Appendicitis: Symptoms, Diagnosis, Treatment Guide
Understand appendicitis symptoms, diagnosis, and treatment options. Learn how to spot early signs, when surgery or antibiotics are needed, recovery timelines, and care tips for adults, children, pregnancy, and older adults.


Introduction
Appendicitis is an inflammation of the appendix that can escalate quickly from nagging abdominal discomfort to a surgical emergency. While some cases are mild, others progress to perforation (a “burst” appendix) that can cause serious infection. Knowing how appendicitis starts, what symptoms to watch for, how it’s diagnosed, and the best treatment options—surgery or antibiotics—can help you act fast and make informed choices.
In this guide, we break down appendicitis in clear language: early and classic symptoms, causes, tests your doctor may order, what to expect from a laparoscopic appendectomy, and when non-surgical treatment makes sense. You’ll also find practical advice for parents, people who are pregnant, and older adults; tips to avoid delays; questions to ask your care team; and evidence from recent studies.
If you suspect appendicitis, do not delay seeking care. Severe or worsening pain, fever, vomiting, or pain that localises to the lower right abdomen needs urgent evaluation. If you’re unsure, you can start with an online consultation to triage, but with concerning symptoms, go to the nearest emergency department.
What Is Appendicitis?
Here’s what appendicitis is and how it develops.
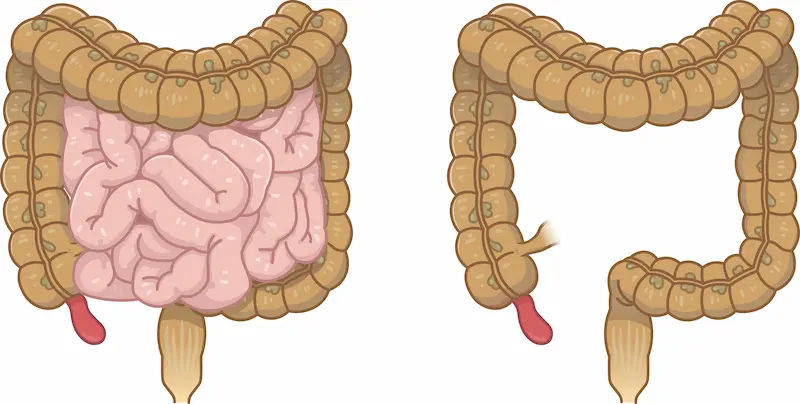
The Appendix: A Quick Primer
The appendix is a small, finger-like pouch attached to the first part of the large intestine in the lower right abdomen. It contains immune tissue and gut bacteria but isn’t essential for digestion in modern humans. Appendicitis happens when the appendix becomes blocked and inflamed, usually by hardened stool (a fecalith), swollen lymph tissue, or, less commonly, parasites or tumours. The blockage leads to swelling, bacterial overgrowth, and rising pressure, which can cut off blood supply and cause perforation if untreated.
Uncomplicated vs Complicated Appendicitis
Doctors often divide appendicitis into:
- Uncomplicated: Inflamed appendix without rupture or abscess. Traditionally treated with surgery, but antibiotics alone can sometimes be an option.
- Complicated: Perforation (rupture), abscess (pocket of infection), phlegmon (inflamed mass), or generalised peritonitis. These require more urgent or staged treatment—often drainage plus antibiotics, and usually surgery.
Knowing which type you have guides imaging, treatment, and urgency. Imaging (ultrasound, CT, MRI) helps distinguish these categories.
How Appendicitis Feels: Early and Classic Symptoms
Here’s how appendicitis typically presents at different stages.
Appendicitis often starts with vague discomfort near the belly button, then over hours migrates to the lower right quadrant (RLQ). Common symptoms include:
- Dull pain that sharpens and localises to the RLQ
- Loss of appetite, nausea, and sometimes vomiting
- Low-grade fever and chills
- Worsening pain with walking, coughing, or jarring movements
- Constipation or diarrhoea, and abdominal bloating in some cases
Adults vs Children, Older Adults, and Pregnancy
- Adults: Classic migration of pain from the centre to the RLQ is typical. Many describe “the worst stomach pain I’ve had” that steadily worsens over 6–24 hours.
