Guide to Brain Injuries Do Not Discriminate
Understand the universal impact of brain injuries (TBI), recognizing that they affect people of all ages, backgrounds, and walks of life. Learn about causes, recovery, and support systems.


Introduction
Brain injuries can affect anyone, anywhere—on the road, at work, on the field, or at home. They don’t discriminate by age, income, or background. Whether you’re a parent, a coach, a commuter, or a caregiver, understanding brain injuries can help you recognize problems early, seek the right care, and support recovery. In this guide, we’ll explain what brain injuries are, how they happen, and the signs you should never ignore. You’ll learn how doctors diagnose injuries, what treatments and rehabilitation look like, and how to safely return to school, work, or sport. We’ll also cover prevention strategies that really work and highlight underrecognized groups—like survivors of domestic violence—who often go unseen. Along the way, we’ll share practical tips, evidence-based insights, and clear steps you can take right now. Because brain injuries do not discriminate, this guide is for everyone.
What We Mean by “Brain Injuries”
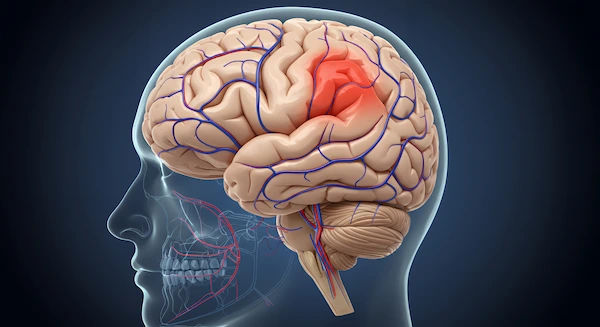
Brain injuries fall into two broad categories. Traumatic brain injury (TBI) happens when an external force—such as a fall, car crash, sports collision, or assault—disrupts normal brain function. Acquired brain injury (ABI) refers to brain damage that occurs after birth from internal causes like stroke, brain tumors, infections (meningitis, encephalitis), oxygen deprivation (near-drowning, cardiac arrest), or toxic exposures. Many people use “brain injuries” to refer to TBI specifically, but both TBI and ABI can cause short- and long-term problems with thinking, memory, mood, sleep, and physical function. [1][2][3]
Clinicians classify TBI as mild, moderate, or severe—often using the Glasgow Coma Scale (GCS) at the time of injury. Mild TBI, commonly called concussion, is by far the most common. Most people with mild TBI recover within weeks, but a significant minority experience prolonged symptoms (post-concussion syndrome). Moderate and severe TBIs are often visible on CT or MRI and can involve bleeding, bruising, swelling, or diffuse axonal injury (microscopic damage to nerve fibers), with a longer and more complex recovery. [3][5][7]
• Here’s an important nuance: the invisible injury. You can have a concussion with a normal CT or MRI. Conventional imaging isn’t sensitive to microscopic or functional changes; that’s why symptoms such as cognitive fatigue, light sensitivity, or dizziness are real even when scans look “normal.” Long-tail keywords naturally included: Glasgow Coma Scale explained; diffuse axonal injury prognosis.
Why Brain Injuries Do Not Discriminate?
