- male
- 45 Years
- 07/02/2025
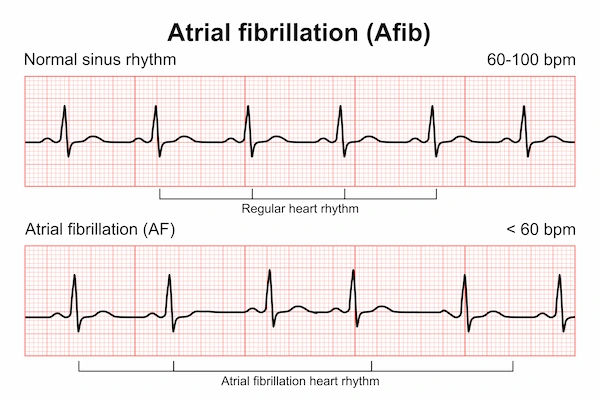
I'm really worried about my heart, and it's been like this for almost a year now. I've had palpitations around 45 times, and I've done a couple of ECGs, echoes, chest X-rays, and a TMT about 8 months ago, but everything came back normal. I don't have diabetes or thyroid issues, and I don't smoke or drink. There's no family history of heart problems either, but my BP is 140, and my LDL and total cholesterol are high at 140 and 192, respectively. The doctors say I shouldn't worry and just manage my BP and LDL, but I still can't shake off this fear of a heart attack. I often feel like I'm sinking or floating, and I get wobbly and fatigued when walking, sometimes even when I'm just resting. These feelings mostly hit me in the evenings, all the way until I go to sleep. I find myself worrying all the time, and there's just no joy or excitement in my day-to-day lifeit affects my ability to do daily activities. Can you help me figure out what's going on? Do you think I need any more tests, or is there something else I should be doing? What's causing all these issues?
Answered by 1 Apollo Doctors
It sounds like you are experiencing anxiety and panic attacks rather than a heart problem, especially since your heart tests have come back normal. Your symptoms of feeling like sinking and floating, wobbling, fatigue, and worry are common in anxiety disorders. It's good that you are focusing on controlling your blood pressure and LDL levels. To address your anxiety symptoms, you can try relaxation techniques, such as deep breathing exercises, meditation, or yoga. Regular physical activity can also help reduce anxiety. In some cases, therapy or counseling may be beneficial. For your elevated blood pressure and LDL levels, your doctors may prescribe medications to help manage them. For high blood pressure, medications like Amlodipine or Losartan can be prescribed. For high LDL levels, medications like Atorvastatin can be used to lower cholesterol levels. It's important to continue following up with your doctors for regular check-ups and to discuss any new or worsening symptoms. If you continue to experience anxiety symptoms, you may benefit from a consultation with a mental health professional for further evaluation and management.
Dr. Shubham Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI'm trying to understand the seriousness of some heart blockages that were reported. Can you explain what level of concern is typical for this kind of issue? Is there any immediate action I should be thinking about?
Patient is advised for angioplasty depending on the blockade of the coronary arteries. Cardiologist opinion is advised to the patient.
Answered by 1 Apollo Doctors
I did an ECG, echo, chest X-ray, and TMT about 2 months ago, and thankfully all the tests came back normal. Since then, Ive managed to get my blood pressure down to 12480. I'm 30 years old, a non-smoker, and I dont drink alcohol. Could you give me some advice on when I should consider repeating these tests?
Hi, since your previous tests were normal and you have controlled your blood pressure well, you can repeat the ECG, echo, chest x-ray, and TMT tests every 1-2 years for routine monitoring.
Answered by 1 Apollo Doctors
I've been having shortness of breath and recently got an Echo done, which said there was mild LVH. A couple of days ago, I noticed a little blood when I spit, and my doctor recommended I take Augmentin 625 and Montair LC for a week. I've been on them for two days now, but I noticed bright red blood when I spit again today, with no mucus color. I also have GERD and have had this issue for more than six years. Could the medication or the GERD be causing this, or should I be worried about something more serious?
check for TB once and review
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.