Guide to Neurosciences Interventional Neurology/bi Plane Labs Advanced Technology Neurovascular
Discover Interventional Neurology, the minimally invasive treatment for strokes, aneurysms, and AVMs. Learn how advanced Bi-Plane Labs enable precise, life-saving procedures through tiny incisions. Find out what matters in rapid neurovascular care.

Written by Dr. Mohammed Kamran
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
If a loved one has a stroke or you’ve been told you have a brain aneurysm, you want the fastest, safest treatment possible. That’s where interventional neurology—sometimes called neurointerventional radiology—comes in. Using tiny catheters and real-time X-ray imaging inside a specialised “bi-plane” lab, these neurosciences experts can remove clots, seal aneurysms, and fix abnormal connections in blood vessels without opening the skull. In this guide, we’ll demystify how interventional neurology works, why bi-plane labs are considered the gold standard for neurovascular care, and what to expect before, during, and after a procedure. We’ll also show you how to evaluate a hospital’s readiness, interpret outcomes like TICI and mRS in simple terms, and understand innovations—such as AI stroke triage—that are reshaping access to life-saving care. Whether you’re seeking preventive advice or navigating urgent decisions, this comprehensive resource in neurosciences, interventional care, and neurology/bi-plane technology will help you move forward with confidence.
Interventional Neurology in the Neurosciences: A Plain-Language Overview
This is a minimally invasive medical speciality that treats blood vessel problems of the brain and spine using highly
precise catheter techniques.
Consult Top Neurologists for Personalised Advice
Interventional neurology is a minimally invasive approach to diagnosing and treating blood vessel problems of the brain and spine. Instead of opening the skull or performing large incisions, specialists guide thin tubes (catheters and microcatheters) through an artery—often from the wrist or groin—up to the brain under live X-ray. Once in place, they can remove a clot (mechanical thrombectomy), seal an aneurysm (coiling, stents, or flow diverters), glue or plug abnormal vessels (embolisation), or open a narrowed artery with angioplasty and stenting. These procedures happen inside an advanced imaging suite called a neurovascular or bi-plane lab.
The Interventional Team
Typically, a neurointerventionalist (trained in neurology, neurosurgery, or radiology) leads the procedure. They work alongside stroke neurologists, neuroanaesthesiologists, specialised nurses, technologists, and often neurosurgeons. The team approach is central to modern neurosciences care—especially for time-critical stroke treatment.
Why Choose Interventional Care?
Compared to open surgery, endovascular procedures often mean quicker treatment, smaller incisions, shorter hospital
stays, and faster recovery. They’re especially valuable when speed is essential, such as in large-vessel ischaemic stroke,
where every minute saved protects millions of brain cells. Understanding what interventional neurology is key to
appreciating this minimally invasive approach.
Unique Insight: Think of interventional neurology like “keyhole plumbing” for the brain—using the inside of blood
vessels as the pathway to fix problems from within. That means many conditions that once demanded major surgery
can be treated through a needle-sized opening.
Bi-Plane Labs: Advanced Technology for Neurovascular Precision
These advanced imaging suites use two X-ray sources and detectors positioned at $90^\circ$ angles to provide
immediate, simultaneous 3D-like views of the brain's delicate vessels.
A bi-plane angiography suite uses two X-ray cameras positioned at right angles to each other. By capturing two views at
once, your team can see the brain’s delicate vessels in stereo-like detail without constantly repositioning the equipment.
This dual-plane approach helps shorten procedure time, reduce contrast dye use, and lower radiation exposure
compared with single-plane systems, while improving visualisation for complex cases like aneurysms near critical
branches. Technology leaders have paired bi-plane systems with flat-panel detectors, 3D rotational angiography
(3DRA), and cone-beam CT that produce CT-like images right in the lab—helpful for confirming device placement or
checking for bleeding before leaving the suite.
Why Dual-Plane Imaging Matters
In neurovascular work, vessels can be less than a millimetre wide. Seeing two planes simultaneously helps operators
navigate tortuous anatomy, deploy stents with precision, and confirm full coverage of aneurysm necks with flow
diverters. In stroke, better visualisation can aid faster clot retrieval and fewer device passes.
Safety Advantages
Dual-plane imaging can reduce “fluoro time” (time under X-ray), and modern systems include dose-saving algorithms,
filtration, and collimation to narrow the beam to exactly where it’s needed. Many centres track dose-area product
(DAP) and use real-time dose maps to adjust technique on the fly.
Unique Insight: The best labs don't just have advanced machines—they're “tuned” to neuro workflows: preloaded
stroke protocols, room layouts that keep anaesthesia and nursing teams in sync, and rapid transitions from diagnostic
runs to therapy. Ask if the lab supports cone-beam CT and 3DRA; these tools can change decisions in the moment.
