Insulin Resistance Causes and Surprising Triggers
Learn about the causes and surprising triggers of insulin resistance, and discover lifestyle tips to help manage and prevent it effectively.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026
Introduction
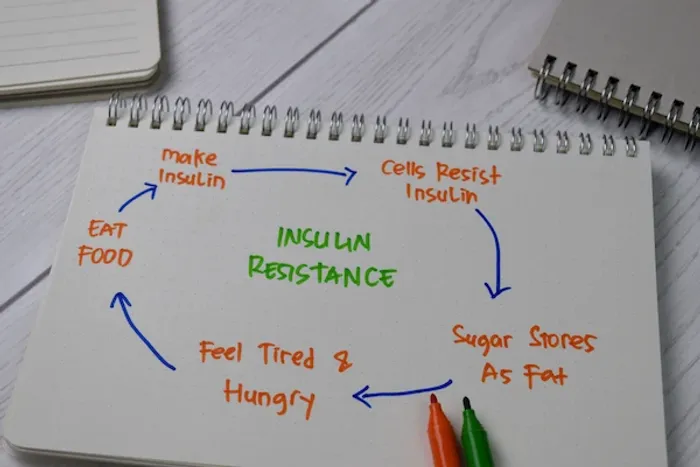
Have you ever felt unusually tired after a meal, struggled with stubborn weight gain around your midsection, or found yourself constantly craving sugary snacks? These could be more than just signs of a busy life; they might be your body's way of signalling an underlying metabolic issue known as insulin resistance. This condition is a silent precursor to type 2 diabetes and affects millions of people, often without them knowing. But what exactly is it, and what leads to this metabolic roadblock? In simple terms, insulin resistance occurs when your body's cells stop responding effectively to the hormone insulin. Imagine insulin as a key designed to unlock your cells' doors to let glucose (sugar) in for energy. With insulin resistance, the key doesn't turn smoothly, leaving sugar stranded in your bloodstream. This article will demystify the primary and often surprising triggers of insulin resistance, moving beyond the usual suspects to explore the intricate roles of inflammation, stress, sleep, and even your gut health. Understanding these causes is the first powerful step toward reclaiming your metabolic health.
Understanding Insulin: The Key to Your Cells
Insulin plays a vital role in how your body uses energy and regulates blood sugar.
The Normal Process: How Insulin is Supposed to Work
Insulin is a vital hormone produced by the beta cells in your pancreas. After you eat a meal, especially one containing carbohydrates, your digestive system breaks down the food into glucose, which enters your bloodstream. In response, your pancreas releases insulin into the blood. Insulin's primary job is to act as a messenger, signalling to cells throughout your body, particularly in the muscles, liver, and fat, to open up and absorb this glucose. This process efficiently lowers your blood sugar levels and provides your cells with the energy they need to function. It's a finely tuned system that keeps your metabolism in perfect balance.
Insulin Resistance: When the Key Stops Fitting the Lock
Insulin resistance begins when this efficient system starts to falter. For reasons we'll explore, your cells become less sensitive or "resistant" to insulin's signal. It's as if the locks on the cells' doors have become rusty or damaged. The key (insulin) is still there, but it doesn't open the door as easily. In response, your pancreas goes into overdrive, producing even more insulin to force the glucose into the resistant cells. This state of elevated insulin in the blood is known as hyperinsulinaemia. For a while, this compensatory mechanism works, and your blood sugar levels may remain normal. However, over time, the overworked beta cells in the pancreas can become exhausted and fail to produce enough insulin, leading to a rise in both insulin and blood sugar levels, eventually resulting in prediabetes and type 2 diabetes.
Consult an Endocrinologist for the best advice
The Primary Culprits: Major Causes of Insulin Resistance
Identifying the main factors behind insulin resistance can help you take control of your health.
Excess Body Fat, Especially Belly Fat
Carrying excess weight, particularly visceral fat that accumulates deep within the abdomen around your organs, is one of the strongest predictors of insulin resistance. This isn't just inactive storage fat; it's metabolically active tissue that pumps out a constant stream of pro-inflammatory chemicals and free fatty acids into the bloodstream.
