Glucose Challenge Test Understanding Normal Values and Results
Learn the normal values for the glucose challenge test, how it screens for gestational diabetes, and what your results indicate for your health.

Introduction
If you’ve been told it’s time for your glucose challenge test, you might be wondering what’s “normal,” how to prepare, and what your numbers really mean. The glucose challenge test is a quick, non-fasting screening that checks how your body handles sugar during pregnancy. It’s an important step in identifying gestational diabetes early—so you and your baby get the right care at the right time. In this guide, we’ll walk through the test, normal glucose values, why thresholds sometimes differ between clinics, what happens next if your result is high, and how to lower your risk safely. You’ll also see clear explanations, helpful examples, and a visual roadmap of the testing pathway. Whether you’re preparing for your first test, reviewing a lab report, or supporting a loved one, this guide aims to make everything simple, evidence-based, and actionable.
What is the Glucose Challenge Test (GCT)?
The glucose challenge test is a screening test used during pregnancy to identify people who may have gestational diabetes (GDM). It’s typically a 50-gram, non-fasting test: you drink a sugary solution, wait one hour, and then have your blood glucose checked. The goal isn’t to diagnose diabetes on the spot but to flag who needs a follow-up diagnostic test.
• Non-fasting: Unlike many glucose tests, you don’t need to fast for the 1-hour GCT. This makes it convenient and widely usable during routine antenatal visits.
• Quick workflow: Drink the 50 g glucose solution, wait 60 minutes without eating or drinking anything else, then a single blood sample is drawn.
• Screening, not diagnosis: If your glucose is high at 1 hour, you’ll be referred for a longer oral glucose tolerance test (OGTT) to confirm or rule out GDM.
One-step vs two-step screening
• Two-step (common in the U.S.): Step 1 is the 50 g, 1-hour GCT (non-fasting). If the screen is positive, Step 2 is a 3-hour 100 g OGTT with fasting.
• One-step (common in many countries): A single 75 g OGTT performed fasting, with blood draws at fasting, 1 hour, and 2 hours. Any one abnormal value can diagnose GDM.
Consult Top Specialists
Why this Test Matters: Screening for Gestational Diabetes?
Gestational diabetes can be silent. You may feel completely fine yet have elevated glucose that increases risks for both you and your baby. Screening at the right time helps catch issues early, so timely lifestyle changes or medication can lower risks.
• Maternal risks of untreated GDM include preeclampsia, cesarean delivery, and progression to type 2 diabetes later in life.
• Fetal risks include macrosomia (a larger baby), shoulder dystocia during delivery, neonatal hypoglycemia, and jaundice. Proper management lowers these risks substantially.
• Evidence-backed benefits: Treating GDM reduces rates of large-for-gestational-age infants and preeclampsia, and decreases the need for cesarean section. The earlier GDM is identified and managed, the better the outcomes.
Risks of untreated GDM (at a glance)
• For the parent: hypertensive disorders, delivery complications, higher lifetime risk of type 2 diabetes.
• For the baby: high birth weight, complicated delivery, low blood sugar after birth, and later-life metabolic risks.
When to take the test—and who needs it earlier?
Most people are screened between 24 and 28 weeks of pregnancy. Why that window? Insulin resistance typically rises as pregnancy progresses, so this timing captures those changes while allowing enough time to intervene before birth.
Early screening if you’re high risk
You may be offered early testing (first prenatal visit or early second trimester) if you have:
• Obesity (BMI ≥ 30)
• A previous pregnancy with GDM or a history of a large baby (macrosomia)
• Polycystic ovary syndrome (PCOS)
• A first-degree relative with diabetes
• Prediabetes or elevated fasting glucose before pregnancy
• Certain ethnic backgrounds with higher GDM prevalence
What early screening looks like
Your clinician may order fasting plasma glucose, HbA1c, or even an early OGTT. If early tests are normal, you’ll usually repeat the standard GCT at 24–28 weeks because glucose metabolism changes as pregnancy advances. If symptoms persist beyond two weeks (e.g., excessive thirst, fatigue), consult a doctor online with Apollo24|7 for further evaluation and guidance.
How to prepare and what to expect on test day?
The 1-hour glucose challenge test is designed to be user-friendly. Here’s how to rpepare for it:
