Prostate Cancer Screening A Clear Guide to the PSA Test
Understand prostate cancer screening with our clear guide to the PSA test—learn who should get tested, how it works, and how to interpret results for informed prostate health decisions.

Written by Dr. Md Yusuf Shareef
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 26th Sep, 2025
Introduction: Navigating the Decision for Prostate Health
For men concerned about their long-term health, the topic of prostate cancer screening often brings up a mix of confusion and anxiety. You may have heard about the PSA test, but aren't sure what it involves, who it's for, or what the results truly mean. You're not alone. Prostate cancer is one of the most common cancers among men, but the decision to get screened is highly personal and should be an informed one. This guide is designed to cut through the complexity and provide you with a clear, comprehensive understanding of prostate cancer and the role of the PSA test. We will walk you through what the test measures, the current screening guidelines, how to interpret results, and the critical discussion around the benefits and potential risks. Our goal is to empower you with the knowledge you need to have a productive conversation with your healthcare provider about your prostate health. Think of this as your roadmap to making a confident, informed decision.
What is Prostate Cancer?
Prostate cancer begins when cells in the prostate gland start to grow out of control. The prostate is a small, walnut-shaped gland that is part of the male reproductive system, producing fluid that nourishes and transports sperm. It's important to know that many prostate cancers grow slowly and may not cause significant harm, especially in older men. However, some types are aggressive and can spread quickly if not detected and treated early.
The Role of the Prostate Gland
Located just below the bladder and in front of the rectum, the prostate gland surrounds the urethra—the tube through which urine passes out of the body. Its primary function is to produce prostatic fluid, a key component of semen. Because of its location, prostate issues, whether cancer or a benign condition like an enlarged prostate, can often affect urinary function.
Consult a Urologist for the best advice
Understanding the PSA Test: Your First Line of Defense
The prostate-specific antigen (PSA) test is a simple blood test that has revolutionised the detection of prostate cancer. It measures the level of PSA, a protein produced by both cancerous and noncancerous tissue in the prostate, in your bloodstream. It's not a test for cancer itself, but rather an indicator that something may be affecting the prostate.
What Does a PSA Test Actually Measure?
PSA is normally present in the blood in small quantities. When the prostate is disturbed—whether by cancer, infection (prostatitis), enlargement (benign prostatic hyperplasia or BPH), or even vigorous exercise—it can release more PSA into the bloodstream, causing the level to rise. Therefore, an elevated PSA level is a signal that warrants further investigation, not a definitive cancer diagnosis.
What is a Normal PSA Level?
There is no single "normal" PSA level for all men. Traditionally, a level below 4.0 nanograms per milliliter (ng/mL) was considered normal. However, this is a guideline, not a strict rule.
Understanding your PSA results requires context:
• Age: PSA levels naturally increase as a man ages. A PSA of 3.5 might be normal for a 70-year-old but cause for concern in a 50-year-old.
• Baseline: Your doctor is often more interested in how your PSA level changes over time (PSA velocity) than in a single reading.
Who Should Get Screened for Prostate Cancer?
The decision to get screened is not one-size-fits-all. Major medical organisations emphasise shared decision-making—a conversation between you and your doctor about the potential benefits and risks based on your individual situation.
General Age Guidelines and Risk Factors
• Average Risk: For men at average risk, discussions about screening often begin at age 50.
• Higher Risk: For men with a higher risk, such as those with a family history (a father or brother diagnosed with prostate cancer), discussions should start earlier, at age 40 or 45.
• Highest Risk: African American men and those with known BRCA1 or BRCA2 gene mutations have the highest risk and should also begin the conversation earlier.
High-Risk Groups: When to Start Sooner
If you fall into a high-risk category, being proactive is key. Early prostate cancer screening can be life-saving. It's crucial to discuss your personal and family medical history openly with your doctor to determine the best timeline for you.
The PSA Test Procedure: What to Expect
The PSA test is straightforward and low-risk, involving a simple blood draw.
Before the Test: Simple Preparation
Very little preparation is needed. However, you should inform your doctor about any recent medical procedures, like a cystoscopy, or infections, as these can temporarily elevate PSA. Some doctors may advise avoiding ejaculation for 24-48 hours before the test.
During and After the Blood Draw