The Role of Chronic Inflammation from Fat Cells
This is a critical mechanism. The inflammatory signals released by excess fat cells, such as TNF-alpha and IL-6, interfere with the insulin signalling pathways inside your cells. They essentially jam the communication lines, preventing the insulin signal from being properly received. This state of low-grade, chronic inflammation is a direct driver of cellular insulin resistance. Therefore, reducing body fat, particularly abdominal fat, is one of the most effective ways to improve insulin sensitivity.
A Sedentary Lifestyle: When Muscles Stop Listening
Muscle tissue is the largest consumer of glucose in your body. When you are physically active, your muscles are primed to absorb glucose efficiently, even without the need for large amounts of insulin. Conversely, a sedentary lifestyle makes your muscles "lazy." They require a stronger insulin signal to take up glucose. Regular exercise, especially a combination of strength training and aerobic activity, directly counteracts this by making your muscle cells more sensitive to insulin. It creates more "doors" (glucose transporters called GLUT4) on the muscle cells, making it easier for glucose to enter. This is why exercise for insulin sensitivity is non-negotiable.
The Modern Diet: Sugar, Carbs, and Processed Foods
The typical Western diet, high in refined carbohydrates, added sugars, and processed foods, is a perfect storm for inducing insulin resistance. Consistently high blood sugar spikes demand consistently high insulin release. Over time, this can lead to the downregulation of insulin receptors on cells; they essentially "turn down the volume" because the signal is always too loud.
The Impact of Fructose on Liver Health
A unique problem comes from high fructose consumption, particularly from sugar-sweetened beverages and processed foods. Unlike glucose, which is metabolised by all cells, fructose is primarily processed in the liver. Excessive fructose intake can lead to non-alcoholic fatty liver disease (NAFLD), where fat builds up in the liver. A fatty liver is highly inflamed and contributes significantly to hepatic insulin resistance, meaning the liver becomes less responsive to insulin's command to stop producing glucose. This dual problem of muscle and liver resistance accelerates metabolic dysfunction.
Hidden Drivers: Less Obvious Factors
Some causes of insulin resistance aren’t immediately obvious but can significantly impact your health.
Chronic Stress and The Cortisol Connection
When you're stressed, your body releases the hormone cortisol. Cortisol's evolutionary purpose is to provide a quick energy source in a "fight or flight" situation by raising blood sugar. However, in our modern lives, chronic stress leads to perpetually elevated cortisol levels. This constant signal to release sugar into the blood forces your pancreas to produce more insulin to manage it, contributing to the cycle of insulin resistance. Managing stress is thus a key, though often overlooked, part of managing blood sugar.
Poor Sleep Quality and Disrupted Circadian Rhythms
Sleep is not a luxury; it's a metabolic necessity. Just one night of poor sleep can induce a state of temporary insulin resistance. Chronic sleep deprivation or disorders like sleep apnoea disrupt the delicate balance of hormones that regulate appetite (ghrelin and leptin) and stress (cortisol). It also promotes inflammation. This combination makes your cells less responsive to insulin. Prioritising 7-9 hours of quality sleep is a powerful tool for metabolic health.
Gut Health: The Surprising Link Between Your Microbiome and Metabolism
Emerging research highlights a fascinating connection between the trillions of bacteria in your gut (your microbiome) and insulin sensitivity. An imbalance in gut bacteria, known as dysbiosis, can contribute to a "leaky gut," where bacterial toxins called lipopolysaccharides (LPS) leak into the bloodstream. These toxins trigger widespread inflammation, which, as we now know, directly interferes with insulin signalling. A diet rich in diverse fibres, fermented foods, and prebiotics can help cultivate a healthy gut microbiome that supports metabolic health.
