- male
- 50 Years
- 07/02/2025
I've been checking my blood pressure with a monitor, and every time the cuff gets tighter, I start feeling some chest pressure. It's not super strong, but I definitely notice it, and it happens every time I check. My blood pressure was 12588. I'm also worried because I get chest pains sometimes. What could be causing this?
Answered by 1 Apollo Doctors
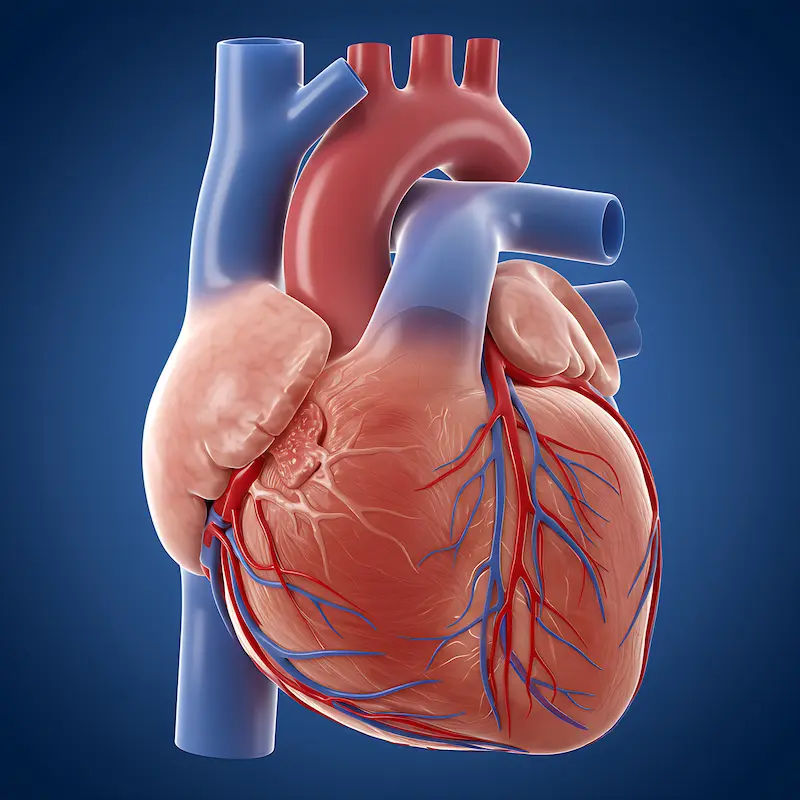
The sensation of chest pressure when the blood pressure cuff is tightened could be due to increased pressure on the chest wall. However, since you also mentioned that you experience chest pains sometimes, it is important to monitor this closely. With a blood pressure reading of 12588, it is within the prehypertension range. To help manage your blood pressure and chest discomfort, you can take a low dose of Amlodipine (brand name: Norvasc) 5mg once daily. Additionally, it is advisable to follow up with your healthcare provider for further evaluation and management.
Dr. Ranjith Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI've noticed my blood pressure is usually around 10462 during the day, but when I'm resting or sleeping, it drops into the 9050s range. I've been keeping an eye on it for about a month and the pattern seems pretty consistent. I had an echocardiogram earlier this year, and it showed I have a diastolic relaxation abnormality. I'm wondering if this could be causing my low blood pressure? Could it lead to more heart-related complications, or is it normal for blood pressure to drop like this at night? I've been feeling really fatigued and low on energy no matter how much I sleep, and it's a bit worrying. What do you think?
Low blood pressure during rest or sleep can be influenced by various factors, including underlying conditions such as diastolic dysfunction. In your case, the diastolic relaxation abnormality noted in your echocardiography may contribute to the lower blood pressure readings, especially during periods of rest. This can potentially lead to symptoms of fatigue and lack of energy. To address this issue, it is important to manage the underlying diastolic dysfunction. In addition, ensuring an adequate intake of fluids and electrolytes can help stabilize blood pressure. If symptoms persist, medications such as Midodrine or Fludrocortisone may be prescribed to raise blood pressure levels, especially during periods of rest or sleep. However, it is crucial to consult with your healthcare provider for a proper evaluation and personalized treatment plan.
Answered by 1 Apollo Doctors
I'm dealing with high blood pressure issues linked to my hypertension. Is it alright if I switch and take Metoprolol 25 mg x 2 tablets twice daily instead of Metoprolol Tartrate 50 mg twice daily?
Yes, you can take Metoprolol Succinate 25 mg (brand name: Toprol XL) twice daily as a substitute for Metoprolol Tartrate 50 mg. Just ensure to follow the prescribed dosage and frequency as directed by your healthcare provider.
Answered by 1 Apollo Doctors
Is it a big issue if I have cardiac conduction defects like PVC and PVAs? My May 2d echo came back normal, but the ECG still shows PVCs. Should I be worried about this?
Having cardiac conduction defects such as PVCs (Premature Ventricular Contractions) and PVAs (Premature Atrial Contractions) can sometimes indicate an underlying heart issue. While PVCs and PVAs are common and can be benign in many cases, they can also be associated with certain heart conditions. Since your 2D echo is normal, it is a good sign that the structure of your heart is normal. However, the presence of PVCs on ECG warrants further evaluation to determine the underlying cause and assess the overall heart function. In terms of medication, if your PVCs are symptomatic or concerning, your doctor may prescribe antiarrhythmic medications such as Flecainide or Propafenone to help regulate your heart rhythm. The dosage and duration of treatment will depend on your individual case and should be determined by your healthcare provider. Regular follow-up with a cardiologist is important to monitor your heart health and make any necessary adjustments to your treatment plan.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.