- male
- 30 Years
- 29/01/2025
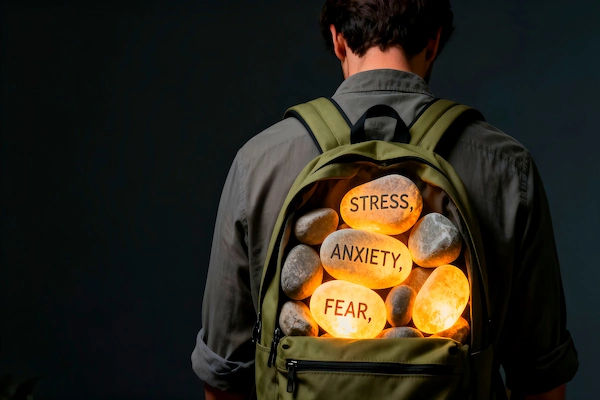
I've had a couple of HIV tests after possible exposure. At 3 months, both the 4th gen rapid test and HIV antibody test from the lab came back negative. Then I waited until 5 months and did another 4th gen CMIA test for p24 AG and antibodies, and that was negative too. I'm really anxious about whether these results are conclusive. Do you think I need any more testing, or can I finally relax?
Answered by 1 Apollo Doctors
Post-COVID-19 Recovery Symptoms
Your Symptoms
- Low-grade fever: Mild fever, usually less than 101F (38.3C).
- Body pain: Mild muscle and joint pain.
- Stuffy nose: Nasal congestion.
Possible Causes
- Residual inflammation: Lingering inflammation from the COVID-19 infection.
- Post-viral fatigue syndrome: A common condition after viral infections, characterized by persistent fatigue, muscle pain, and other symptoms.
Medication and Self-Care
- Over-the-counter pain relievers: Acetaminophen (Tylenol) or ibuprofen (Advil) for body pain and fever.
- Decongestants: Pseudoephedrine (Sudafed) or phenylephrine (Sudafed PE) for stuffy nose.
- Rest and hydration: Prioritize rest, drink plenty of fluids, and maintain a balanced diet.
- Monitor symptoms: If symptoms worsen or persist, consult your doctor.
Consult Your Doctor
- Schedule a follow-up appointment: Discuss your symptoms and receive personalized guidance.
- Report any severe symptoms: If you experience difficulty breathing, chest pain, or severe headache, seek immediate medical attention.
Dr. Dhankecha Suggests...
Consult a Infectious Disease specialist
Answered 04/07/2025
0
0

More Infectious Disease Health Queries
View allI'm dealing with this recurring infection caused by Staphylococcus aureus bacteria, and it keeps showing up every couple of months since it first appeared in January 2019. I've had it in various placeslike my knee, finger, chin, nose, and scrotum. Even after seeing multiple doctors and taking antibiotics like Linezolid and Clarithromycin, the infection just popped up again on my right scrotum, and every time it brings on a fever. I've even had surgery for a carbuncle on my knee under anesthesia. The pus and blood cultures both came back positive for Staph A, but my nasal swab results were negative both times, and blood cultures were too. I'm really struggling to figure out why this keeps happening and would appreciate any guidance on how to stop these infections from coming back. What could be causing this, and is there anything specific I should be doing to prevent it?
Recurring Staphylococcus aureus infections indicate a persistent underlying issue. To address this, consider: Medical Evaluation 1. Comprehensive metabolic panel (CMP) to rule out diabetes, kidney issues, or electrolyte imbalances. 2. Complete blood count (CBC) to assess immune function. 3. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) to monitor inflammation. 4. Staphylococcus aureus susceptibility testing to determine antibiotic resistance patterns. 5. Nasal swab and skin cultures to identify potential carriers. Infection Prevention Strategies 1. Personal Hygiene: Frequent handwashing, showering, and cleaning. 2. Skin Care: Moisturize, avoid irritants, and use antibacterial soap. 3. Antibiotic Stewardship: Avoid unnecessary antibiotic use. 4. Immunizations: Ensure up-to-date on influenza, pneumococcal, and tetanus vaccines. 5. Stress Management: Yoga, meditation, or deep breathing exercises. Root Cause Investigation 1. Carrier State: Nasal or skin colonization. 2. Underlying Conditions: Diabetes, eczema, or other skin conditions. 3. Environmental Factors: Contaminated surfaces or water. 4. Genetic Predisposition: Family history of Staph infections. Treatment Considerations 1. Long-term Antibiotics: Consider oral antibiotics (e.g., doxycycline or minocycline) for 6-12 months. 2. Topical Treatments: Antibiotic ointments or creams. 3. Surgical Intervention: Drainage or debridement for severe infections. Recommended Specialists 1. Infectious Disease Specialist 2. Dermatologist 3. Orthopedic Surgeon (for skin and soft tissue infections)
Answered by 1 Apollo Doctors
I've recently done a dengue test and the results showed NS1 weakly positive, but IgM and IgG are both negative. I'm a bit confused about what this means and what kind of treatment I should be looking at. Could you help me understand this better?
Concerns about a child's fever are natural. _Current situation:_ 1. _Age_: 1.5 years 2. _Fever_: 101.4F (38.6C) 3. _Medication_: Crocin (6ml) since yesterday night _Next steps:_ 1. _Consult a pediatrician_: Reach out to your child's pediatrician for guidance. 2. _Monitor temperature_: Continue tracking your child's temperature. 3. _Watch for other symptoms_: Look for signs of distress, such as difficulty breathing, vomiting, or diarrhea. 4. _Keep your child hydrated_: Offer plenty of fluids, like breast milk, formula, or electrolyte-rich beverages. _When to seek immediate attention:_ 1. _Fever above 104F (40C)_ 2. _Difficulty breathing_ 3. _Vomiting or diarrhea_ 4. _Refusal to drink fluids_ 5. _Seizures or convulsions_ Consult a pediatrician for personalized advice.
Answered by 1 Apollo Doctors
Gosh, Im feeling a bit anxious and really need some clarity. I did an HIV test using Elisa two years after potentially being exposed, and the result was 0.32. Earlier, I also had a rapid antigen test which was non-reactive. Do these results mean Im in the clear, or should I be worried?
negative
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.