- male
- 60 Years
- 06/03/2021
Can ECG detect heart blockage?
Answered by 1 Apollo Doctors
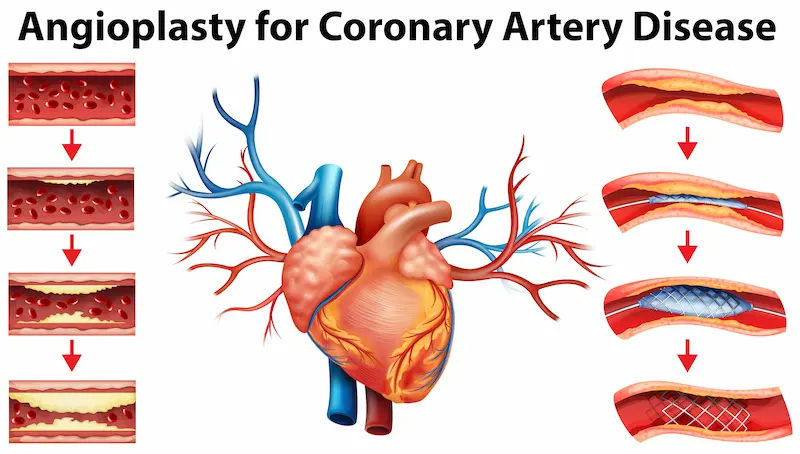
An ECG Can Recognize the Signs of Blocked Arteries. But for further accurecy a CT coronary angiogram can reveal plaque buildup and identify blockages in the arteries, which can lead to a heart attack.
Dr. Anshul Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0


Ask Apollo
AI powered Health Chatbot
-
ECG Utility
An ECG can record the heart's electrical activity and detect some heart issues, but it doesn't directly show artery blockages. -
Detection Limitations
- It may indicate heart muscle damage or reduced blood flow.
- It cannot precisely locate or confirm coronary artery blockages.
-
Further Testing
For detecting blockages, consider tests like: a. Stress test
b. Coronary angiography
c. CT coronary angiogram -
Recommendation
If there are symptoms like chest pain, consult a cardiologist for appropriate tests and treatment. An ECG is a starting point but not definitive for blockages.
Recommended next steps
Consult a Cardiologist or Take a Apollo Stress Impact Management Test
Answered 20/08/2025
1
0
More Cardiology Health Queries
View allI'm a bit worried about my health right now. I've had hypertension for about 9 years and just found out there's an issue with my heart, something about left atrial enlargement. I'm experiencing symptoms like peripheral edema, dizziness, and even feeling faint sometimes. Is this something that can be reversed or might it turn out to be really serious?
Left atrial enlargement is a common complication of long-standing hypertension. While it may not be completely reversible, managing your blood pressure effectively can help prevent further enlargement and reduce the risk of complications. To help manage your symptoms and condition, you can take medications like Losartan 50mg once daily to control your blood pressure and reduce the strain on your heart. Additionally, your doctor may recommend a diuretic like Furosemide 40mg once daily to help with the peripheral edema. It's important to follow your doctor's advice closely and make lifestyle changes such as maintaining a healthy diet, regular exercise, and reducing stress to improve your overall health and prognosis.
Answered by 1 Apollo Doctors
For the past 4 to 5 days, Ive been dealing with an unusually fast heart rate, even when Im just resting. I havent been exercising for a few months now, and I can really feel my heart pounding throughout my body. It gets worse at night and when I checked, my heart rate was 103 bpm, and sometimes its 95 bpm, but it never goes below 90, even when Im just sitting. Im staying hydrated and I dont feel anxious, but Ive started having this chest pain that feels like when someone presses on a bone. What tests should I consider doing to find out whats going on? This fast heart rate is really becoming unbearable. Any advice?
Based on your symptoms of a fast heart rate at rest, palpitations, and chest pain, it is important to consult a healthcare professional for further evaluation. The following tests may be recommended: 1. Electrocardiogram (ECG) to assess the electrical activity of the heart. 2. Holter monitor to continuously record your heart's activity for a period of time. 3. Echocardiogram to evaluate the structure and function of the heart. 4. Blood tests to check for any underlying conditions such as thyroid disorders or electrolyte imbalances. In the meantime, to help manage your symptoms, you can consider taking a beta-blocker medication such as Metoprolol at a starting dose of 25mg once daily, as prescribed by a healthcare professional. Beta-blockers can help lower heart rate and reduce chest pain.
Answered by 1 Apollo Doctors
I'm a bit concerned because I was on medication for blood pressure until November, but stopped after my doctor said my BP levels were normal. It's been fine for the past five months, but now I notice my home readings are at 13898. I've had 500 ml of beer each day for the last two days before this reading. Should I be worried about this change, or is there something I can try before considering going back on medication?
It's important to monitor your blood pressure regularly, especially after noticing an increase like 13898. Since you have a history of high blood pressure and recent alcohol consumption, it's advisable to take action to lower your blood pressure. You can start by making lifestyle changes such as reducing alcohol intake, maintaining a healthy diet low in sodium and high in fruits and vegetables, exercising regularly, and managing stress. Additionally, you can consider taking medication again as prescribed by your doctor to help control your blood pressure. If these measures do not lower your blood pressure, it's essential to consult with your doctor for further evaluation and management.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.