Conditions Interventional Neurology Treats
The speciality is crucial for treating sudden blockages, weak bulges in vessels, and abnormal artery-vein connections in
the brain.
Acute Ischaemic Stroke (Large Vessel Occlusion, LVO)
A clot blocks a major brain artery (often the middle cerebral, internal carotid, or basilar). Interventional teams perform
mechanical thrombectomy—threading a catheter to the clot and removing it using a stent retriever or aspiration system.
Evidence shows significant improvement in independence for eligible patients when treated rapidly.
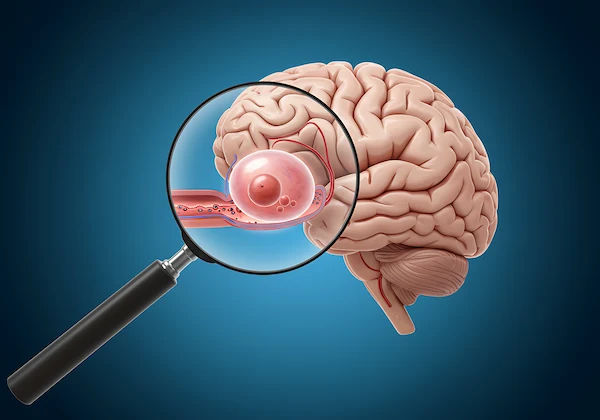
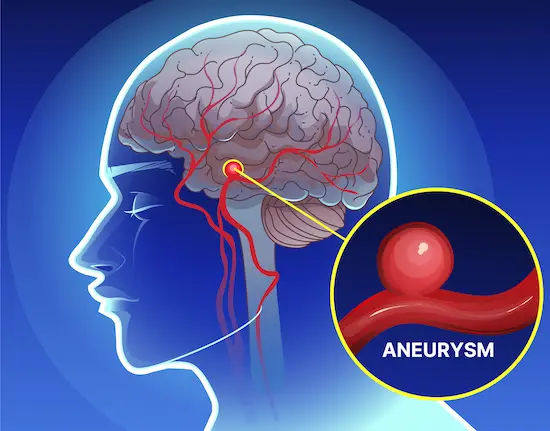
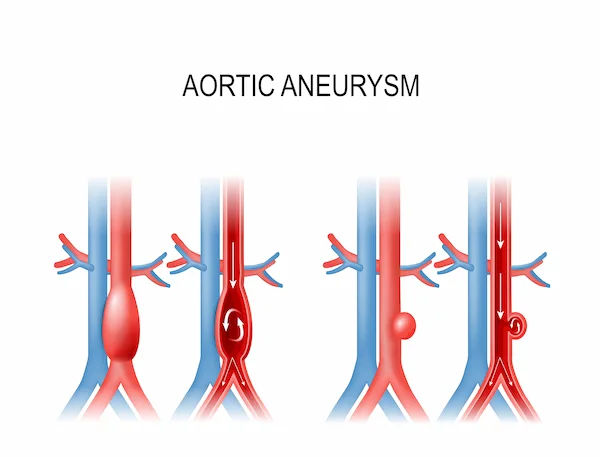
Brain Aneurysms
Weak bulges in artery walls can rupture and cause subarachnoid haemorrhage. Endovascular options include coil
embolisation (packing the aneurysm with platinum coils), stent-assisted coiling, and flow diverters (fine-mesh stents that
redirect blood and promote aneurysm healing). Choice depends on aneurysm size, shape, and location.
Arteriovenous Malformations (AVMs) and Dural Arteriovenous Fistulas (dAVFs)
Abnormal connections between arteries and veins can be embolised using liquid agents (e.g., Onyx), sometimes as a
standalone treatment or staged before surgery or radiosurgery. Knowing the details of an AVM embolisation procedure
helps in understanding the care plan.
Other Treated Conditions
- Carotid stenosis and intracranial atherosclerosis: Balloon angioplasty and stenting can restore blood flow when the
narrowing is severe and symptomatic. - Spinal vascular lesions and tumour embolisation: Embolisation can reduce blood flow to spinal AVMs or to tumours to
make surgery safer.
Unique Insight: Many conditions are best treated by a hybrid plan—combining interventional, surgical, and radiation
options in stages. A centre with a multidisciplinary neuroradiology-neurology-neurosurgery board can individualise
care.
What Happens During a Neurovascular Procedure
The procedure involves careful preparation, minimally invasive access, precise device navigation using real-time
imaging, and immediate post-procedure monitoring.
