Guide to Bone Marrow Failure Syndrome
Bone marrow failure syndrome occurs when the bone marrow cannot produce enough healthy blood cells. This guide explains causes, symptoms, diagnosis, treatment options, and long-term care. Learn how specialists evaluate and manage this complex group of disorders.

Written by Dr. Mohammed Kamran
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
Bone marrow failure syndrome may sound daunting, but understanding the mechanisms, warning signs, and treatment pathways can provide clarity and reassurance. Bone marrow is the soft, spongy tissue inside bones responsible for producing red blood cells, white blood cells, and platelets. When it cannot produce adequate quantities of these essential cells, the result is bone marrow failure syndrome. Individuals may experience fatigue, recurrent infections, or easy bleeding.
This guide explains what bone marrow failure syndrome is, who may be affected, how doctors diagnose it, and current therapeutic approaches—from supportive measures to stem cell transplantation. It also includes considerations for daily living, when to seek urgent support, and how to communicate effectively with healthcare teams. If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for timely evaluation.
What Is Bone Marrow Failure Syndrome?
This section describes what happens when the marrow cannot generate sufficient blood cells.
A simple definition
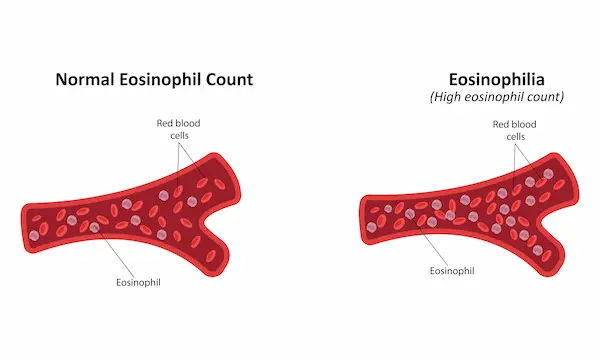
Bone marrow failure syndrome arises when the marrow fails to produce adequate numbers of red cells, white cells, and platelets. When all three cell lines are reduced, this leads to pancytopenia. Low red cells cause fatigue, poor exercise tolerance, and shortness of breath. Low white cells weaken the immune defence. Low platelets increase bleeding and bruising.
In some cases, marrow becomes hypocellular, with few active cells, as in aplastic anaemia. In others, the marrow may
contain cells that are abnormal or dysplastic, as seen in myelodysplastic syndromes (MDS).
Consult a Top General Practitioner for Personalised Advice
Types: acquired vs inherited
• Acquired bone marrow failure is more common in adults. Aplastic anaemia often results from immune-mediated damage to stem cells. Triggers may include toxins, certain medicines, viral illnesses, or pregnancy, although many cases have no identifiable cause.
• Inherited bone marrow failure syndromes (IBMFS) typically present in childhood or young adulthood, such as Fanconi anaemia, Diamond-Blackfan anaemia, Shwachman-Diamond syndrome, and dyskeratosis congenita. These conditions may involve other organs and increase the risk of malignancies.
Related conditions you may hear about
• Paroxysmal nocturnal haemoglobinuria (PNH): Can occur alongside aplastic anaemia and is marked by haemolysis and clotting risks.
• MDS: Characterised by dysplastic marrow cells and a risk of progression to acute myeloid leukaemia (AML).
Clarifying the exact subtype guides treatment strategy and determines whether family screening is needed.
Signs and Symptoms You Shouldn’t Ignore
This section highlights clinical features requiring proactive assessment.
Early symptoms and red flags
Symptoms often develop gradually and may include:
- Fatigue, pallor, headaches, shortness of breath
- Frequent infections and fevers
- Easy bruising, gum or nose bleeding, menstrual heavy flow
- Dizziness or rapid heart rate in severe anaemia
Urgent symptoms requiring immediate care:
High fever, severe breathlessness, uncontrolled bleeding, chest pain, or confusion.
Special considerations in children and pregnancy
Children may show short stature, limb or thumb anomalies, skin pigment changes, nail abnormalities, or developmental
differences, indicating inherited syndromes.Pregnancy may exacerbate pancytopenia or reveal new marrow failure. Management requires coordination between high-risk obstetrics and haematology. Transfusion support may be necessary.
Maintaining a symptoms diary can help measure change over time. For persistent symptoms, consult a doctor online
with Apollo24|7.
Causes and Risk Factors
This section summarises immune, environmental, and genetic contributors.
Acquired causes: immune, toxins, infections
• Immune-mediated aplastic anaemia: T-cells attack stem cells, reducing marrow cellularity, which is why
immunosuppressive therapy can improve counts.
• Toxins/medications: Benzene, industrial solvents, chemotherapy, and radiation may trigger marrow suppression.
• Infections: Viral illnesses such as hepatitis viruses, EBV, HIV, or parvovirus B19 may precede marrow failure.
Inherited syndromes and genetics
• Fanconi anaemia: Associated with skeletal abnormalities and cancer risk.
• Dyskeratosis congenita/short telomere disorders: Characterised by mucocutaneous changes and potential lung or
liver involvement.
• Diamond-Blackfan anaemia: Affects red cell production in infancy or early childhood.
Environmental exposures and medication triggers
Avoidable hazards include benzene exposure and high-dose radiation. Medication evaluation and adjustment may
prevent worsening cytopenias.
In adults presumed to have acquired disease, hidden telomere disorders remain possible—clinical history helps detect
subtle genetic causes.
How Doctors Diagnose Bone Marrow Failure Syndrome
This section explains diagnostic tools used to confirm the condition.
Blood tests and what they show
