Guide to Brain Attack Or Stroke Emergency
Know what a brain attack, haemorrhagic attack, is, and life after a brain attack. Learn about signs, diagnosis and treatment options for a brain attack.

Introduction
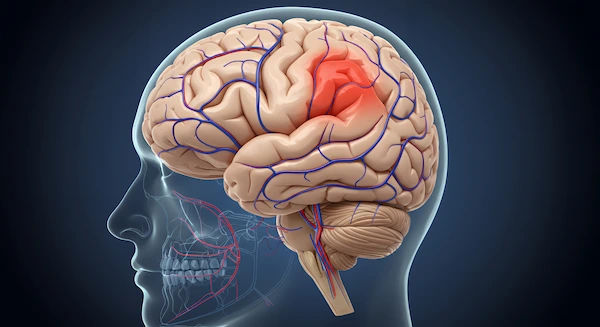
A brain attack, more commonly known as a stroke, is a medical crisis that strikes with terrifying speed. It occurs when the vital blood supply to a part of your brain is interrupted or severely reduced, depriving brain tissue of oxygen and nutrients. Within minutes, brain cells begin to die. This is why a stroke is a true emergency where every minute matters. Understanding what a stroke is, how to spot its signs, and knowing the immediate steps to take can mean the difference between life and death, or between a full recovery and permanent disability. This guide will walk you through everything you need to know, from recognising the earliest warning signs to navigating the path of recovery and prevention. Your quick thinking could save a life, perhaps even your own.
What is a Brain Attack? Understanding Stroke
A stroke, or cerebrovascular accident (CVA), is aptly named a "brain attack" because it shares the same urgency as a
heart attack. It's a sudden injury to the brain caused by a problem with blood flow. To function correctly, your brain needs a constant supply of oxygen-rich blood. When this supply is cut off, the affected brain tissue can't get the oxygen it needs, and cells start to perish. The effects of a stroke depend on which part of the brain is damaged and how much tissue is affected, potentially impacting movement, speech, memory, and more.
Ischemic Stroke: The Blocked Artery
This is the most common type of stroke, accounting for about 87% of all cases. An ischemic stroke happens when a blood clot blocks or plugs an artery leading to the brain. The clot can form directly in the artery (thrombotic stroke) or travel from elsewhere in the body, such as the heart, and lodge in a narrower brain artery (embolic stroke). The underlying cause is often atherosclerosis—a buildup of fatty deposits (plaque) that narrows the arteries.
Consult a Top Neurologist for Personalised Advice
Hemorrhagic Stroke: The Burst Blood Vessel
A hemorrhagic stroke occurs when a weakened blood vessel in the brain ruptures and bleeds into the surrounding tissue. The accumulated blood compresses brain cells, damaging them. High blood pressure (hypertension) is the leading cause of this type of stroke, as it can weaken artery walls over time. Aneurysms (ballooning of a blood vessel) are another common cause.
Transient Ischemic Attack (TIA): The Warning Stroke
Often called a "mini-stroke," a Transient Ischemic Attack (TIA) is caused by a temporary clot. The symptoms are
identical to those of a full-blown stroke but typically last only a few minutes to an hour and leave no permanent
damage. However, a TIA is a critical warning sign. It indicates a high risk of a major stroke in the near future and
should never be ignored. Approximately 1 in 3 people who have a TIA will later have a stroke, with about half
occurring within a year after the TIA.
Recognising a Brain Attack: Don't Ignore the Signs
Time is brain. The faster a stroke is recognised and treated, the better the chances of recovery. Symptoms usually appear
suddenly and without warning.
The F.A.S.T. Acronym: A Lifesaving Tool
The American Stroke Association promotes the F.A.S.T. acronym as an easy-to-remember tool for identifying common
stroke symptoms:
* F - Face Drooping: Does one side of the face droop or is it numb? Ask the person to smile. Is the smile uneven?
* A - Arm Weakness: Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
* S - Speech Difficulty: Is speech slurred or strange? Ask the person to repeat a simple sentence. Are the words difficult to understand?
* T - Time to Call Emergency Services: If you observe any of these signs, even if they disappear, call your local
emergency number immediately. Note the time when the symptoms first appeared.
Beyond F.A.S.T.: Other Crucial Stroke Symptoms
While F.A.S.T. covers the major signs, a brain attack can cause other sudden symptoms, which may occur alone or in combination:
* Sudden numbness or weakness in the leg, face, or especially on one side of the body.
* Sudden confusion, trouble understanding speech, or difficulty speaking.
* Sudden trouble seeing in one or both eyes.
* Sudden trouble walking, dizziness, loss of balance, or lack of coordination.
* Sudden severe headache with no known cause, often described as "the worst headache of my life."
What to Do During a Stroke Emergency: Every Second Counts
If you suspect someone is having a stroke, your response must be immediate and decisive. Panic is natural, but focused
action is what saves lives.
The Single Most Important Action: Call Emergency Services
Do not drive the person to the hospital yourself. Call an ambulance immediately. Paramedics are trained to begin life-
saving treatment on the way to the hospital. They can also alert the hospital, ensuring the stroke team is ready upon