Before You Arrive
You’ll likely undergo a CT or an MRI to define the problem and guide the plan. In emergencies (stroke), CT
angiography quickly maps vessels; in elective cases (aneurysm), catheter angiography remains the gold standard for
detail. You’ll review allergies (especially to contrast dye), kidney function labs, and medicines (blood thinners). You’ll
sign consent forms discussing benefits and risks.
In the Suite
After IV lines are placed, anaesthesia may be local with sedation or general anaesthesia. Access is obtained via a small
puncture in the femoral artery (groin) or radial artery (wrist). Through a guiding catheter, a microcatheter navigates
under bi-plane imaging to the target. For thrombectomy, the team uses aspiration catheters or stent retrievers to remove
the clot; for aneurysms, coils and devices are deployed; for embolisation, a liquid agent or plugs are delivered to shut
down abnormal flow. Cone-beam CT or 3DRA may be performed mid-procedure to confirm results.
Aftercare
You’ll be monitored for blood pressure, neurologic status, and the puncture site. Most patients lie flat briefly after
femoral access; radial access can allow earlier mobility. Imaging follow-up varies: post-stroke scans, 6- to 12-month
aneurysm surveillance (MRA/CTA/DSA) to ensure durable results, and clinic visits to adjust medications.
Unique Insight: Ask about transradial (wrist) access. In some patients, it can reduce access-site bleeding, speed
recovery, and improve comfort—though complex neurovascular anatomy sometimes still favours femoral access.
If you’re being evaluated for stroke symptoms, seek emergency care immediately. For non-emergent concerns or post-
procedure questions, you can consult a doctor online with Apollo 24|7 for guidance and follow-up planning. Apollo24|
7 also offers convenient home collection for tests like lipid profile and HbA1c that help track stroke risk factors.
Evidence and Outcomes: Why Speed and Technique Matter
Fast intervention for large-vessel stroke, supported by robust clinical evidence, is critical for achieving the best chance of
functional recovery.
Randomised trials and pooled analyses have transformed stroke care. The HERMES meta-analysis showed that for
carefully selected patients with large-vessel occlusion, mechanical thrombectomy significantly increases the chance of
functional independence at 90 days compared to best medical therapy alone, without a prohibitive increase in
symptomatic bleeding. AHA/ASA guidelines recommend thrombectomy within established time windows, with
advanced imaging used to select patients even up to 24 hours after symptom onset in certain cases.
Outcome Measures in Plain Terms
- TICI (Thrombolysis in Cerebral Infarction) score: A grade (0–3) of how well blood flow is restored. TICI 2b/3 (good to
complete reperfusion) correlates with better recovery. - mRS (modified Rankin Scale): A 0–6 scale of disability at 90 days. mRS 0–2 means independence in daily activities;
lowering mRS is a key goal of care.
Time is Brain
Door-to-puncture (arrival to start of procedure) and door-to-reperfusion times are tracked closely; every 15-minute delay
reduces the likelihood of a good outcome. High-performing centres standardise workflows: parallel processing for
imaging and consent, premade “thrombectomy trays,” and 24/7 team readiness. Mechanical thrombectomy success
rates are tightly linked to these metrics.
Unique Insight: Ask a centre about its median door-to-puncture time, its rate of TICI 2b/3 reperfusion, and how often
thrombectomy is started within 60 minutes of arrival. These metrics are as important as having a bi-plane lab—they tell
you how effectively it’s used.
Safety, Risks, and Patient Recovery
Minimising radiation and contrast exposure, managing bleeding risks, and comprehensive post-procedure follow-up are
central to patient safety.
Safety Measures
- Radiation: Modern bi-plane systems include dose-reduction tools, and experienced teams track your cumulative dose
using protocols to keep dose As Low As Reasonably Achievable (ALARA). - Contrast Dye: Iodinated contrast can rarely trigger allergic reactions or stress the kidneys. Preventive steps include
hydration, using the lowest dose needed, and premedication if you’ve had contrast reactions before. - Procedure Risks: Risks can include access-site bleeding, vessel injury, stroke extension, haemorrhage, or device-related
issues. However, in properly selected patients, benefits typically outweigh risks.
Recovery and Follow-up
- For stroke, rehabilitation (physical, occupational, and speech therapy) begins early.
- For aneurysms and AVMs, follow-up imaging (MRA/CTA/DSA) ensures durable occlusion.
- Blood pressure control, smoking cessation, and medication adherence (antiplatelets after stents/flow diverters) are
essential. Recovery after aneurysm coiling typically involves a few days of observation.
Unique Insight: Ask your team about “contrast stewardship” and whether they use cone-beam CT to answer questions
mid-procedure. Avoiding a return trip to the lab can reduce both risk and anxiety. If symptoms persist beyond two
weeks after a procedure—such as worsening headache, new weakness, or speech changes—consult a doctor online with
Apollo 24|7 for further evaluation or book a physical visit if advised.