Genetic and Medical Factors
While lifestyle is the dominant factor for most people, genetics can predispose someone to insulin resistance. A family history of type 2 diabetes increases your risk. Certain ethnicities, including South Asian, African, Hispanic, and Native American populations, also have a higher predisposition. Furthermore, conditions like Polycystic Ovary Syndrome (PCOS) are intrinsically linked to insulin resistance, as are hormonal disorders like Cushing's syndrome and severe sleep apnea. It's also important to note that certain medications, such as high-dose steroids, some antipsychotics, and HIV medications, can induce insulin resistance. If you are on long-term medication and are concerned about your metabolic health, it's important to discuss this with your doctor.
How is Insulin Resistance Diagnosed?
There isn't one single test, but doctors use a combination of markers. The most common is the HbA1c test, which measures your average blood sugar levels over the past three months. A result between 5.7% and 6.4% indicates prediabetes. A fasting blood glucose test and a fasting insulin test can also be used; a high fasting insulin level is a clear sign that your body is struggling with resistance. The gold-standard test is the oral glucose tolerance test (OGTT). Apollo24|7 offers convenient home collection for tests like HbA1c, making it easier to monitor these important health markers.
Get Your Health Assessed
Conclusion: Reversing the Trend is Possible
Understanding what leads to insulin resistance empowers you to take control of your metabolic health. While the list of causes, from belly fat and poor diet to stress and sleep deprivation, may seem daunting, the crucial takeaway is that these are largely reversible factors. Insulin resistance is not a life sentence; it's a warning sign. By adopting a whole-foods diet rich in fibre and healthy fats, incorporating regular physical activity into your routine, managing stress through mindfulness or hobbies, and prioritising restorative sleep, you can significantly improve your body's sensitivity to insulin. These changes work synergistically to reduce inflammation, optimise hormone function, and allow your cells to "hear" insulin's signal clearly once again. The journey to better health begins with a single step. If symptoms persist or you need a personalised plan, consult a doctor online with Apollo24|7 for further evaluation and guidance.
Consult an Endocrinologist for the best advice
Consult an Endocrinologist for the best advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)
Aditya Singh
Endocrinologist
8 Years • MBBS
Bengaluru
Apollo One Electronic City, Bengaluru
Dr Venkata Naga Sai Tribhushan Rambhatla
General Physician
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Shruthi B
Endocrinologist
20 Years • MBBS,MD ( GEN MED) DM (ENDOCRIONOLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Consult an Endocrinologist for the best advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)
Aditya Singh
Endocrinologist
8 Years • MBBS
Bengaluru
Apollo One Electronic City, Bengaluru
Dr Venkata Naga Sai Tribhushan Rambhatla
General Physician
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Shruthi B
Endocrinologist
20 Years • MBBS,MD ( GEN MED) DM (ENDOCRIONOLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
More articles from Type 2 Diabetes Treatment
Frequently Asked Questions
1. What are the first signs of insulin resistance?
Often, there are no obvious symptoms initially. However, early signs can include severe fatigue (especially after meals), intense cravings for sugar and carbs, difficulty losing weight (particularly around the abdomen), and skin changes like dark patches (acanthosis nigricans) in the armpits or neck.
2. Can you reverse insulin resistance completely?
Yes, in many cases, insulin resistance can be significantly reversed through consistent lifestyle changes. Weight loss, dietary improvements, and increased physical activity are the most effective strategies. The earlier you address it, the greater the chance of full reversal.
3. What is the best diet for someone with insulin resistance?
A diet focused on whole, unprocessed foods is key. Emphasise non-starchy vegetables, lean proteins, healthy fats (like avocados, nuts, and olive oil), and high-fibre, low-sugar fruits. The goal is to minimise blood sugar spikes by reducing refined carbohydrates and added sugars.
4. How does insulin resistance lead to type 2 diabetes?
When cells are resistant, the pancreas overproduces insulin to compensate. Over years, the insulin-producing beta cells in the pancreas become exhausted and can no longer keep up with the demand. This leads to a rise in blood sugar levels, progressing from prediabetes to type 2 diabetes.
5. Are there specific exercises that are best for improving insulin sensitivity?
Both aerobic exercise (like brisk walking, cycling, swimming) and resistance training (weight lifting, bodyweight exercises) are highly beneficial. Resistance training is particularly effective because it builds muscle mass, which is a primary site for glucose disposal.