arrival, which shaves critical minutes off the diagnosis time. When you call, be prepared to state the time the symptoms
started and describe them clearly.
What NOT to Do While Waiting for Help
While waiting for emergency services:
* Do NOT give the person any food, drink, or medication. A stroke can impair swallowing, leading to choking.
* Do NOT let the person go to sleep or talk you out of calling for help, especially if symptoms seem to fade (as with a TIA).
* Do note the time of symptom onset. This is crucial information for doctors.
* Do keep the person comfortable, lying on their side with their head slightly elevated if they are conscious. This position can help protect the airway if they vomit.
What Happens at the Hospital? Diagnosis and Immediate Treatment
Upon arrival at a certified stroke centre, the medical team moves quickly to confirm the diagnosis and determine the
type of stroke.
Rapid Diagnosis: CT Scans and MRIs
A brain scan, typically a CT (computed tomography) scan, is one of the first tests performed. It can quickly distinguish
between an ischemic stroke and a hemorrhagic stroke—a vital distinction because the treatment for one can be harmful
for the other. An MRI (magnetic resonance imaging) may provide more detailed images later.
Clot-Busting Drugs (tPA) and Mechanical Thrombectomy
For an ischemic stroke, the goal is to restore blood flow rapidly.
* tPA (Tissue Plasminogen Activator): This is a "clot-busting" drug that can dissolve the clot causing the stroke. It is most effective if administered within 3 to 4.5 hours of the onset of symptoms.
* Mechanical Thrombectomy: For larger clots, doctors may perform a procedure where a catheter is threaded through an artery to physically remove the clot. This procedure can be effective up to 24 hours after symptom onset in some eligible patients.
For a hemorrhagic stroke, treatment focuses on controlling the bleeding and reducing pressure on the brain, which may involve medication or surgery.
Life After a Stroke: The Road to Recovery
Recovery is a marathon, not a sprint. It begins in the hospital and continues with long-term rehabilitation. The extent of recovery varies greatly from person to person.
The Role of Rehabilitation Therapy
Rehabilitation is crucial for regaining lost skills and learning new ways to perform tasks. If mobility or speech is affected after the initial hospital stay, a doctor will likely recommend a rehabilitation program. If your condition does not improve after trying initial at-home exercises, booking a physical visit to a specialist with Apollo24|7 can help create a structured recovery plan.
Therapy often includes:
* Physical Therapy: To improve strength, balance, and coordination.
* Occupational Therapy: To relearn daily activities like dressing, eating, and bathing.
* Speech Therapy: To address problems with speaking, understanding, and swallowing.
Managing Emotional and Cognitive Changes
A stroke can lead to emotional challenges like depression, anxiety, and frustration. Cognitive changes, such as memory loss or difficulty with concentration, are also common. Support from mental health professionals, family, and support groups is an essential part of the healing process.
How to Prevent a Brain Attack: Controlling Your Risk Factors?
Up to 80% of strokes are preventable. Managing risk factors is the most powerful tool you have.
Manageable Health Conditions
Working with a doctor to manage the following conditions is critical:
* High Blood Pressure: The leading cause of stroke. Regular monitoring and medication are key.
* Atrial Fibrillation (AFib): An irregular heartbeat that can cause clots to form in the heart. Apollo24|7 offers convenient home collection for tests like INR (used to monitor blood thinners for AFib patients).
* High Cholesterol and Diabetes: These conditions contribute to artery-clogging plaque.
Lifestyle Choices for a Healthier Brain
* Eat a balanced diet rich in fruits, vegetables, and whole grains.
* Exercise regularly, aim for at least 150 minutes of moderate activity per week.
* Quit smoking and limit alcohol consumption.
* Maintain a healthy weight.
Conclusion
A brain attack is a formidable health event, but knowledge is your greatest defense. By recognising the sudden signs of a stroke—using the F.A.S.T. acronym as your guide and acting without hesitation, you can drastically improve outcomes. Remember, a transient ischemic attack (TIA) is not a minor event; it is a critical warning that demands immediate medical attention to prevent a more devastating stroke. The journey of recovery requires patience, support, and professional rehabilitation, but countless survivors go on to live fulfilling lives. Ultimately, the power of prevention should not be underestimated. By taking proactive steps to manage your blood pressure, stay active, and eat well, you are actively protecting your brain health for the future. Share this knowledge with your loved ones; it’s information that truly has the power to save a life.
Consult a Top Neurologist for Personalised Advice
Consult a Top Neurologist for Personalised Advice

