- male
- 55 Years
- 29/01/2025
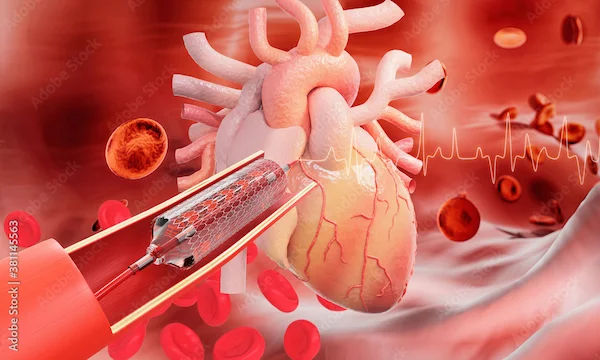
I'm a bit confused about my recent heart tests and need some advice. I had a TMT test that was positive a few months ago, and even after showing it to a cardiologist and doing an echo test, which was normal, they still suggested an angiogram because the TMT stayed positive. When comparing the latest TMT results to the previous one, it seemed slightly better but still came back positive. So, I went for a coronary angiogram and found out I have double vessel disease. The plan mentioned possibly needing a PTCA with a stent in the mid LCX RCA. I'm wondering if managing it with medication, diet, meditation, and exercise might be an option, or if the stent is really necessary. I don't have any symptoms like chest pain, hand pain, or dizziness, and my blood pressure and sugar levels have been under control for years. What do you suggest?
Answered by 1 Apollo Doctors
Based on your medical history and the findings from your tests, it is important to follow the treatment plan given by your healthcare provider. In addition to the PTCA with stent procedure, it is crucial to adhere to a healthy lifestyle which includes medication, diet, meditation, and exercise to help control your condition. The prescribed medications such as Aspirin, Clopidogrel, Atorvastatin, and Metoprolol will help in managing your condition. It is also essential to follow a heart-healthy diet low in saturated fats and cholesterol, engage in regular physical activity as advised by your healthcare provider, practice stress-reducing techniques like meditation, and maintain a healthy weight. Regular follow-up appointments with your cardiologist are necessary to monitor your condition and make any necessary adjustments to your treatment plan.
Dr. Ibrahim Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI'm yawning a lot at strange times and it's happening quite often. I've also had some pain on the left side of my chest, along with discomfort in my jaw and left neck sometimes. Every now and then there's this stabbing pain between my shoulder blades. I've had heart tests and an X-ray done, and they didn't show anything wrong. Sometimes I also feel short of breath. I'm just trying to figure out what's going on. Any ideas?
It sounds like you may be experiencing symptoms of anxiety or stress, which can manifest as excessive yawning, chest pain, jaw pain, neck pain, and stabbing pain between the shoulder blades. Breathlessness can also be a symptom of anxiety. I recommend trying to manage your stress levels through relaxation techniques, exercise, and possibly counseling. Additionally, you can take over-the-counter pain relievers like acetaminophen for the pain. If symptoms persist or worsen, please follow up with your healthcare provider for further evaluation and management.
Answered by 1 Apollo Doctors
I'm really worried about my wife's ECG results. It showed a Poor R Wave from V1 to V3. Could this mean a serious heart problem? What should we do next?
It is normal finding .
Answered by 1 Apollo Doctors
I'm really worried after my mom's health check-up today. Her blood pressure was really hightwice it was 18090 and the third time was 17090. We're going to get the full health report by Wednesday, but I'm anxious. Do you think she might need to start taking medicine right away?
The symptoms you're experiencing, such as lightheadedness, spinning sensation, and vomiting, could be related to various factors. Considering your recent changes in diet and daily workouts, here are a few potential causes: *Potential Causes* 1. *Low Blood Sugar*: With your new diet, you might be experiencing hypoglycemia (low blood sugar), leading to lightheadedness and dizziness. 2. *Dehydration*: Insufficient fluid intake, especially during workouts, can cause dehydration, resulting in dizziness and lightheadedness. 3. *Electrolyte Imbalance*: Your new diet might be lacking essential electrolytes like sodium, potassium, or magnesium, which can disrupt your body's balance and cause dizziness. 4. *Inner Ear Issues*: The spinning sensation could be related to inner ear problems, such as benign paroxysmal positional vertigo (BPPV). *Recommendations* 1. *Consult a Doctor*: Schedule an appointment with your primary care physician to rule out any underlying medical conditions. 2. *Monitor Blood Sugar*: If you're experiencing low blood sugar, consider monitoring your blood sugar levels and adjusting your diet accordingly. 3. *Stay Hydrated*: Drink plenty of water throughout the day, especially during and after workouts. 4. *Balance Your Diet*: Ensure you're getting essential electrolytes and nutrients through your diet or consider supplements after consulting your doctor. 5. *Rest and Recovery*: Allow your body time to recover between workouts, and prioritize getting enough sleep.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.


_1.webp)