• No fasting required: You can eat normally. Most clinics recommend avoiding a very sugary meal or drink immediately before the test, which could artificially elevate your reading.
• The drink: You’ll receive a 50 g glucose solution (often called “glucola”) to consume within 5 minutes. It’s sweet, sometimes flavoured (orange, lemon-lime).
• The wait: Stay seated and do not eat, drink, or smoke for 60 minutes. Vigorous activity can lower glucose levels, potentially causing an inaccurate “normal” result. Keep activity light and consistent.
• The draw: A single blood sample is taken exactly 60 minutes after finishing the drink. Try to arrive a few minutes early and time your drink carefully per staff instructions.
Side effects and simple tips
• Common: Nausea, a brief “sugar rush,” lightheadedness. Eating protein and fiber earlier in the day (hours before your appointment) can help you feel steadier—but don’t eat right before you drink.
• If you vomit: Tell the staff. You may need to reschedule the test.
• Medications: Steroids can raise glucose; ask your clinician if any current medicines could affect results.
Normal glucose values for the 1-hour test—and why thresholds differ
What’s a normal result for the 1-hour, 50 g glucose challenge test? Most clinics consider a result below 140 mg/dL (7.8 mmol/L) as normal. However, some use 135 mg/dL or even 130 mg/dL as the cutoff to “flag” the test as positive, especially in higher-risk populations.
Common cutoffs you might see
• Less than 140 mg/dL: Often considered normal.
• 130–139 mg/dL: Normal in many clinics, but some use 130 or 135 mg/dL as a stricter cutoff for a positive screen to capture more cases.
• 140 mg/dL or higher: Usually triggers a diagnostic OGTT.
• High values (e.g., ≥ 190 mg/dL): Some clinics consider this sufficient to diagnose GDM without a confirmatory OGTT; others still require the 3-hour test. Policies vary.
Check Your Glucose Levels Here
Why the cutoffs vary (sensitivity vs specificity)
• 130 mg/dL maximises sensitivity (fewer missed cases) but increases false positives (more people sent for OGTT who don’t have GDM).
• 140 mg/dL improves specificity (fewer OGTTs for people who are actually normal) but can miss some milder cases.
ACOG and ADA acknowledge this variability and allow clinics to choose within 130–140 mg/dL based on local prevalence and resource considerations.
Real-world example
In a population with higher baseline GDM risk (e.g., more people with obesity or prior GDM), a clinic may choose 135 mg/dL to catch more at-risk pregnancies earlier, accepting that more OGTTs will follow.
What to do if your Result is High?
A positive screen on the 1-hour test doesn’t mean you have GDM; it means you need the diagnostic OGTT:
• The 3-hour, 100 g OGTT (two-step approach): You fast overnight. Blood is drawn at fasting, then at 1, 2, and 3 hours after drinking a 100 g glucose solution. Diagnosis typically requires two or more values at or above specific cutoffs.
Common diagnostic cutoffs (Carpenter–Coustan):
• Fasting ≥ 95 mg/dL
• 1 hour ≥ 180 mg/dL
2 hours ≥ 155 mg/dL
• 3 hours ≥ 140 mg/dL
Alternative criteria (NDDG) use slightly higher thresholds. Your lab report should note which criteria are used.
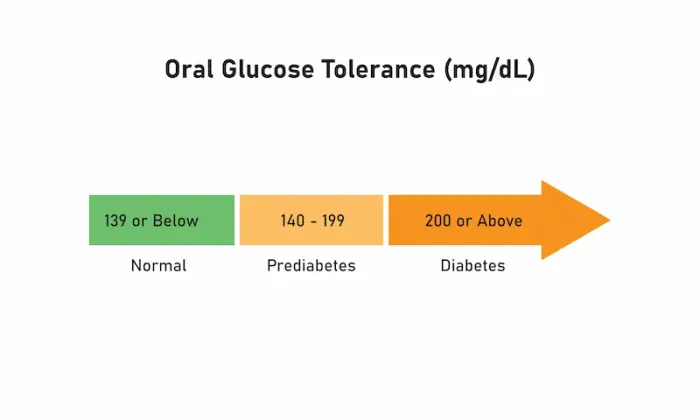
One-step alternative: the 75 g, 2-hour OGTT
Some regions use the one-step method:
• Fasting ≥ 92 mg/dL
1 hour ≥ 180 mg/dL
• 2 hours ≥ 153 mg/dL
One or more abnormal values can diagnose GDM. [2,5]
What can skew results?
Several factors can nudge your 1-hour glucose higher or lower:
• Medications: Systemic corticosteroids and beta-agonists can raise glucose. Discuss your medication list beforehand.
• Timing of meals: While it’s a non-fasting test, a very sugary meal just before can push your glucose up. Eat normally and avoid a heavy sugar load right before the appointment.
• Physical activity: Vigorous exercise shortly before or during the waiting period can lower glucose and potentially mask issues. Keep activity level consistent and moderate.
• Sleep and stress: Sleep deprivation and acute stress can transiently elevate glucose.
• Acute illness: Infections can raise glucose; consider rescheduling if you’re sick.
• Lab handling: Blood processed promptly in fluoride/oxalate tubes avoids glycolysis-related drops in glucose; reputable labs follow this, but delays can artifactually lower readings. [2–4]
What about anaemia or iron supplements?
• Iron deficiency can affect HbA1c interpretation, but it has minimal direct impact on the 1-hour GCT. Still, severe anaemia or dehydration can influence lab values; let your clinician know if you have known hematologic issues.
GCT vs OGTT: Key Differences you Should Know
• Purpose: GCT is a screening test; OGTT is diagnostic.