The global burden of brain injuries is massive. Estimates suggest tens of millions of TBIs occur worldwide each year—about 69 million annually—making TBI a major cause of death and disability across all regions. In the United States alone, there were approximately 223,000 TBI-related hospitalizations and about 64,000 deaths in 2020; many more people are treated in emergency departments and released. Falls are the leading cause overall, particularly among older adults and young children, while road traffic crashes are a dominant cause in many low- and middle-income countries. [1][2]
Brain injuries do not discriminate—but their effects are not evenly distributed. Social determinants of health influence risk, recognition, and recovery. People in rural areas may live farther from trauma centers. Those with limited resources may lack access to rehabilitation or time off from work. Women, especially survivors of intimate partner violence, experience head injuries that often go unrecognized or underreported. Migrant and informal workers may face higher occupational risks. Students and athletes from underserved schools may have less access to athletic trainers and standardized concussion protocols. Older adults, who are more likely to fall, often have co-morbidities and take medicines that increase bleeding risk, complicating recovery. By acknowledging these inequities, we can tailor prevention, screening, and support to those who need it most. [1][2][8]
Unique insight: Simple changes—like adding a one-question domestic violence head injury screening in urgent care or attaching fall-risk checklists to home care visits—can close real gaps in recognition and care.Consult a Top Neurologist
Causes Across Life Stages and Settings
Falls are the top cause of brain injuries globally and in high-income countries, especially among older adults and toddlers. Most fall-related TBIs happen at home: slipping in bathrooms, tripping on rugs, or falling from ladders. Road traffic injuries—motorcyclists, bicyclists, pedestrians, and occupants—are a leading cause of moderate to severe TBI, particularly in regions with rapid urbanization and limited helmet use. Seatbelts, child restraints, and quality roads save lives; so do speed management and drink–driving enforcement. [1][2]
Sports and recreation contribute to many mild TBIs. Contact sports (football, rugby), ice hockey, soccer (heading), and combat sports carry notable risk. Helmets reduce risk in cycling, skating, and skiing but cannot prevent all concussions. Domestic and community violence, including intimate partner violence, is an underrecognized cause across ages and genders—one where injuries are often repeated and unreported. Workplace TBIs occur in construction, mining, agriculture, and manufacturing, often involving falls from height or struck-by incidents. Military service members face blast-related TBIs from explosions; symptoms may overlap with PTSD, complicating diagnosis and rehabilitation. [3][5][8]
• Special scenarios: At home, toddlers may fall from furniture or stairs; always use gates and window guards. In older adults, vision problems, neuropathy, and medications increase fall risk; a home safety audit plus strength and balance exercises can substantially reduce falls. Long-tail keywords incorporated: preventing falls in older adults at home; blast-related TBI in veterans.
Warning Signs You Should Never Ignore
Not all head bumps cause brain injury. But certain red flags need urgent medical evaluation, ideally in an emergency department:
• Worsening headache, repeated vomiting, or seizures
• Slurred speech, weakness or numbness on one side, trouble walking, severe dizziness
• Unequal pupils, vision changes, confusion that worsens, agitation, or unusual behavior
• Loss of consciousness, persistent drowsiness, inability to awaken
• Clear fluid from the nose or ears, or a depressed skull fracture
• For infants/children: inconsolable crying, refusal to eat, bulging fontanelle, or any concerning change in behavior [1][4]
Common mild symptoms that usually improve over days to weeks include headache, feeling “foggy,” light/noise sensitivity, sleep disturbances, and mood changes. Children may be clingier or have trouble concentrating. Older adults may present subtly—confusion, balance issues, or a change from baseline—especially if they’re on blood thinners.
You can sleep after a concussion if you’ve been medically assessed and cleared, but someone should check on you periodically in the first 24 hours. If symptoms persist beyond two weeks—or you notice new or worsening problems—consult a doctor online with Apollo 24|7 for further evaluation. Early medical guidance can prevent complications and accelerate recovery. Long-tail keywords included: signs of concussion in adults; second impact syndrome risk.
How Brain Injuries Are Diagnosed
Clinicians start with history (what happened, speed/height, loss of consciousness, amnesia, current symptoms) and a neurological exam. The Glasgow Coma Scale (GCS) rates eye, verbal, and motor responses to grade injury severity. In suspected moderate or severe TBI—or if red flags are present—head CT is the first-line imaging to detect bleeding, fractures, or swelling. MRI can reveal subtle injuries (e.g., diffuse axonal injury), small contusions, or shearing not visible on CT. Many concussions have normal imaging; diagnosis remains clinical. [3][5][7]
Blood biomarkers are an emerging tool. For example, GFAP and UCH-L1 (in some settings) can help determine the need for CT in adults with mild TBI, potentially reducing unnecessary scans. These tests are not yet universally available but show promise. Neuropsychological tests assess attention, memory, processing speed, and executive function; vestibular and oculomotor testing can reveal treatable causes of dizziness and visual strain. In sports, standardized tools (e.g., SCAT, updated periodically) support sideline and clinic evaluations. [7]
If you’re on anticoagulants, have a bleeding disorder, or are over 65, clinicians may favor a lower threshold to image and observe. Keep a list of your medications handy. If lab tests are recommended to investigate factors that raise fall risk (e.g., vitamin D), Apollo 24|7 offers a convenient home collection for tests like vitamin D or HbA1c.
