- Male
- 25 Years
- 29/01/2025
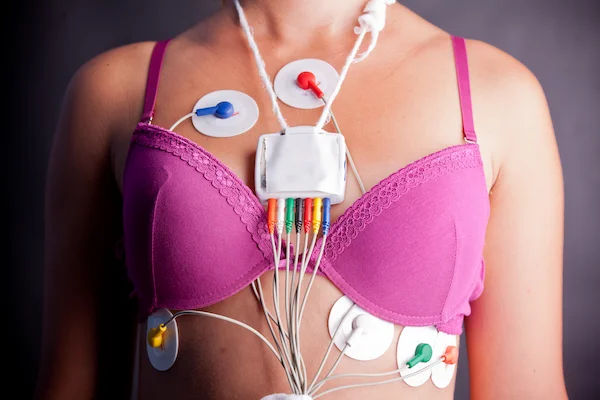
I've been noticing that when I'm lying down, I can hear my heartbeat clearly, and it's even visible through my shirt and in my stomach area. At night, while trying to fall asleep, I sometimes feel a sense of fear in my chest and stomach. What could be causing this?
Answered by 1 Apollo Doctors
These symptoms could be due to anxiety or stress, which can cause palpitations (feeling of heart beating fast or irregularly), visible pulsations in the abdomen, and a sensation of fear or unease in the chest and stomach. It is important to manage stress and anxiety through relaxation techniques, exercise, and possibly counseling. Additionally, you can take a beta-blocker like Propranolol 20mg to help reduce palpitations and visible pulsations. Make sure to consult with a healthcare provider for proper evaluation and management.
Dr. Dr Khaleel Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI've been having this strange sensation on the left side of my chest, kind of like a needle prick. I got an ECG done, and it was normal, which is a relief, but my doctor put me on Provonal Forte. I'm just wondering, could this be some kind of chest infection or maybe anxiety acting up?
The symptoms you are experiencing could be related to anxiety or nerve-related issues. Provanol forte tablet is likely prescribed to help with chest discomfort and anxiety symptoms. However, if you are still feeling needle pricking sensations in your chest, it is important to follow up with your doctor for further evaluation. In the meantime, you can take Paracetamol for pain relief as needed.
Answered by 1 Apollo Doctors
My mom, who's 75, has been having this center chest pain for 25 days now. Last week the doctor gave her met xl 12.5 and veloz d to take every morning after looking at her ECG report, but it hasn't helped with the pain. Today, after checking her 2D echo, they suggested she take Mucaine syrup and Sucrafil three times a day for a month. She's also on telmikind am 80 (half a tablet) and rosuless c 10 every night. I'm really worried since it's been more than a week without improvement. Do you have any idea what might be causing this pain?
Based on the medications your mother is currently taking and the symptoms described, the chest pain could be due to acid reflux or gastroesophageal reflux disease (GERD). The medications prescribed such as Veloz D, Mucaine, and Sucrafil are commonly used to treat symptoms of acid reflux. It is possible that the pain is related to acid irritation in the esophagus. To further alleviate the symptoms, you can consider adding a proton pump inhibitor (PPI) such as Esomeprazole (brand name: Nexium) or Pantoprazole (brand name: Protonix) to reduce stomach acid production. The usual dosage for Esomeprazole is 20-40mg once daily before a meal, and for Pantoprazole, it is 40mg once daily in the morning. Additionally, lifestyle modifications such as avoiding trigger foods, eating smaller meals, avoiding lying down after eating, and maintaining a healthy weight can also help in managing acid reflux symptoms. It is important to continue the current medications as prescribed and follow up with your doctor for further evaluation if the chest pain persists.
Answered by 1 Apollo Doctors
I've been having some strange symptoms lately when I masturbate or watch intimate scenes. My chest gets tight, it feels like there's a lump in my throat, and I have shortness of breath. I sometimes even feel light-headed with my heart racing. I've had heart and lung tests but everything came back normal. Do you have any idea what this might be?
normal
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.