- female
- 30 Years
- 29/01/2025
I've been wondering if you could help me figure out what's going on because I've been feeling strange lately. Around 12 April, I tested positive for COVID, but luckily, it was mild, and the only real issue was losing my sense of smell, which came back after about 10 days. But for the past 8-10 days, I've been experiencing this weird sensation all over my bodyalmost like heart palpitations, though I'm not entirely sure if that's what it is. It's like I can feel my heartbeat in my stomach, neck, and just about everywhere in my body, like my whole body is pumping. It tends to disappear when I'm doing something else, but comes roaring back when I'm trying to relax. If I focus on it too much, my heart really starts pounding before eventually calming down. It's really unsettling and sometimes makes me feel anxious and on edge. Do you have any idea what might be causing this or what I should do about it?
Answered by 1 Apollo Doctors
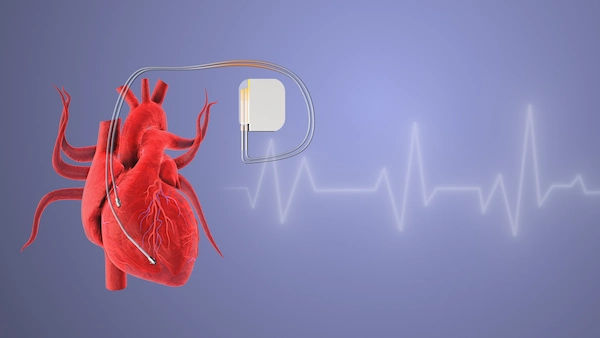
It sounds like you may be experiencing palpitations and anxiety following your COVID-19 infection. To help with your symptoms, you can try taking Propranolol 20mg twice a day. This medication can help reduce palpitations and anxiety by slowing down your heart rate. Additionally, practicing relaxation techniques such as deep breathing exercises or mindfulness meditation may also be beneficial in managing your symptoms. If your symptoms persist or worsen, please consult your healthcare provider for further evaluation and management.
Dr. Dr Khaleel Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
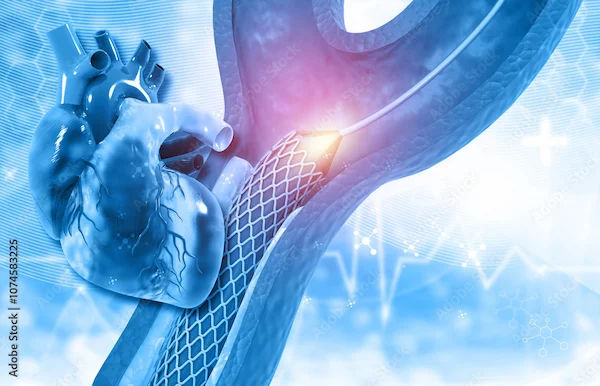
View allI'm really confused because my Echo and ECG tests came back normal, but I'm still experiencing these palpitations. I'm a GERD patient, and whenever these palpitations hit, I get really nervous. What could be causing this, and is there anything I should be doing or looking out for?
Palpitations despite normal Echo and ECG in a GERD patient could be due to acid reflux irritating the vagus nerve, leading to palpitations. In such cases, managing GERD effectively can help reduce palpitations. You can try taking Omeprazole 20mg once daily before breakfast for GERD.
Answered by 1 Apollo Doctors
I'm having some pain on the left side of my chest and it's really worrying me. I'm also diabetic and on top of that, I'm supposed to have cervical surgery soon. Could these chest pains be related to my diabetes or maybe the upcoming surgery? I'm kind of anxious about it all and I'm wondering what I should do next.
Sometimes pain in the left side of the chest can be concerning, especially if you have a history of diabetes and are scheduled to undergo cervical surgery. This pain could be due to various reasons such as musculoskeletal issues, heart problems, or even related to your diabetes. It's important to get this evaluated by a healthcare professional. To help with the pain, you can take acetaminophen (Tylenol) 500mg every 6 hours as needed. However, if the pain persists or worsens, it is important to seek medical attention promptly.
Answered by 1 Apollo Doctors
I'm looking at my cholesterol numbers and I'm a bit worried. My total cholesterol is 226.3 mgdL, LDL is 145.7 mgdL, and triglycerides are 190.5 mgdL. Is this something I should be really concerned about? What does this mean for my health?
Cholesterol total of 226.3mgdl, LDL cholesterol of 145.7mgdl, and triglycerides of 190.5mgdl indicate slightly elevated levels, which may increase the risk of heart disease. To help lower these levels, you can consider taking Atorvastatin 20mg once daily to lower LDL cholesterol and Fenofibrate 145mg once daily to lower triglycerides. Additionally, lifestyle changes such as a healthy diet, regular exercise, and weight management can also be beneficial.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.