Dr. Vemula Sreekanth
Neurologist
18 Years • MD(Med), DM(Neuro)
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad

Dr. Gopal Poduval
Neurologist
32 Years • MBBS, MD (Medicine), DNB (Medicine), DNB (Neurology)
Lucknow
Apollomedics Super Speciality Hospital, Lucknow
(250+ Patients)

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Deepak A N
Neurosurgeon
10 Years • MBBS, MS (General Surgery, M.Ch (Neurosurgery)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
(25+ Patients)
Consult a Top Neurologist for Personalised Advice

Dr. Vemula Sreekanth
Neurologist
18 Years • MD(Med), DM(Neuro)
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad

Dr. Gopal Poduval
Neurologist
32 Years • MBBS, MD (Medicine), DNB (Medicine), DNB (Neurology)
Lucknow
Apollomedics Super Speciality Hospital, Lucknow
(250+ Patients)

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Deepak A N
Neurosurgeon
10 Years • MBBS, MS (General Surgery, M.Ch (Neurosurgery)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru
(25+ Patients)
More articles from Brain Injury
Frequently Asked Questions
1. What is the difference between a stroke and a brain attack?
There is no difference. 'Brain attack' is a newer term used to emphasise the suddenness and urgency of a stroke, similar to a 'heart attack,' helping people understand that it requires immediate emergency care.
2. Can a young person have a stroke?
Yes. While the risk increases with age, strokes can occur at any age, including in children and young adults. Factors like congenital heart defects, clotting disorders, substance abuse, and untreated high blood pressure can contribute to stroke in young adults.
3. What are the long-term effects of a stroke?
The long-term effects of a brain attack depend on the stroke's severity and location. They can include paralysis or weakness on one side of the body, difficulty speaking (aphasia), memory loss, emotional changes, and chronic pain.
4. What is the difference between a stroke and an aneurysm?
Aneurysm is a weak, bulging spot on an artery wall. A stroke is an event where brain tissue is damaged. A ruptured brain aneurysm is one cause of a hemorrhagic stroke.
5. How can I prevent a second stroke?
Preventing a second stroke involves strict adherence to prescribed medications (e.g., blood thinners, statins), managing risk factors like hypertension and diabetes, attending all follow-up appointments, and committing to heart-healthy lifestyle changes. If symptoms persist or you have concerns about your prevention plan, consult a doctor online with Apollo24|7 for further evaluation.