- Children: Symptoms can be less specific (fever, vomiting, diffuse pain). Kids perforate more quickly; seek care early for persistent belly pain and fever.
- Older adults: Pain and fever may be milder, making diagnosis tricky. Confusion or a general decline may be the only clue. Risk of perforation is higher.
- Pregnancy: The appendix shifts upward as the uterus grows; pain may be higher in the abdomen. Nausea and vomiting can be mistaken for morning sickness. MRI or ultrasound is preferred for diagnosis.
Consult Top Specialists Here
Red Flags and When to Seek Urgent Care
Get urgent care now if you have severe or worsening abdominal pain (especially RLQ), fever, persistent vomiting, inability to pass gas with bloating, or pain with walking. These may indicate perforated appendicitis or another emergency.
If you’re unsure, start with a virtual triage. If symptoms persist beyond a day or are severe, consult a doctor online with Apollo 24|7 for further evaluation, or proceed directly to the emergency department.
What Causes Appendicitis?
Here’s what typically triggers appendicitis.
Common Triggers and What We Know
Most cases stem from a blockage at the opening of the appendix:
- Fecaliths (hardened stool) are common in adults.
- Lymphoid tissue swelling after a GI or viral infection (more common in children).
- Less commonly, parasitic infection or appendiceal tumours.
The blockage traps bacteria, causing swelling and pressure. Left untreated, this can progress to gangrene and perforation. While we don’t fully understand why certain people develop appendicitis, it’s not typically linked to diet or stress.
Risk Factors and Persistent Myths
- Age: Most common in teens and young adults but can occur at any age.
- Family history: Some familial clustering exists but isn’t strong enough for screening.
- Myths: Spicy food, chewing gum, or seeds are not proven causes.
- Seasonal/viral trends: Lymphoid hyperplasia after infections may explain seasonal variation, especially in children.
There’s no proven way to prevent appendicitis, but prompt recognition and care reduce complications.
How Doctors Diagnose Appendicitis
Here’s how healthcare professionals confirm appendicitis.
Physical Exam Signs
Clinicians check for RLQ tenderness, rebound (pain when pressure is released), guarding (muscle tensing), and specific signs such as:
- McBurney’s point tenderness (classically over the appendix)
- Rovsing sign (pain in RLQ when pressing on the left side)
- Psoas/obturator signs (pain with certain leg movements suggesting irritation)
- No single sign is definitive; findings guide the need for tests and imaging.
Blood and Urine Tests
- Blood: Elevated white blood cell count and C-reactive protein (CRP) support the diagnosis but aren’t specific.
- Urine: Rules out urinary tract infections or kidney stones that can mimic appendicitis.
- Pregnancy test: For people who can become pregnant, to guide imaging and rule out ectopic pregnancy.
If a clinician advises lab tests such as CBC or CRP but you’re stable at home, Apollo 24|7 offers convenient home collection. However, if you suspect appendicitis, prioritise urgent in-person evaluation over home testing.
Imaging: Ultrasound, CT, MRI
- Ultrasound: Preferred first-line in children and pregnancy; no radiation; operator-dependent. Looks for a noncompressible, enlarged appendix and surrounding changes.
- CT scan: Highly accurate in adults; quickly identifies complications like abscess or perforation. Uses radiation; contrast may be used.
- MRI: Useful in pregnancy and when radiation should be avoided.
Risk Scores: Alvarado and AIR
Clinicians sometimes use the Alvarado score or AIR (Appendicitis Inflammatory Response) score to estimate risk based on symptoms, signs, and labs. These tools help decide who can be observed, who needs imaging, and who needs surgery.
Treatment Options: Surgery vs Antibiotics
Here’s what treatment options are available and when each is preferred.
Appendectomy (Laparoscopic vs Open)
- Laparoscopic appendectomy is the standard in many centres: 3–4 small incisions, faster recovery, less pain, fewer wound complications, and a shorter hospital stay compared with open surgery.
- Open appendectomy is used when laparoscopy isn’t feasible or in certain complicated cases.
- Timing: Early surgery reduces risk of perforation. Perforated appendicitis may require drainage of abscesses and broader antibiotics.