A complete blood count (CBC) identifies the extent of cytopenias. Reticulocyte count indicates whether the marrow is
responding. Iron studies, vitamin B12, folate levels, and organ function tests help rule out nutritional or metabolic
causes.
Apollo24|7 offers convenient home collection for these investigations.
Bone marrow biopsy and specialised testing
Bone marrow aspirate and biopsy provide definitive assessment.
- Aplastic anaemia: Hypocellular marrow without significant dysplasia
- MDS: Normal or increased marrow cellularity with abnormal cell morphology
Cytogenetic and molecular studies help estimate prognosis and guide treatment decisions.
When to consider genetic and viral testing
Genetic analysis is important where onset is early, physical anomalies exist, or family history suggests inherited risk.
PNH testing via flow cytometry may be necessary due to overlap risks. Viral testing is ordered based on clinical
suspicion.
Second-opinion review at a specialist centre ensures precise classification before major treatment choices are made.
Treatment Options That Work Today
This section outlines therapies tailored to severity and cause.
Supportive care
• Transfusions: Correct severe anaemia or thrombocytopenia; long-term transfusion may cause iron overload requiring
chelation therapy.
• Infection control: Rapid treatment of fever; preventative antibiotics or antifungals in selected cases; cautious use of
growth factors.
• Lifestyle adjustments: Avoid contact sports and medicines that increase bleeding.
Immunosuppressive therapy
Standard therapy combines antithymocyte globulin (ATG) and cyclosporine. Many patients achieve a durable response,
although relapse or clonal evolution may occur over time. Eltrombopag, a thrombopoietin-receptor agonist, can enhance responses and accelerate recovery in severe aplastic
anaemia.
Stem cell transplantation (HSCT)
Allogeneic HSCT remains the curative approach for many young patients with a matched sibling donor. Alternative donors may be considered when necessary.Risks include graft-versus-host disease, infection, and fertility complications; fertility preservation discussions should
occur beforehand.
Approaches for MDS and telomere-related conditions
Treatment depends on disease behaviour and genetic markers. Options may include growth-stimulating medicines,
hypomethylating agents, or HSCT. Reduced-intensity procedures may limit toxicity in telomere disorders.
Enquiring about clinical trial eligibility may provide access to innovative treatments.
Living Well With Bone Marrow Failure Syndrome
This section supports daily management and long-term well-being.
Infection prevention and bleeding precautions
Hand hygiene, safe food practices, and vaccination guidance help reduce infection risk. Bleeding precautions include avoiding high-risk activities and using soft oral care products.
Nutrition, fitness, vaccinations, mental well-being
A balanced diet with adequate protein supports recovery. Exercise—guided by platelet counts—can reduce fatigue and
improve mood. Mental health support through counselling or peer groups may strengthen resilience.
Managing iron overload and long-term monitoring
Long-term transfusions may lead to iron overload requiring chelation. Regular monitoring with blood tests and
occasional marrow assessments helps detect relapse or clonal changes early.
Keeping detailed records of transfusions and test results improves continuity of care.
Outlook, Complications, and When to Seek Care
This section explains long-term expectations and monitoring needs.
Clonal evolution and relapse
Some patients may develop PNH clones or progress to MDS or AML over time. Others may relapse after
immunosuppressive therapy, requiring re-treatment or consideration of HSCT.
Prognosis and quality of life
Outcomes depend on age, disease severity, donor availability, genetic findings, and treatment response. With modern
care, many individuals return to education, employment, and active lifestyles.
When to see a specialist and urgent warning signs
Persistent unexplained fatigue, repeated infections, or abnormal bleeding warrant prompt haematology evaluation.
Emergency signs include high fever, breathlessness, chest pain, and uncontrolled haemorrhage.
If your condition does not improve, consult a doctor online with Apollo24|7 or arrange a specialist review.
Conclusion
Bone marrow failure syndrome describes a group of conditions with insufficient production of healthy blood cells. Aplastic anaemia remains the most common acquired subtype and often responds well to immunosuppressive therapy. Stem cell transplantation is a curative option for many eligible patients, particularly younger individuals with a matched donor. Inherited syndromes require precise diagnosis and genetic guidance.
Daily preventive strategies—such as hand hygiene, bleeding precautions, nutritional support, and mental health care—are equally important in maintaining quality of life. If symptoms continue for more than two weeks or if treatment decisions feel unclear, speak to a doctor online with Apollo 24|7 to review investigations and treatment planning. With the right expertise and timely care, individuals can move confidently towards recovery and long-term stability.
Consult a Top General Practitioner for Personalised Advice
Consult a Top General Practitioner for Personalised Advice

