Varicose Veins: Causes, Symptoms, and Modern Treatment Options
Discover everything about varicose veins—causes, symptoms, risk factors, and complications. Learn the difference from spider veins, explore modern treatments like laser ablation and sclerotherapy, and find prevention tips for better vascular health.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026
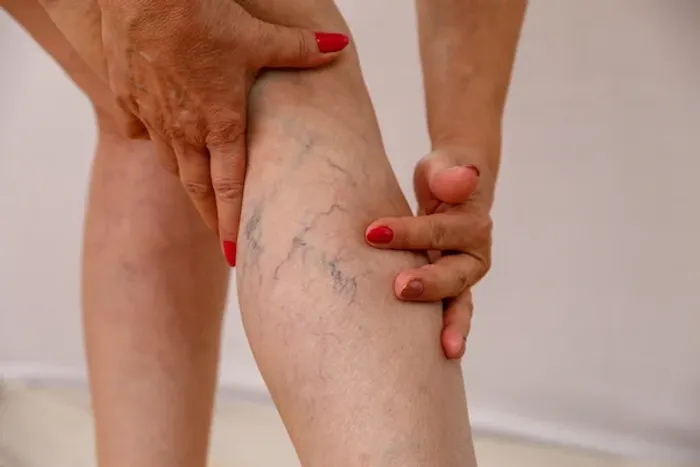
Have you noticed twisted, bulging, blueish-purple veins just under the surface of your skin, particularly on your legs? You’re not alone. Varicose veins are an incredibly common condition, affecting millions of people worldwide. While often dismissed as a mere cosmetic concern, they can sometimes signal underlying circulation issues and cause significant discomfort. This comprehensive guide will walk you through everything you need to know about varicose veins—from what causes them and how to recognize the symptoms, to the latest effective treatment options and preventive measures. Whether you're looking for answers for yourself or a loved one, understanding this condition is the first step toward finding relief and improving your vascular health. Let's unravel the mystery of these prominent veins.
What Are Varicose Veins, Exactly?
Varicose veins are enlarged, swollen, and twisting veins that often appear blue or dark purple. They occur when faulty valves in the veins allow blood to flow backward and pool, causing the veins to stretch and bulge. While they can develop anywhere, they are most commonly found on the legs and feet due to the pressure of standing and walking upright.
The Role of Veins and Valves
To understand varicose veins, it's helpful to know how healthy veins work. Your arteries carry oxygen-rich blood from your heart to the rest of your body. Your veins then have the tough job of carrying deoxygenated blood back to your heart against gravity. Tiny one-way valves inside your veins open to let blood through and then snap shut to prevent it from flowing backward. When these valves weaken or become damaged, blood can leak backward and collect in the vein, creating the characteristic appearance of varicose veins. This entire process is known as venous insufficiency.
Varicose Veins vs. Spider Veins: Knowing the Difference
It's easy to confuse the two, but they are different. Spider veins are smaller, finer, red or blue vessels that are closer to the skin's surface. They look like a spiderweb or tree branches and are primarily a cosmetic issue. Varicose veins are larger, deeper, and more likely to cause pain and other symptoms. Think of spider veins as a precursor; they can sometimes indicate a higher risk for developing varicose veins.
What Causes Varicose Veins to Develop?
The primary culprit behind varicose veins is weakened or damaged valves, leading to venous insufficiency. But what causes this damage in the first place? A combination of factors is usually at play.
Faulty Valves and Venous Insufficiency
As we age, veins can lose elasticity, causing them to stretch. The valves within them may become weak, allowing blood that should be moving toward your heart to flow backward. This backflow pools in the vein, causing it to stretch and twist, further weakening the valve—a vicious cycle that defines venous insufficiency.
Key Risk Factors You Should Know
Several factors increase your pressure on your leg veins or your likelihood of developing valve problems:
Age: The natural wear and tear of aging makes valve weakening more common.
Sex: Women are more likely to develop the condition, often due to hormonal changes during pregnancy, pre-menstruation, or menopause.
Pregnancy: Blood volume increases during pregnancy to support the growing fetus, but this can also enlarge veins in your legs.
Family History: If other family members had varicose veins, your risk is higher.
Obesity: Excess weight puts additional pressure on your veins.
Prolonged Standing or Sitting: Jobs that require long periods in one position make it harder for blood to flow against gravity.
Recognizing the Symptoms: More Than Just a Cosmetic Issue
While the bulging, rope-like appearance is the most recognizable sign, the symptoms of varicose veins can extend far beyond aesthetics.
Common Physical Sensations
Many people experience:
An aching or heavy feeling in the legs.
Burning, throbbing, or muscle cramping in the lower legs.
Worsened pain after sitting or standing for a long time.
Itching around one or more of your veins.
Swelling in the feet and ankles.
Signs of a More Serious Problem
In some cases, complications can arise. Be aware of:
Skin discoloration or inflammation around the vein.
Bleeding from the vein.