Non-Operative Management with Antibiotics
- Evidence shows that some people with uncomplicated appendicitis can be treated with antibiotics:
The CODA trial (NEJM) found antibiotics were noninferior to surgery at 30 days for overall health status; however, about 29% underwent appendectomy within 90 days (higher if an appendicolith was present). - Cochrane reviews suggest antibiotics can avoid surgery initially in many, but recurrence or later surgery is more common than with upfront appendectomy.
- Advantages: No surgery, quicker initial recovery in select patients.
- Trade-offs: Risk of recurrence, need for close follow-up, and higher failure rate with an appendicolith.
Choosing an Approach That Fits You
Consider:
- Imaging findings: An appendicolith, abscess, or perforation typically pushes care toward surgery.
- Your values: Avoiding surgery vs accepting a small recurrence risk.
- Access: Ability to return promptly if symptoms recur.
- Work and recovery needs: Laparoscopy often allows faster return than open surgery.
If symptoms are escalating or you have a fever and severe RLQ pain, don’t delay. If your condition does not improve after initial advice or pain worsens, book a physical visit to a doctor with Apollo 24|7 or go to the emergency department.
What to Expect During and After Appendectomy
Here’s what happens before, during, and after surgery.
In the Hospital: Pain Control and Mobilisation
- Before surgery: You’ll receive antibiotics and IV fluids.
- During laparoscopic surgery: Typically 30–60 minutes.
- After surgery: Most people go home within 24–48 hours for uncomplicated cases. Early walking improves recovery and lowers clot risk.
- Pain control: Often a combination of paracetamol, NSAIDs, and short-term opioids if needed.
Recovery Timeline and Scar Care
- Days 1–3: Shoulder-tip pain (from laparoscopy gas) possible; walking helps. Small incisions are covered with dressings; keep dry as directed.
- Days 4–14: Energy returns; light activity is encouraged. Most resume desk work in 1–2 weeks.
- Weeks 3–6: Gradual return to full activity; avoid heavy lifting until cleared.
- Scars: Protect from sun; gentle silicone gel/sheets can improve appearance.
Eating, Moving, and Returning to Work or School
- Diet: Start with light meals and advance as tolerated. Hydration and fibre help prevent constipation.
- Movement: Short, frequent walks speed recovery.
- Work/school: Many return in 1–2 weeks after laparoscopic surgery; manual labour may require 3–4 weeks depending on your surgeon’s advice.
Complications and How They’re Managed
Here’s what complications can arise and how doctors manage them.
Perforation, Abscess, and Sepsis
- Perforation: Risk rises with delays. Signs include severe, spreading pain, high fever, and a very tender abdomen.
- Abscess: May be treated with percutaneous drainage plus antibiotics, followed by interval appendectomy in some cases.
- Sepsis: Requires urgent hospital care with IV antibiotics and fluids.
Negative Appendectomy and Missed Cases
- Negative appendectomy: Removal of a normal appendix. Rates have dropped with modern imaging but still occur.
- Missed cases: Appendicitis can mimic gastroenteritis, ovarian conditions, kidney stones, or Crohn’s disease. If pain localises to the RLQ or persists, seek reevaluation.
Appendicitis in Special Groups
Here’s how appendicitis differs in specific populations.
Children and Teens
Children can worsen quickly. Ultrasound is the preferred first test. If your child has persistent belly pain with fever or won’t jump/walk due to pain, seek urgent care.
Pregnancy
Use ultrasound first; MRI if unclear. Symptoms may be atypical due to the uterus shifting organs upward. Laparoscopic surgery is generally safe in pregnancy with appropriate precautions. Prompt diagnosis protects both parent and foetus.
Older Adults
Atypical symptoms and delayed presentations are common. CT is often needed for clarity. Complication rates are higher, so a low threshold for imaging and treatment is appropriate.
Preventing Delays: Practical Steps and Telehealth
Here’s how to avoid dangerous delays and use telehealth wisely.
Home Monitoring Tips (While Seeking Care)
- Do not self-treat severe RLQ pain with laxatives or painkillers that mask symptoms.
- Note pain onset, migration, fever, vomiting, and inability to pass gas.
