHEST), DNB (PULM MED), FCCP
Hyderabad
Apollo Medical Centre Kondapur, Hyderabad
Consult Top Specialists

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. P Sravani
Pulmonology Respiratory Medicine Specialist
3 Years • MBBS, MD
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam
Dr. Ambuj Kumar
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS, MD (Pulmonary Medicine)
New Delhi
Smriti Gynaecology and Lung Centre, New Delhi

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)

Dr. K Prasanna Kumar Reddy
Pulmonology Respiratory Medicine Specialist
16 Years • MBBS, DTCD (TB&CHEST), DNB (PULM MED), FCCP
Hyderabad
Apollo Medical Centre Kondapur, Hyderabad
More articles from Tuberclosis
Frequently Asked Questions
Can TB come back after successful treatment?
Yes, but it's uncommon. Most people are cured with a full course of treatment. Recurrence is usually due to reinfection from a new source or, rarely, relapse if the initial bacteria were not fully eradicated. Following the treatment plan precisely minimizes this risk.
Is there a difference between TB of the lungs and TB in other parts of the body?
Yes. Pulmonary TB affects the lungs and is contagious. Extrapulmonary TB affects other organs and is generally not contagious to others. However, the treatment for both forms involves a combination of antibiotics.
What are the side effects of TB medication?
Common side effects can include nausea, loss of appetite, jaundice (yellowing skin), and dark urine. Some can affect vision or cause tingling in the hands/feet. It's vital to report any side effects to your doctor immediately; they can often manage them without stopping treatment.
How can I protect my family if I am diagnosed with TB?
Follow your doctor's instructions on initial isolation. Ensure good ventilation at home, cover your mouth when coughing, and most importantly, start and adhere to your medication regimen. Your family members should be tested for exposure.
What is drug-resistant TB?
Drug-resistant TB occurs when the bacteria become immune to the standard first-line drugs. This can happen due to incorrect or incomplete treatment. It is more complex and time-consuming to treat, requiring longer courses of more toxic, second-line drugs.