Long-tail keywords included: CT scan vs MRI for head injury; Glasgow Coma Scale explained.
Treatment and Rehabilitation
Acute care focuses on stabilizing airway, breathing, and circulation; preventing secondary brain injury; and managing complications like bleeding or elevated intracranial pressure. Severe cases may require neurosurgery (e.g., hematoma evacuation) and ICU care with careful monitoring. For mild TBI, initial management includes 24–48 hours of relative rest—reducing cognitive and physical exertion, limiting screen time—followed by a gradual return to activity guided by symptoms. Prolonged strict rest is not recommended; graded activity promotes recovery. [3][4][5]
Rehabilitation is where recovery unfolds. A multidisciplinary team can include physiatrists, physical and occupational therapists, speech-language pathologists, neuropsychologists, social workers, and mental health professionals. Targeted therapies address:
• Headaches: hydration, sleep hygiene, limited analgesics, preventive medications when needed
• Dizziness and balance: vestibular therapy for concussion dizziness
• Vision problems: oculomotor and vision therapy
• Cognitive challenges: structured cognitive rehabilitation and pacing
• Mood and sleep: cognitive behavioral therapy, mindfulness, and sleep consolidation
• Return to driving: cognitive and on-road assessments, local regulations
Unique insight: Pair “energy accounting” with a daily symptom budget—plan your highest-demand tasks for times you feel strongest and schedule “micro-rests” before, not after, you hit the wall. Long-tail keywords included: post-concussion syndrome treatment; traumatic brain injury rehabilitation exercises.
If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7 to update your plan and consider referrals to specialized rehabilitation.
Life After Injury: Returning to School, Work, and Sport
Returning too quickly can worsen symptoms; waiting too long can delay recovery. Aim for a step-wise return individualized to your symptoms and job or school demands.
School:
• Start with partial days or reduced workload.
• Use accommodations: extra time on tests, note-taking support, reduced homework volume, screen breaks, sunglasses or tinted overlays for light sensitivity.
• Reassess weekly and ramp up gradually.
Work:
Begin with reduced hours or remote work if possible.
• Adjust lighting, noise, and screen time; take brief scheduled breaks.
• Prioritize tasks requiring deep concentration early in the day; use checklists and timers.
Sport:
• Follow a return to play protocol after head injury: no same-day return, then progress through light aerobic activity, sport-specific exercise, non-contact practice, full-contact practice, and game play—advancing a step every 24 hours if symptoms do not worsen. Seek medical clearance before contact. Second impact syndrome, while rare, can be catastrophic; don’t rush. [1][4]
Managing persistent symptoms:
• Headaches: consider a headache diary to identify triggers.
• Sleep: consistent schedule, limit naps to under 30 minutes, reduce caffeine late in day.
• Mood: screen for anxiety, depression, PTSD; ask for counseling early.
• Cognitive fatigue: chunk tasks, use “3-30-3” (3 minutes plan, 30 minutes work, 3 minutes rest).
If symptoms persist beyond two weeks (or four weeks in children), consult a doctor online with Apollo 24|7 for further evaluation, therapy referrals, and documentation for accommodations.
Prevention That Works for Everyone
Many brain injuries are preventable with common-sense measures that fit your life and budget.
Home and community:
• Preventing falls in older adults at home: remove loose rugs, install grab bars and bright lighting, use non-slip mats, organize frequently used items within easy reach, and wear well-fitted footwear.
• Strength and balance: exercises like tai chi and supervised strength training reduce falls.
• Vision and hearing checks: correct impairments that increase fall risk.
• Review medications: some increase dizziness or bleeding risk—ask your doctor to reassess.
On the road:
• Wear seatbelts every trip; ensure proper child restraints.
• Always wear a helmet when biking, skating, or riding a motorcycle.
• Avoid alcohol and distracted driving; respect speed limits.
Sports and recreation:
• Helmets reduce severe injuries but don’t prevent all concussions—play smart.
• Learn and enforce concussion protocols; when in doubt, sit them out.
• Educate players, parents, and coaches about the signs of concussion.
Violence and workplace:
• Promote domestic violence screening in clinics and schools; know local hotlines and shelters.
• In higher-risk jobs, use fall protection, guardrails, and lockout/tagout procedures; report near-misses to fix hazards.
