- male
- 50 Years
- 22/01/2025
I've been tracking my triglycerides, and they were around 260. Lately, I've started doing a brisk walk every day for about 1.5 hours, just following what my doctor suggested. After about 20 days, my triglycerides dropped to 156. Is it normal for them to fall that much, or should I think about getting retested? Also, I'm curious whether high lipid profiles from before can get stuck in the arteries, or do they clear out once the levels go down?
Answered by 1 Apollo Doctors
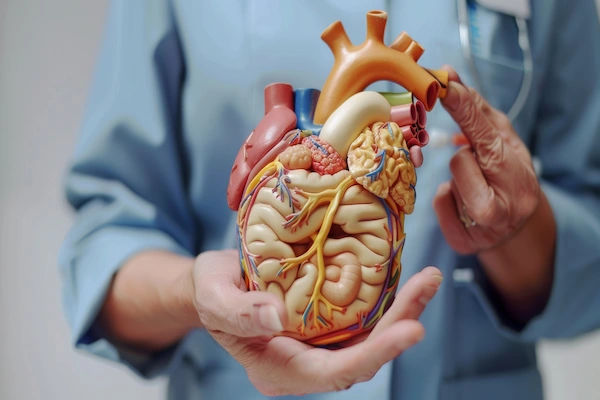
It is possible for your triglyceride levels to decrease with regular exercise like brisk walking. However, it is advisable to repeat the test to confirm the improvement. As for the second part of your question, high lipid profiles can contribute to the buildup of plaque in your arteries over time. Lowering your lipid levels, such as triglycerides, through lifestyle changes and medication can help reduce this buildup and lower the risk of cardiovascular diseases.
Dr. Ranjith Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI've been dealing with heart anxiety since 2011 and had a bunch of tests done back in 2015. Everything seemed normal then but recently, I got an echo done in August that showed mild MRTR grade 1 DD. I also did some ECGs and they showed issues likely because of a fast heart rate or tachycardia. The doctor suggested a stress echo and I went through that last week. Could you take a look at the report? I'm a bit worried because my tests were normal in 2015 and now there's something going on. What do you think?
You have a history of heart anxiety since 2011 and have undergone multiple tests, including an echo in August which showed mild mitral regurgitationtricuspid regurgitation grade 1 and grade 1 diastolic dysfunction. After experiencing issues with fast heart rate tachycardia on recent ECGs, your doctor suggested a stress echo which you have completed. It would be helpful to review the report to provide a more accurate recommendation. Please provide the details of the stress echo report for further evaluation.
Answered by 1 Apollo Doctors
I'm really concerned because over the last three months, I've been noticing that my heart occasionally skips a beatit happens about an hour a day. My blood pressure is also around 14090. I've had some tests done, like an echo and a Holter monitor, and my doctor mentioned something about trivial mitral regurgitation. Should I be worried about this and the skipped heartbeats? What does all of this mean for my heart health?
Trivial mitral regurgitation is a common finding and usually does not cause any symptoms or require treatment. As for the skipped heart beats, if they are occasional and not causing any other symptoms, they may not be concerning. However, since you are experiencing them frequently, it would be best to follow up with your doctor for further evaluation. In the meantime, you can try to manage your symptoms by reducing stress and anxiety. If your doctor deems it necessary, they may prescribe medications such as beta-blockers like Metoprolol to help regulate your heart rate and blood pressure. It is important to follow your doctor's recommendations for further management.
Answered by 1 Apollo Doctors
How do you feel when you have high blood pressure?
Most people who have high blood pressure do not have symptoms. In some cases, people with high blood pressure may have a pounding feeling in their head or chest, a feeling of lightheadedness or dizziness, or other signs.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.