- female
- 31 Years
- 29/01/2025
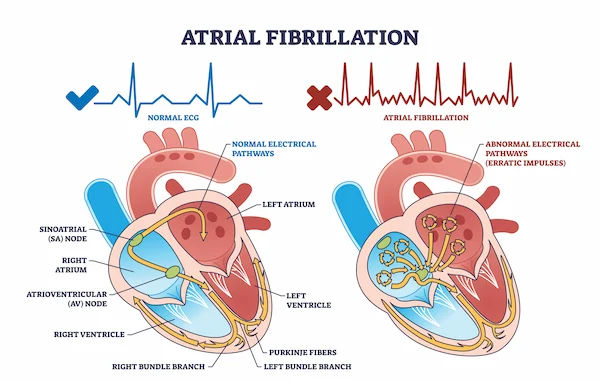
I've been having these sudden heart palpitations and some breathlessness since last week in May, and even when I do activities like slow walking or yoga, my heart rate spikes up to around 150-170. After seeing my cardiologist, I was on Inderal 10 mg for 2 months, but it didn't help much. Now I'm taking Betacap TR 40 and Daxid 25 mg, but sometimes my heart still races even when I'm just resting. My cardiologist mentioned that stress might be causing it. I'm really anxious to know when this might get better. I'm 31, breastfeeding, and all my tests like ECG, echo, thyroid, and sugar levels came back normal. I'm using my iWatch to track my heart ratehow reliable is that, or should I consider a different device?
Answered by 1 Apollo Doctors
Based on your symptoms and the medications you have tried, it seems like you are experiencing persistent tachycardia and palpitations despite the treatment. Since your cardiologist mentioned stress as a possible cause, it may take some time to see improvement as managing stress levels can be a gradual process. In addition to the medications you are currently taking (betacap tr 40 and daxid 25mg), your doctor may consider adjusting the dosage or trying other medications to better control your symptoms. It is important to continue following up with your cardiologist for further evaluation and management. Regarding monitoring your heart rate, while devices like the Apple Watch can provide useful information, they may not always be as accurate as medical-grade monitoring devices. If you are experiencing persistent symptoms and want more accurate heart rate monitoring, you may consider investing in a dedicated heart rate monitor recommended by your healthcare provider. It is essential to continue working closely with your cardiologist to address your symptoms effectively and monitor your progress over time.
Dr. Ibrahim Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allMy mom has had diabetes for 10 years and has been experiencing chest pain while walking for the last 3 months. We just got her angiography report, and the doctor suggested bypass surgery right away. Does she really need the surgery based on the findings?
It's crucial to understand that while your mother's symptoms and diabetes history are concerning, a definitive answer to whether bypass surgery is necessary requires a detailed review of the angiogram findings and a discussion with her doctor. Bypass surgery isn't always the first or best option, and other treatment options may be available.
Answered by 1 Apollo Doctors
I'm looking over my brother's medical report, and I'm curious about his high sensitive troponin I levelit came back as 0.05. Is this something to worry about? Can you help me understand if this is within a normal range or if there might be cause for concern?
High sensitive troponin I level of 0.05 ngmL is within the normal range. Troponin levels are often used to diagnose heart attacks or other heart-related conditions. In this case, the level of 0.05 ngmL is not concerning and does not indicate any acute heart issues. It is important to consider other factors and symptoms in conjunction with this result for a comprehensive evaluation. If your brother is experiencing any symptoms or concerns, it is recommended to follow up with his healthcare provider for further assessment and guidance.
Answered by 1 Apollo Doctors
I'm having this chest pain on the left side about 30 to 40 minutes after falling asleep, and it even comes with a bit of sweating. Once it starts, I can't find a comfortable position to sleep in without it hurting, so I've been sleeping in an easy chair for the past five days. I started taking Tonact TG for my high cholesterol, which is 290. I'm also on Thyronorm 75 and Telmisartan 40. My TSH levels and blood pressure are normal. Should I be worried about this chest pain and what should I do about it?
It sounds like you're experiencing discomfort that could be related to a few different factors, including your cholesterol and medications. Since the pain is persistent and affects your sleep, it's important to follow up with your doctor to rule out any heart-related issues and ensure the medications are working well for you. If the pain persists, consider an evaluation for possible musculoskeletal causes or other conditions that might be contributing.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.