Choosing the Right Centre and Team
For the highest level of neurovascular care, select a high-volume Comprehensive Stroke Centre (CSC) with a dedicated,
multidisciplinary team.
- Comprehensive Stroke Centres (CSCs) provide 24/7 thrombectomy, neurosurgery, neurocritical care, and advanced
imaging. - Primary Stroke Centres stabilise and give clot-busting drugs (when appropriate) and transfer patients to CSCs for
thrombectomy. - For aneurysms, AVMs, and complex cases, look for high-volume centres with a dedicated neurointerventional
programme. The process of choosing a comprehensive stroke centre should involve researching its capabilities and
outcomes.
Looking Ahead: Innovation, Access, and Patient Empowerment
Future advancements in AI, new device technology, and streamlined workflows promise to further increase the speed
and effectiveness of neurointerventional treatments.
Workflow and Technology Innovations
- AI Triage and Mobile Stroke Workflows: AI tools can flag suspected large-vessel occlusions (LVO) on CT angiography
and push alerts to interventional teams, shrinking time to treatment. AI stroke triage is a major advancement. - Next-Gen Devices: Flow diverters are expanding to smaller vessels; intrasaccular devices provide options for wide-
necked aneurysms without long stents. Low-profile catheters improve access in tortuous anatomy.
Prevention and Long-Term Health
- For stroke and aneurysm risk reduction, manage blood pressure, lipids, diabetes, and smoking.
- Apollo24|7 offers convenient home collection for tests like lipid profile and HbA1c, helping you and your doctor track
and optimise risk factors over time. Prevention strategies after stroke are crucial for long-term health.
Unique Insight: Ask if your centre uses “pre-notification” apps where EMS can transmit imaging as you’re en route; this
can mobilise the neurointerventional team before you arrive.
Conclusion
Interventional neurology sits at the intersection of cutting-edge technology and urgent clinical need. In a modern bi-
plane lab, specialists navigate tiny catheters through delicate neurovascular pathways to reverse strokes, secure
aneurysms, and fix complex vessel malformations—often within minutes that matter. The strongest evidence supports
fast, expertly executed mechanical thrombectomy for large-vessel stroke, and newer devices have broadened minimally
invasive options for aneurysms and AVMs. As you choose where to seek care, look beyond the equipment to the team’s
outcomes and readiness: 24/7 coverage, streamlined workflows, and transparent quality metrics. Empower yourself
with clear questions, understand the safety steps taken on your behalf, and partner with a centre committed to prevention and long-term follow-up. If you need help managing risk factors or clarifying next steps after discharge, consult a doctor online with Apollo 24|7; and consider home collection for key blood tests to track your progress. With the right team and technology, neurosciences, interventional care, and bi-plane imaging offer a path to safer procedures, better outcomes, and renewed confidence.
Consult Top Neurologists for Personalised Advice
Consult Top Neurologists for Personalised Advice

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(100+ Patients)

Dr. Soniya Tambe
Neurologist
16 Years • MBBS, MD, DM(NEUROLOGY), FEBN (European board of neurology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Consult Top Neurologists for Personalised Advice

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(100+ Patients)

Dr. Soniya Tambe
Neurologist
16 Years • MBBS, MD, DM(NEUROLOGY), FEBN (European board of neurology)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
More articles from Aneurysm
Frequently Asked Questions
1) What is interventional neurology, and how is it different from neurosurgery?
It’s a minimally invasive speciality that treats brain and spine blood vessel problems using catheters guided by X-ray in a bi-plane lab. Neurosurgery involves open operations. Many conditions can be treated either way; your team will advise on the safest option.
2) Why is a bi-plane angiography suite better than a single-plane system?
Bi-plane labs capture two X-ray views at once, helping doctors see complex anatomy, reduce procedure time, and potentially lower radiation and contrast use, which may translate into safer, more precise neurointerventional care.
3) How effective is mechanical thrombectomy for stroke?
For eligible patients with large-vessel occlusion, thrombectomy significantly increases the chance of independence at 90 days compared with medicine alone, especially when performed quickly and with high-quality reperfusion (TICI 2b/3).
4) What are the risks of a cerebral angiogram, and how is recovery?
Risks include bleeding at the access site, contrast reactions, kidney strain, or, rarely, vessel injury or stroke. Most patients go home the same or the next day, with puncture-site care and temporary activity limits.
5) How do I choose the right hospital for an aneurysm or AVM?
Look for a Comprehensive Stroke/Neurovascular Centre with a bi-plane lab, high case volumes, 24/7 coverage, and transparent metrics (complication and retreatment rates). Ask about device options (coils, stents, flow diverters) and multidisciplinary planning.