The sudden development of a painful, hard, cord-like vein accompanied by redness—this could signal a blood clot (thrombophlebitis).
Venous ulcers, especially near the ankle, indicating severe vascular disease.
If you experience persistent pain, significant swelling, or skin changes, it's crucial to seek professional advice. If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation.
How Are Varicose Veins Diagnosed?
Diagnosing varicose veins is typically straightforward. A doctor will first conduct a physical examination, looking at your legs while you're standing to check for swelling.
The Physical Examination
Your doctor will observe the visible veins and may ask you to describe any pain or achiness. They might also recommend tests to get a clearer picture of the blood flow.
The Duplex Ultrasound Scan
This is the gold standard for diagnosis. A duplex ultrasound is a non-invasive test that uses high-frequency sound waves to create detailed images of your veins. It allows the doctor to see the structure of your veins, check the functionality of the valves, and detect any evidence of a blood clot. This painless procedure is crucial for planning the most effective treatment for varicose veins.
Effective Treatment Options for Varicose Veins
Thankfully, you don't have to live with the discomfort. A range of treatments exists, from simple self-care to advanced medical procedures.
Lifestyle and Home Remedies
For mild cases, these measures can reduce pain and prevent worsening:
Exercise: Walking improves calf muscle strength and circulation.
Weight Management: Shedding excess pounds reduces pressure on veins.
Elevation: Raising your legs above heart level for 15 minutes several times a day helps drainage.
Avoiding prolonged sitting/standing: Shift your weight and take short walking breaks.
Compression Stockings
Often the first line of defense, these specially designed stockings apply steady pressure to your legs, helping veins and leg muscles move blood more efficiently. They come in various strengths and styles.
Minimally Invasive Procedures
When conservative measures aren't enough, several effective outpatient procedures are available:
Sclerotherapy: A solution is injected into the vein, causing it to scar and collapse, forcing blood into healthier veins.
Laser Ablation (EVLA): Laser energy is delivered through a thin fiber inserted into the vein, heating and sealing it shut.
Radiofrequency Ablation (RFA): Similar to laser treatment, but uses radiofrequency energy to heat and close the vein.
Surgical Options
For very large, severe veins, surgery might be recommended:
Ligation and Stripping: The problematic vein is tied off (ligation) and removed (stripping) through small incisions. This is less common now due to the success of less invasive methods.
If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 to discuss which medical procedure might be right for you.
Can You Prevent Varicose Veins?
There's no guaranteed way to prevent them, but you can improve circulation and muscle tone to reduce your risk:
Exercise regularly.
Maintain a healthy weight.
Eat a high-fiber, low-salt diet.
Avoid high heels and tight hosiery.
Elevate your legs.
Change your sitting or standing position frequently.
Potential Complications of Untreated Varicose Veins
While often manageable, leaving severe varicose veins untreated can sometimes lead to:
Ulcers: Painful ulcers can form on the skin near the ankle.
Blood Clots: Occasionally, deep veins within the legs become enlarged and might cause pain and swelling (DVT).
Bleeding: The veins close to the skin can burst, causing minor bleeding that requires medical attention.
Conclusion
Varicose veins are a widespread condition rooted in faulty valves that cause blood to pool in the veins. While they can be unsightly, they often present real physical symptoms like aching, heaviness, and swelling. Understanding the causes of bulging veins and recognizing the symptoms is key to seeking timely intervention. The good news is that a spectrum of highly effective treatments exists, from lifestyle adjustments and compression wear to quick, minimally invasive procedures that offer significant relief. Remember, vascular health is a crucial part of your overall well-being. Don’t dismiss persistent leg pain as a normal part of aging. Take proactive steps, listen to your body, and consult a healthcare professional to explore your options for healthier, more comfortable legs.
More articles from Varicose Veins
Frequently Asked Questions
Q1. Can varicose veins go away on their own?
No, once they develop, varicose veins will not disappear without treatment. However, symptoms can be managed with lifestyle changes, and their appearance can be significantly reduced with medical procedures
Q2. Are varicose veins dangerous?
For most people, they are not dangerous but can be uncomfortable. In rare cases, they can lead to more serious complications like blood clots (DVT) or ulcers, which is why evaluation by a doctor is important.
Q3. What is the best treatment for varicose veins?
There is no single 'best' treatment. The right option depends on the size, location, and severity of your veins, as well as your overall health. A vascular specialist can recommend the most appropriate procedure, such as sclerotherapy for smaller veins or endovenous laser treatment for larger ones.
Q4. Can I exercise if I have varicose veins?
Yes, exercise is highly encouraged! Activities like walking, swimming, and cycling improve circulation and strengthen calf muscles, which act as a pump to help move blood back to the heart. Avoid exercises that put excessive strain on your veins, like heavy weightlifting.
Q5. Do varicose veins come back after treatment?
Treating a varicose vein successfully removes or destroys it, and that specific vein will not return. However, the underlying tendency for venous insufficiency remains, so it is possible for new varicose veins to develop over time.

