Urinary Tract Infection Overview
Get the facts on UTIs. Learn about the causes, common symptoms, effective treatments, and prevention tips for urinary tract infections in our comprehensive overview.

Written by Dr. Siri Nallapu
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026
Urinary tract infections represent a frequent pathogenetic event with a profound discomfort threshold, afflicting populations annually in significant numbers. The prototypical nociceptive symptom—dysuria accompanied by a cumulative frequent micturition reflex—provides a practical diagnostic clue. Notwithstanding the symptom severity, the therapeutic trajectory is characteristically straightforward upon the institution of evidence-based protocols.
This therapeutic memorandum delineates the phenotypic, aetiologic, and preparatory domains requisite for effective clinical navigation of the disorder.
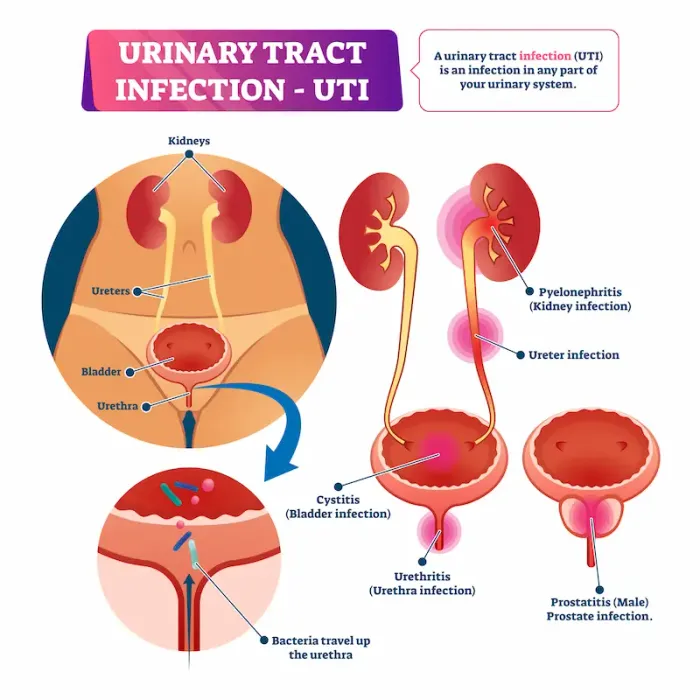
Definition of a Urinary Tract Infection
A urinary tract infection comprises a pathogenic event involving contiguous urinary system components. In clinical practice, the focus is often the lower urinary tract, encompassing the bladder and urethra, owing to the demographic predisposition of the female sex.
UTI Subtypes
1. Cystitis: Infection is localized to bladder mucosa; presentations include suprapubic discomfort and altered voiding patterns.
2. Urethritis: Infection of the urethral epithelium presents with characteristic burning during voiding and frequency.
3. Pyelonephritis: Ascending infections involve renal parenchyma; symptomology includes systemic febrile response and unilateral flank pain.
Characteristic Manifestations of Urinary Tract Infection
Although the presence of a urinary tract infection (UTI) does not guarantee observable clinical manifestations, the most widespread signs consist of the following:
1. Dysuria, frequently described as a sharp, burning discomfort accompanying micturition
2. Urgency, frequently registered as a persistent need to void, resulting in scant urine output
3. Urine exhibiting turbidity, a darker hue, or an unusually pungent odor
4. Lower abdominal discomfort, reported most frequently in the female population
5. Hematuria, which appears in a subset of cases
When the pathological process ascends to the renal pelvicalyceal system, the following systemic presentations may be noted:
1. Pyrexia, commonly accompanied by rigor
2. Flank or costovertebral angle tenderness
3. Gastrointestinal disturbance manifested by nausea or emesis
Patients exhibiting any of the latter features are strongly advised to obtain prompt medical evaluation to avert potential complications.
What Causes UTIs?
A urinary tract infection is initiated when opportunistic bacteria, predominantly uropathogenic E. coli, colonize the urinary tract. Common contributing mechanisms encompass the following:
1. Inadequate perineal hygiene, where retrograde wiping facilitates fecal flora translocation to the urethra
2. Extended urinary retention, which permits unattended bacteria to proliferate
3. Coital activity, functioning as a vector for external flora invasion
4. Postmenopausal estrogen decline, which compromises uroepithelial defense
5. Anatomical obstruction, e.g., urethral stricture, calcium crystals, or benign prostatic hypertrophy
6. Immunosenescence or comorbid syndromes, such as diabetes, which reduce host resistance
Who is at Higher Risk?
Individual susceptibility is expedited in the following populations:
1. Females, given the shorter urethral transit distance
2. Sexually active persons, particularly with frequent or aggressive intercourse
3. Diabetic individuals, where glycosuria supersedes host defense
4. Geriatric cohorts, in whom comorbidities and atrophic urethra converge
5. Those requiring prolonged or intermittent urinary catheters, which breach mucosal barriers
6. Males with hypertrophic prostate tissue, impeding full bladder drainage
How to Prevent UTIs
Prophylactic measures are often more efficacious than curative protocols. Evidence-based recommendations for reducing infection incidence are:
1. Ingest copious liquids, enhancing renal flow and micturitional washing
2. Maintain scheduled micturition, avoiding pathological retention
3. Adopt a front to back wiping directive to curtail urethral contamination
4. Void postintercourse, a bidirectional clearing strategy against coital contamination
5. Choose unscented feminine products: Scented sprays or douches can destabilize the vaginal flora, allowing pathogens to multiply.
6. Opt for breathable fabrics: Cotton promotes airflow and diminishes moisture accumulation that encourages bacterial colonization.
Dietary Interventions
Consume unsweetened cranberry beverages or standardized capsules to inhibit bacterial adhesion to the uroepithelium.
Incorporate probiotics, particularly Lactobacillus species, to reinforce urogenital microbiota.
Reduce intake of caffeinated and alcoholic beverages, both of which can provoke bladder irritation.
Indications for Clinical Evaluation
Although uncomplicated cystitis may remit spontaneously, evaluation is warranted under the following circumstances:
Dysuria and frequency persist for 4872 hours
Accompanying systemic signs (fever greater than 100°F, rigors, or flank pain) suggest pyelonephritis
Hematuria is present
The patient experiences three or more episodes annually
Apollo 24|7 Support
Patients suspecting a urinary tract infection can access:
• Virtual physician consultations—Receive urological evaluation and treatment recommendations from home.
• Laboratory diagnostics—Rapid, accurate urine microscopy and culture.
• Pharmacologic therapy—Antimicrobial regimens shipped to the patient’s registered address.
• Schedule a consultation or laboratory evaluation to obtain expedient management.
Management Protocol
Uncomplicated urinary tract infections are usually eradicated with a full course of the appropriate oral antibiotic. Adhere to the directed treatment duration to mitigate recurrence and resistance.
For symptomatic relief of pain:
• Increase oral fluid intake.
• Apply a heated pad to the pelvis or lower abdomen.
• Administer available analgesics such as acetaminophen.
Conclusion
Urinary tract infections cause significant discomfort yet can be effectively treated by adopting targeted preventive measures. Adequate fluid consumption, rigorous personal hygiene, and prompt professional evaluation are essential steps to minimize recurrence and facilitate swift recovery.
Persistent or worsening symptoms should prompt immediate assessment to avert potential sequelae.
Protect your wellbeing. Contact Apollo 24|7 for expert guidance.