• Fasting: GCT is non-fasting; OGTT requires fasting.
• Time: GCT takes about 1 hour plus setup; OGTT requires 2–3 hours of timed blood draws.
• Interpretation: GCT has a single cutoff (e.g., 130–140 mg/dL). OGTT has multiple time-point thresholds; meeting specific criteria confirms GDM. [2–4]
Safe Ways to Lower Risk Before and After the Test
You can’t “study for” the test, and trying to game it (e.g., crash dieting or extreme exercising) could miss a diagnosis that matters for your health. Instead, focus on sustainable habits:
• Balanced meals: Pair carbohydrates with protein, healthy fats, and fibre (e.g., whole grains + eggs + avocado) to moderate glucose spikes.
• Regular movement: Aim for light-to-moderate physical activity most days (e.g., 20–30 minutes of walking), unless advised otherwise by your obstetrician.
• Sleep: 7–9 hours supports better glucose control.
• Hydration: Proper hydration helps overall well-being and lab accuracy.
These changes help even if you ultimately need medication; many with GDM manage well with diet and activity alone.
What to Expect If GDM is Diagnosed?
A diagnosis is not a failure—it’s a roadmap. With guidance, most pregnancies with GDM end with healthy outcomes.
• Monitoring: You’ll likely check glucose at home (fasting and post-meal targets set by your clinician).
• Nutrition counselling: A registered dietitian can tailor a plan that supports both you and your baby.
• Medications: If glucose targets aren’t met with lifestyle changes, insulin is first-line; some clinicians use metformin in specific cases. Treatment reduces complications.
• Delivery planning: Your team may adjust your monitoring late in pregnancy and discuss timing of delivery based on glucose control and fetal growth.
If you need help getting started, consult a doctor online with Apollo24|7 to review your results and plan next steps.
Postpartum follow-up and long-term health
After delivery, glucose usually improves—but your long-term health still matters.
• 4–12 weeks postpartum: ADA recommends a 75 g, 2-hour OGTT to check for persistent glucose issues.
• Long-term: If normal postpartum, screen for diabetes every 1–3 years (fasting glucose, HbA1c, or OGTT as advised).
• Lifestyle: Continuing balanced meals, activity, and sleep helps reduce future risk of type 2 diabetes. Breastfeeding, when possible, may also have metabolic benefits.
Why follow-up is crucial?
Up to half of people with prior GDM develop type 2 diabetes over the next 10–20 years. Early detection lets you intervene sooner. Apollo 24|7 offers convenient home collection for routine labs like fasting glucose and HbA1c; ask your clinician which test is right for you at each interval.
Access, costs, and practical options
• Where the test happens: Most GCTs and OGTTs are performed in clinics or hospital labs due to strict timing and handling requirements.
• Insurance and costs: Coverage is common as part of prenatal care; out-of-pocket costs vary. Ask your clinic and insurer ahead of time.
• Alternatives to the drink: Some centers allow validated alternatives (e.g., specific jelly bean protocols) if you cannot tolerate the standard solution—availability varies by clinic.
Safety, myths, and what not to do
• Myth: “I should cut carbs drastically right before the test to pass.” Reality: You might mask an issue, increasing risks later. Eat normally.
• Myth: “The drink is dangerous.” Reality: It’s safe for most; side effects like nausea are usually brief. If you have a specific intolerance, discuss options.
• Myth: “A borderline high result means I have diabetes.” Reality: It means you need the OGTT to know for sure.Consult Top Specialists
Conclusion
The glucose challenge test is a simple, valuable part of prenatal care. Understanding what’s normal, why your clinic’s cutoff might differ from a friend’s, and what happens after a positive screen can remove a lot of the mystery—and stress. If your 1-hour result is below your clinic’s cutoff (often 140 mg/dL), you likely don’t need more testing. If it’s at or above the cutoff, the confirmatory OGTT gives a definitive answer. Either way, you’re taking the right steps to protect your health and your baby’s. Should you need support interpreting results, or if symptoms such as excessive thirst, fatigue, or frequent urination persist, consult a doctor online with Apollo 24|7 for timely advice. And remember: a diagnosis of gestational diabetes is a starting point, not an endpoint. With a personalised plan—nutrition, activity, monitoring, and medications if needed—most people achieve healthy outcomes. Don’t forget postpartum follow-up at 4–12 weeks and regular screening thereafter; it’s your best long-term safeguard.
Consult Top Specialists