- Keep fluids light; avoid solid food if surgery is likely.
If advised by a clinician, basic labs (CBC, CRP) can help, and Apollo 24|7 offers home collection—but acute severe abdominal pain warrants an ER visit.
When to Use an Online Consult (Apollo 24|7)
- Good for early triage, clarifying symptoms, and arranging imaging or labs.
- If symptoms persist beyond two weeks (for chronic/recurrent RLQ pain) or you have non-urgent questions post-recovery, consult a doctor online with Apollo 24|7 for further evaluation.
- For sudden, severe, or localised RLQ pain, fever, or vomiting, go to the emergency department.
Cost, Access, and Questions to Ask Your Surgeon
Here’s how to prepare financially and what to ask before treatment.
Questions to Ask About Surgery or Antibiotics
- Is my appendicitis uncomplicated or complicated?
- Do I have an appendicolith?
- Am I a candidate for antibiotics first? What’s my recurrence risk?
- How many laparoscopic appendectomies does your team perform yearly?
- What’s the plan if symptoms worsen?
Understanding Bills, Insurance, and Recovery Leave
- Ask about facility fees, surgeon and anaesthesia fees, imaging, and labs.
- Clarify expected length of stay and time off work or school.
- If cost is a concern, discuss non-urgent imaging choice (ultrasound vs CT) when clinically appropriate and local options for outpatient follow-up.
Myths, FAQs, and Trustworthy Resources
- Myth: “If the pain comes and goes, it’s not appendicitis.”
Reality: Pain can wax and wane early, then localise and worsen. - Myth: “Appendicitis always causes high fever.”
Reality: Fever can be mild or absent early.
Trusted resources: Major hospitals, national health services, and peer-reviewed reviews.
Conclusion
Appendicitis is common, urgent, and—when recognised early—very treatable. The classic symptom pattern starts as vague central abdominal discomfort that migrates to the right lower quadrant, often with nausea, loss of appetite, and low-grade fever. Diagnosis combines a careful exam with targeted tests and imaging to confirm appendicitis and assess for complications.
Treatment has advanced: while laparoscopic appendectomy remains the go-to for many, antibiotics alone can be appropriate for select uncomplicated cases. The safest path is guided by your clinical picture, imaging, and preferences.
If you’re experiencing severe or worsening abdominal pain—especially in the right lower abdomen—seek urgent care now. For questions about your symptoms, results, or recovery plan, you can consult a doctor online with Apollo 24|7; if a clinician recommends labs, Apollo 24|7 offers home collection for tests like CBC or CRP. Above all, don’t delay: timely decisions reduce complications, shorten recovery, and improve outcomes.
Consult Top Specialists Here
Consult Top Specialists Here

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)
Dr. Thandra Ramoji Babu
General Physician/ Internal Medicine Specialist
5 Years • MBBS, DNB(General Medicine)
Warangal
Sai Ram multi-specialty hospital, Warangal
Consult Top Specialists Here

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)
Dr. Thandra Ramoji Babu
General Physician/ Internal Medicine Specialist
5 Years • MBBS, DNB(General Medicine)
Warangal
Sai Ram multi-specialty hospital, Warangal
More articles from Appendicitis
Frequently Asked Questions
Can appendicitis go away on its own?
True appendicitis usually progresses without treatment and can perforate. Some mild cases may temporarily improve, but recurrence is likely. Seek medical evaluation promptly.
How do doctors confirm appendicitis without CT?
Ultrasound can diagnose many cases, especially in children and pregnancy; MRI is an option when radiation should be avoided. Blood tests and clinical scores also guide decisions.
Is appendicitis treatment without surgery safe?
For uncomplicated cases, antibiotics can work short-term; however, recurrence or later surgery is more common than with immediate appendectomy.
How long is recovery after laparoscopic appendectomy?
Many people return to desk work in 1–2 weeks and full activity by 3–6 weeks. Recovery is typically faster than with open surgery.
What if my pain seems like gas or food poisoning?
Early appendicitis can mimic gastroenteritis or gas. Worsening pain that localises to the right lower quadrant, fever, or pain with movement strongly suggests appendicitis.


.webp)