Policy-level wins—like safer road design, speed calming, and helmet and seatbelt laws—deliver big population benefits. Community groups, schools, employers, and families all have a role.
Conclusion
Brain injuries do not discriminate, but informed action can make all the difference. Understanding what brain injuries are, how they happen, and which warning signs signal urgent care helps you protect yourself and those you love. Most people with mild injuries recover well with early rest, gradual activity, and targeted rehabilitation when needed. More serious injuries require coordinated acute care and a team-based rehabilitation plan that supports physical, cognitive, and emotional recovery. Across all severities, small, consistent steps—like pacing your day, tracking triggers, and practicing balance and strength—add up.
Equity matters, too. By recognizing who gets missed—older adults at home, survivors of intimate partner violence, rural residents, workers at height—we can bring screening, prevention, and support to where it’s needed most. Community measures like helmet and seatbelt use, safer road design, and fall-proof homes protect everyone.
If you or someone you care for has persistent symptoms—headaches, dizziness, sleep problems, or cognitive fatigue—don’t wait. Consult a doctor online with Apollo 24|7 for guidance, referrals, and documentation for school or work accommodations. And if your clinician recommends lab checks that affect fall risk and recovery (e.g., vitamin D), Apollo 24|7 offers home collection to keep your care on track. Recovery is a journey; you don’t have to walk it alone.Consult a Top Neurologist
Consult a Top Neurologist

Dr. Dipti Ranjan Tripathy
Neurologist
15 Years • MBBS, MD (GENERAL MEDICINE ),DM (NEUROLOGY)
Rourkela
Apollo Hospitals, Rourkela, Rourkela
(25+ Patients)

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Rajendra Prasad
Spine Surgeon
36 Years • MBBS. FRCS (Glas) U.K FRCS (Neurosurgery) Intercollegiate Specialty Board in Neurosurgery (U.K). Fellowship in Spine Surgery, Stanmore, London U.K. Specialist Registration in Neurosurgery with General Medical Council. U.K
Delhi
Apollo Hospitals Indraprastha, Delhi
Dr. J C Rasmi Reddy
Neurologist
5 Years • M.B.B.S, M.D, DrNb in Neurology
Nellore
Apollo Speciality Hospitals, Nellore
Consult a Top Neurologist

Dr. Dipti Ranjan Tripathy
Neurologist
15 Years • MBBS, MD (GENERAL MEDICINE ),DM (NEUROLOGY)
Rourkela
Apollo Hospitals, Rourkela, Rourkela
(25+ Patients)

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Rajendra Prasad
Spine Surgeon
36 Years • MBBS. FRCS (Glas) U.K FRCS (Neurosurgery) Intercollegiate Specialty Board in Neurosurgery (U.K). Fellowship in Spine Surgery, Stanmore, London U.K. Specialist Registration in Neurosurgery with General Medical Council. U.K
Delhi
Apollo Hospitals Indraprastha, Delhi
Dr. J C Rasmi Reddy
Neurologist
5 Years • M.B.B.S, M.D, DrNb in Neurology
Nellore
Apollo Speciality Hospitals, Nellore
More articles from Brain Injury
Frequently Asked Questions
1) Is a concussion the same as a traumatic brain injury?
Yes. A concussion is a mild traumatic brain injury (mTBI). Symptoms can include headache, dizziness, and trouble concentrating. Even with a normal scan, mTBI is real and needs proper rest and a graded return to activity.
2) How long do concussion symptoms last?
Many people improve within 2–4 weeks. If symptoms persist beyond two weeks (adults) or four weeks (children), consult a doctor online with Apollo 24|7 to assess for post-concussion syndrome and adjust your recovery plan.
3) Do I need a CT or MRI after a head injury?
Not always. Imaging is based on red flags, age, mechanism, and risk factors (e.g., blood thinners). CT is first-line for suspected bleeding; MRI can detect subtle injuries. Ask your clinician which is right for you.
4) Is it safe to sleep after a head injury?
After medical assessment, it’s generally safe to sleep. Have someone check on you periodically in the first 24 hours and seek care if symptoms worsen or new red flags appear.
5) Which tests might help reduce my risk of future falls?
Your clinician may recommend vision and hearing checks and labs like vitamin D or HbA1c (for diabetes). Apollo 24|7 offers a convenient home collection for these tests so you can act on results quickly.