A healthcare professional will draw a small sample of blood from a vein in your arm. The process takes only a few minutes. You can resume your normal activities immediately afterward. The sample is sent to a lab for analysis, and your doctor will discuss the results with you once they are available. For convenience, services like Apollo24|7 offer home collection for tests like the PSA, making the process even easier.
Interpreting Your PSA Results: It's Not Just a Number
A single PSA number is just one piece of the puzzle. Doctors look at several factors to understand what your level means.
Factors That Can Affect PSA Levels
Many non-cancerous conditions can cause an elevated PSA. These include:
• Benign Prostatic Hyperplasia (BPH): A common, non-cancerous enlargement of the prostate in older men.
• Prostatitis: An inflammation or infection of the prostate gland.
• Urinary Tract Infection (UTI)
• Recent Medical Procedures: Anything that manipulates the prostate, like a catheter or biopsy.
• Vigorous Exercise: Such as long-distance cycling, shortly before the test.
PSA Velocity and Density: A Deeper Look
Here’s what each means:
• PSA Velocity: This refers to how quickly your PSA level rises over time. A rapid increase may be more concerning than a stable, slightly elevated level.
• PSA Density: This calculation compares your PSA level to the size of your prostate (measured via an ultrasound or MRI). A high PSA in a small prostate may be more suspicious than the same PSA in a very large prostate.
The Great Debate: Weighing the Benefits and Risks of PSA Screening
This is the most critical part of the screening discussion. Understanding both sides is essential for making an informed choice.
The Benefit: Early Detection Saves Lives
The primary benefit of the PSA test is clear: it can find prostate cancer at an early, treatable stage, often before symptoms appear. This early detection has been shown to reduce the risk of the cancer spreading and to lower the death rate from prostate cancer.
The Risks: Understanding Overdiagnosis and Overtreatment
This is the core of the debate. The test can detect slow-growing cancers that would never have caused symptoms or harm during a man's lifetime. This is called overdiagnosis. The problem is that once cancer is detected, it often leads to overtreatment—aggressive therapies like surgery or radiation that can have significant side effects like erectile dysfunction and urinary incontinence, all for a cancer that didn't need treatment. This is why "active surveillance" (monitoring low-risk cancer instead of immediately treating it) has become a common and important management strategy.
If Your PSA is High: The Next Steps in Diagnosis
A high PSA does not mean you have cancer. It means more information is needed.
The Digital Rectal Exam (DRE)
Your doctor may perform a DRE to feel the prostate for any lumps, hardness, or asymmetry. The DRE and PSA test together provide a better picture than either test alone.
The Prostate Biopsy: Getting a Definitive Answer
If results are suspicious, the next step is usually a biopsy. A urologist uses a thin needle to take small tissue samples from the prostate, which are then examined under a microscope for cancer cells. If cancer is found, it is assigned a Gleason score that indicates how aggressive it is. If your symptoms or test results are concerning, it's crucial to consult a specialist. You can book a physical visit to a urologist with Apollo24|7 for a comprehensive evaluation.
Get Your Health Assessed
Beyond the Standard PSA: Newer, Smarter Tests
To help address the limitations of the standard PSA test, several newer tests provide more refined information.
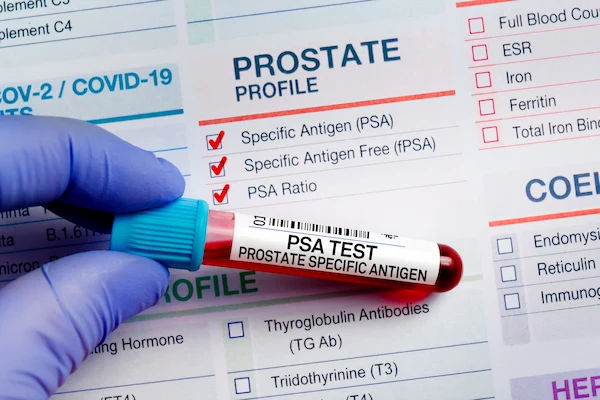
The Free PSA Test
This test measures the ratio of "free" PSA (not attached to proteins in the blood) to total PSA. A lower percentage of free PSA is associated with a higher likelihood of cancer. This can help doctors decide if a biopsy is necessary when total PSA levels are in a borderline range.
The 4Kscore Test and PHI Test
These are more advanced blood tests that combine PSA with other biomarkers to better predict the risk of finding an aggressive prostate cancer on a biopsy. They are valuable tools for helping men and their doctors decide on the best course of action after an elevated PSA.
Conclusion: An Informed Decision is the Best Decision
Navigating the world of prostate cancer screening can feel complex, but knowledge is your most powerful tool. The PSA test remains a key part of men's health, offering the potential for life-saving early detection. However, it is crucial to approach it with a clear understanding of both its strengths and its limitations. The goal is not simply to get tested, but to engage in a thoughtful, informed conversation with your healthcare provider. Discuss your personal risk, the meaning of the results, and the full spectrum of options available, from watchful waiting to active treatment if needed. By taking this proactive and educated approach, you are making the best possible decision for your long-term health and well-being.
Consult a Urologist for the best advice
Consult a Urologist for the best advice