Dr. Vasanthasree Nair
General Practitioner
15 Years • MBBS
Angamaly
Apollo 24|7 Clinic - Kerala, Angamaly
(525+ Patients)

Dr. Jawwad Mohammed Kaleem
General Practitioner
4 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Shaik Abdul Kalam
General Practitioner
3 Years • MD (Physician)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam
(175+ Patients)

Dr. Mohammed Kamran
General Practitioner
5 Years • MBBS, FIDM
Nashik
Apollo 24|7 Clinic - Maharashtra, Nashik

Dr. Hrishikesh Shivakumar
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (GENERAL MEDICINE)
Bangalore
Apollo 24|7 Clinic - Karnataka, Bangalore
(75+ Patients)
Consult Top Specialists

Dr. Vasanthasree Nair
General Practitioner
15 Years • MBBS
Angamaly
Apollo 24|7 Clinic - Kerala, Angamaly
(525+ Patients)

Dr. Jawwad Mohammed Kaleem
General Practitioner
4 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Shaik Abdul Kalam
General Practitioner
3 Years • MD (Physician)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam
(175+ Patients)

Dr. Mohammed Kamran
General Practitioner
5 Years • MBBS, FIDM
Nashik
Apollo 24|7 Clinic - Maharashtra, Nashik

Dr. Hrishikesh Shivakumar
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (GENERAL MEDICINE)
Bangalore
Apollo 24|7 Clinic - Karnataka, Bangalore
(75+ Patients)
Frequently Asked Questions
1) Do I need to fast for the 1-hour glucose challenge test?
No. It’s a non-fasting test. Eat normally but avoid a very sugary meal or drink right before to keep results accurate. This is a screening test for gestational diabetes.
2) What is a normal glucose value for the 1-hour test?
Many clinics use under 140 mg/dL as normal. Some use 130–135 mg/dL to increase sensitivity. Ask your clinic which cutoff they use.
3) I “failed” the 1-hour test but “passed” the 3-hour OGTT. What now?
You do not have GDM by standard criteria, but you may still have a slightly higher risk later. Keep healthy habits and attend all prenatal visits.
4) Can I avoid the glucose drink?
Some centers offer validated alternatives (such as specific jelly bean protocols), but this varies. If you have intolerance or prior bariatric surgery, ask about options or a direct OGTT.
5) How can I safely prepare for better results?
Focus on balanced meals, regular light-to-moderate activity, good sleep, and staying hydrated. Don’t crash diet or over-exercise to “pass” the test; accurate results are safest for you and your baby.

.webp)