- male
- 60 Years
- 22/01/2025
I'm a bit concerned because my doctor has put me on Lipitas 10 (Rosuvastatin) to take at night, along with Sartel LN (Telmisartan 40) and Cilnidipine. I stumbled across some info that mentioned a serious drug interaction between Cilnidipine and Lipitas. Is that something I should be worried about?
Answered by 1 Apollo Doctors
Prolonged use of clinidipine 10 mg can cause hypotension ,that is a serious side effect. whereas telma causes sinus congestion,tachycardia,changes in vision, large ives and fainting etc.. Both telma and clinidepine are recommended for the control of BP.,You can continue taking the medications..
Dr. Shubham Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI'm 27 and have had no bad habits. For the last eight months, I've been experiencing these quick chest pains on the left side; they just last about 5 to 15 seconds, and they come and go. I've been to the cardiologist and had around 20 ECGs, an echo, and a lipid profile done, and everything came back normal. The thing is, I don't feel any pain during heavy work, just at random times. I'm worried and wondering if this is a heart issue or maybe something physiological? Also, at home, my heart rate is slow, but as soon as I enter the hospital and the tension hits, my heart rate spikes. What could be going on?
It sounds like you may be experiencing episodes of non-cardiac chest pain, especially since your cardiology checkups including ECG, echo, and lipid profile have come back normal. Non-cardiac chest pain can be caused by issues such as muscle strain, anxiety, or gastrointestinal problems. Since your symptoms have been ongoing for eight months and are not related to heavy work, it is less likely to be a heart-related issue. To help with the chest pain, you can try taking over-the-counter pain relievers like acetaminophen. Additionally, practicing relaxation techniques or deep breathing exercises may help with episodes of high heart rate related to tension. If the chest pain persists or worsens, it would be advisable to consult with a doctor for further evaluation and management.
Answered by 1 Apollo Doctors
My mom's been having issues with her high BP lately. She was on Telsartan 50 earlier, and then the doctor switched her to Amlip 5 about four months ago. It seemed okay at first, but now her BP is getting out of hand again. I'm really worried and wondering what could be causing this. Could it be that Amlip 5 isn't as effective for her as Telsartan was, or could something else be affecting her BP levels?
Dietary Tweaks:* 1. Increase protein intake: Include lean protein sources like chicken, fish, lentils, and legumes. 2. Fiber-rich foods: Add more fruits, vegetables, and whole grains. 3. Healthy fats: Nuts, seeds, avocados, and olive oil. 4. Hydration: Drink plenty of water (at least 8-10 glassesday). 5. Portion control: Eat smaller, frequent meals. *Non-Exercise Weight Loss Strategies:* 1. Stress reduction: Meditation, deep breathing, or yoga. 2. Sleep optimization: 7-8 hoursnight. 3. Walking breaks: Take short walks during work hours. 4. Desk stretches: Simple exercises at your workstation. 5. Active commuting: Walk or cycle to work, if possible.
Answered by 1 Apollo Doctors
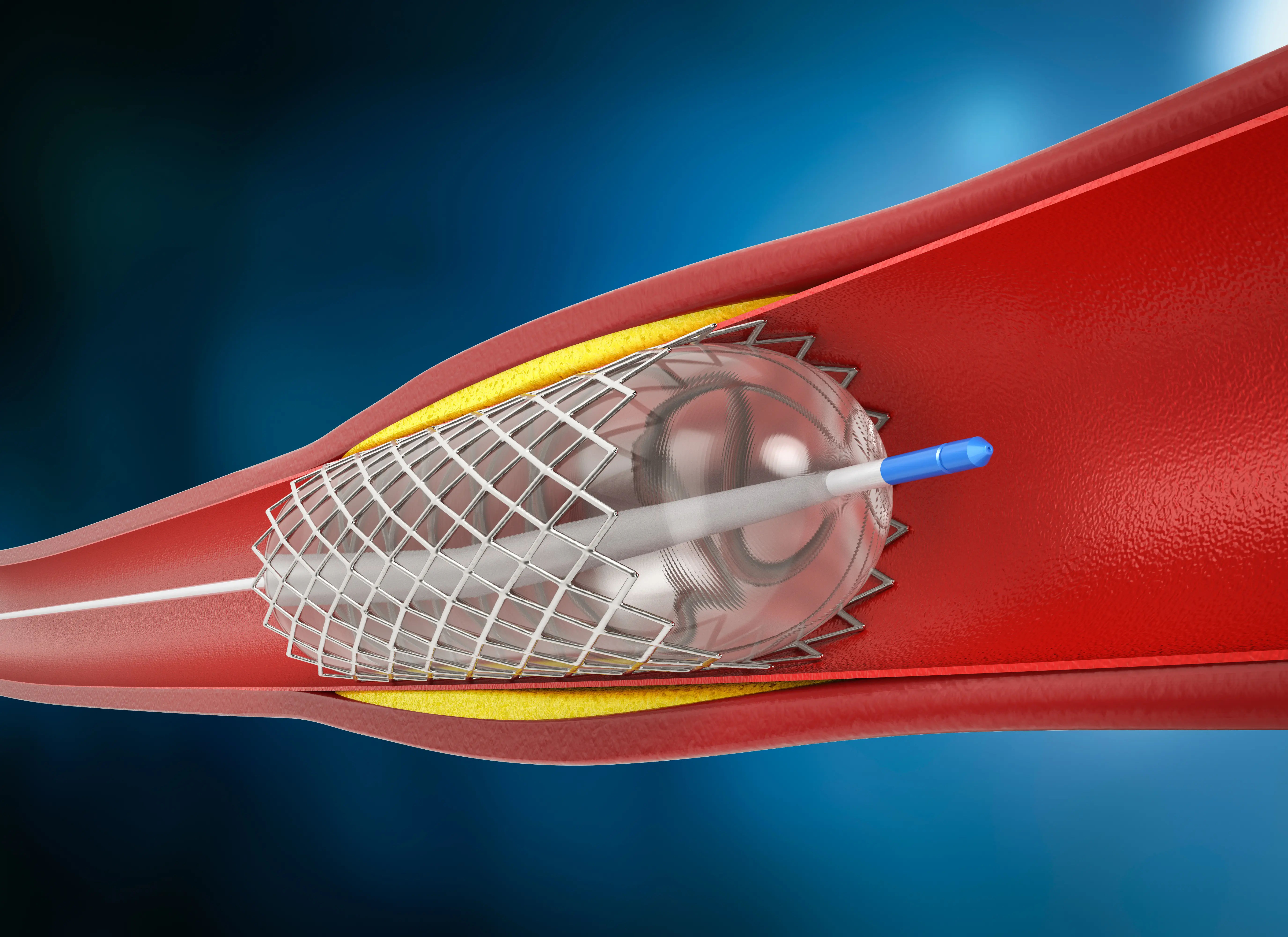
I'm having these frequent chest pains, and it's really stressing me out and leading to panic attacks. I went ahead and got a CT coronary angiography done, and the report came back saying my arteries are normal. Can I relax now and assume there aren't any heart-related issues, or is there something else I should be considering?
Hi, since your CT coronary angiography shows normal arteries, it is generally safe to assume that there are no significant heart-related issues causing your chest pain. However, it is always important to follow up with your healthcare provider for further evaluation and to discuss any other possible causes for your symptoms.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.