Dr. Sateesh Marriwada
Urologist
17 Years • MBBS, MS (General Surgery), Mch ( Genito Urinary Surgery)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr Tharaka Mourya Nutulapati
Urologist
7 Years • MBBS, MS (General Surgery), Mch ( Urology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Gaurab Dasgupta
Urologist
14 Years • MBBS, MS General Surgery, MCH Urology, FMAS
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Prabir Basu
Urologist
19 Years • MBBS, MS General Surgery, DNB Genito-Urinary Surgery
Jodhpur Park
Dr. Prabir Basu urology clinic, Jodhpur Park
(200+ Patients)

Dr. Barun Kumar
Urologist
12 Years • MBBS MS MCH UROLOGY DNB GENITOURINARY SURGERY
Guwahati
Apollo Clinic Guwahati, Guwahati
Consult a Urologist for the best advice

Dr. Sateesh Marriwada
Urologist
17 Years • MBBS, MS (General Surgery), Mch ( Genito Urinary Surgery)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr Tharaka Mourya Nutulapati
Urologist
7 Years • MBBS, MS (General Surgery), Mch ( Urology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Gaurab Dasgupta
Urologist
14 Years • MBBS, MS General Surgery, MCH Urology, FMAS
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Prabir Basu
Urologist
19 Years • MBBS, MS General Surgery, DNB Genito-Urinary Surgery
Jodhpur Park
Dr. Prabir Basu urology clinic, Jodhpur Park
(200+ Patients)

Dr. Barun Kumar
Urologist
12 Years • MBBS MS MCH UROLOGY DNB GENITOURINARY SURGERY
Guwahati
Apollo Clinic Guwahati, Guwahati
Frequently Asked Questions
1. What is a high PSA level for a 60-year-old man?
While 4.0 ng/mL was once the universal cutoff, age-specific ranges are now often used. For a 60-year-old, a PSA level above 4.0 ng/mL is generally considered elevated and warrants a discussion with a doctor. However, the rate of change (PSA velocity) is equally important.
2. Can I lower my PSA level naturally?
Some lifestyle changes, like maintaining a healthy weight, eating a diet rich in tomatoes (lycopene) and cruciferous vegetables, and reducing red meat intake, may contribute to better prostate health and potentially lower PSA. However, you should never attempt to self-treat a high PSA without consulting a doctor, as this could mask a serious problem.
3. What are the symptoms of an elevated PSA?
The PSA test itself has no symptoms. However, the underlying condition causing the high PSA might. This can include urinary symptoms like frequent urination, weak flow, blood in the urine or semen, or pain in the back, hips, or pelvis. If you experience any of these, it's important to see a doctor.
4. How accurate is the PSA test for detecting cancer?
The PSA test is sensitive but not highly specific. This means it's good at finding something wrong with the prostate but not always good at distinguishing between cancer and benign conditions. This is why a high PSA leads to further tests, not an immediate cancer diagnosis.
5. Does a low PSA level mean I definitely don't have prostate cancer?
While a low PSA level is reassuring, it does not completely rule out prostate cancer. It is possible, though less common, to have prostate cancer with a low PSA level. This is why the combination of PSA, DRE, and other factors is important.