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Suseela
General Physician
5 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Suvadeep Sen
Critical Care Specialist
12 Years • MBBS, MD, FNB (CRITICAL CARE MEDICINE), EDIC
Mumbai
Apollo Hospitals CBD Belapur, Mumbai

Dr. Ishita Mandal
General Surgeon
7 Years • MBBS(hons.), MS(general surgery), General and laparoscopic surgeon
Kolkata
VDC Clinic, Kolkata

Dr. Dilip Joseph Wilson
General Physician/ Internal Medicine Specialist
30 Years • MBBS, DT M&H, DFFP, DIP.IIST
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
Consult a Top General Practitioner for Personalised Advice

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Suseela
General Physician
5 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Suvadeep Sen
Critical Care Specialist
12 Years • MBBS, MD, FNB (CRITICAL CARE MEDICINE), EDIC
Mumbai
Apollo Hospitals CBD Belapur, Mumbai

Dr. Ishita Mandal
General Surgeon
7 Years • MBBS(hons.), MS(general surgery), General and laparoscopic surgeon
Kolkata
VDC Clinic, Kolkata

Dr. Dilip Joseph Wilson
General Physician/ Internal Medicine Specialist
30 Years • MBBS, DT M&H, DFFP, DIP.IIST
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
More articles from Blood Disorders
Frequently Asked Questions
Q1. Is bone marrow failure syndrome the same as aplastic anaemia?
Aplastic anaemia is one form of bone marrow failure characterised by hypocellularity and pancytopenia, but other disorders such as MDS also fall within this category.
Q2. How is bone marrow failure diagnosed?
Doctors begin with a CBC and reticulocyte count, followed by a bone marrow biopsy and genetic or molecular testing. Apollo24|7 provides home sample collection for essential laboratory tests.
Q3. What is the success rate of treatment?
Immunosuppressive therapy is effective for many patients, while HSCT offers cure in selected individuals. Outcomes depend on multiple clinical factors.
Q4. Can children outgrow bone marrow failure?
Inherited causes do not typically resolve spontaneously, but appropriate treatment can achieve long-term stability and good quality of life.
Q5. What lifestyle changes help with bone marrow failure syndrome?
Infection prevention, bleeding precautions, balanced nutrition, and monitoring of blood counts support overall health.