Navigating the Landscape of Brain Damage: A Comprehensive Guide
Discover the causes, symptoms, types, and treatment options for brain damage in this comprehensive guide. Learn how early diagnosis and rehabilitation can improve outcomes.

Written by Dr. Vasanthasree Nair
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
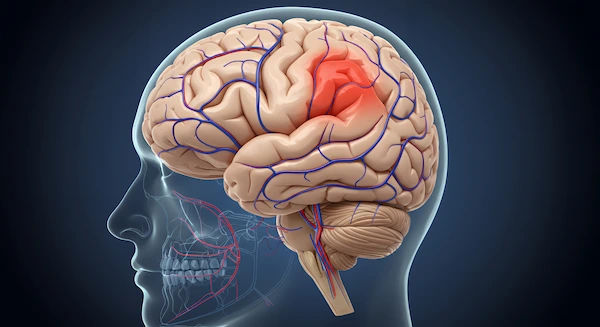
The human brain, the command centre for our entire being, is remarkably resilient yet profoundly vulnerable. An injury to this complex organ can feel like navigating an uncharted and frightening landscape, leaving individuals and their families searching for a map. The term "brain damage" encompasses a vast territory, from a mild concussion that resolves quickly to severe traumatic injuries that require lifelong adaptation. This guide aims to be your compass. We will demystify the types and causes of brain injuries, illuminate the path from diagnosis through rehabilitation, and provide practical advice for recovery and prevention.
What is Brain Damage? Understanding the Basics
Brain damage refers to any injury that causes the deterioration or destruction of brain cells. It's not a single condition but an umbrella term for a spectrum of injuries that can disrupt the brain's normal functioning. These disruptions can affect everything from motor skills and speech to memory, personality, and sensory processing. The impact is as unique as the individual, depending on the injury's location, severity, and cause. Broadly, brain injuries are categorised into two types: those caused by an external force and those that originate from within the body.
Consult a Neurologist for Personalised Advice
Traumatic Brain Injury (TBI): The External Assault
A Traumatic Brain Injury (TBI) occurs when an external mechanical force injures the brain. This can be a blow, jolt, or penetrating injury to the head. Common causes include falls, vehicle accidents, sports injuries, and violence. TBIs are graded on a scale of severity:
Mild TBI (Concussion): The most common form, often involving a brief change in mental status or consciousness. While often called "mild," the effects can be significant and should not be ignored.
Moderate TBI: Involves a longer period of unconsciousness and confusion, with clearer evidence of injury on imaging scans.
Severe TBI: Often involves an extended period of unconsciousness or amnesia and can lead to long-term physical, cognitive, and behavioural challenges. A diffused axonal injury, where tearing of nerve tissues occurs throughout the brain, is a common type of severe TBI.
Acquired Brain Injury (ABI): Internal Causes
An Acquired Brain Injury (ABI) is any injury to the brain that occurs after birth and is not hereditary, congenital, or degenerative. The key difference from TBI is the lack of external trauma. Instead, the damage comes from internal medical events.
Major causes include:
Stroke: When blood supply to part of the brain is interrupted (ischemic) or when a blood vessel leaks or ruptures (hemorrhagic).
Anoxic/Hypoxic Injury: Damage caused when the brain is completely deprived of oxygen (anoxic) or receives insufficient oxygen (hypoxic), often during cardiac arrest or drowning.
Infections: illnesses like meningitis or encephalitis can cause swelling and damage to brain tissue.
Tumours: Both cancerous and non-cancerous tumours can destroy healthy brain cells and increase intracranial pressure.
Toxic Exposure: Inhaling or ingesting harmful substances like carbon monoxide or heavy metals can lead to neurological damage.
Recognising the Signs: Symptoms of Brain Injury
Symptoms can appear immediately or days after the incident. They are often grouped into physical, sensory, cognitive, and behavioural categories. Recognising these signs is crucial for seeking timely medical help.
Physical and Sensory Symptoms
These are often the most immediately noticeable signs. They include:
Persistent headaches or migraines
Nausea or vomiting
Convulsions or seizures
Dizziness, loss of balance, or coordination problems
Sensitivity to light or sound
Blurred vision or ringing in the ears (tinnitus)
Loss of smell or taste
Fatigue and drowsiness
Cognitive and Behavioural Changes
These symptoms can be more subtle but are equally disruptive to daily life. They may involve:
Memory problems, especially with new information
Difficulty concentrating or paying attention
Slowed thinking speed ("brain fog")
Mood swings, irritability, or increased anxiety
Depression and feelings of sadness
Changes in sleep patterns (sleeping too much or too little)
Impulsivity or lack of inhibition
If you or a loved one experiences any of these symptoms following a head injury or medical event, it is critical to consult a doctor. For immediate evaluation, you can consult a neurologist online with Apollo24|7 to discuss your symptoms and determine the next steps.
The Diagnostic Journey: How Brain Damage is Identified
A swift and accurate diagnosis is the cornerstone of effective treatment. The process typically begins with a neurological exam to check vision, hearing, balance, coordination, and reflexes. Doctors use advanced tools to look inside the brain and assess its function.
Imaging Techniques: CT Scans and MRIs
Computerised Tomography (CT) Scan: This is usually the first imaging test performed in an emergency room. It uses a series of X-rays to create a detailed cross-sectional image of the brain. It's excellent for quickly revealing bleeding, swelling, and skull fractures.
Magnetic Resonance Imaging (MRI): An MRI uses powerful radio waves and magnets to create a highly detailed view of brain tissue. It's more sensitive than a CT scan for detecting more subtle injuries, including diffused axonal injury, and is often used once the patient is stable.
Neurological Assessments and Cognitive Testing
Beyond imaging, doctors use specialised assessments to gauge the functional impact of the injury. The Glasgow Coma Scale is a standard tool used to assess the level of consciousness after a TBI. For cognitive and behavioural symptoms, neuropsychologists conduct detailed testing to evaluate memory, problem-solving skills, attention, and emotional state. This helps create a tailored brain injury rehabilitation plan.
The Road to Recovery: Treatment and Rehabilitation Strategies
Treatment is a two-phase process: acute medical care to stabilise the patient and prevent further damage, followed by long-term rehabilitation to restore function and promote independence.
Immediate Medical Interventions
In the immediate aftermath of a severe injury, the primary goal is to ensure the brain receives enough oxygen and blood flow.
This may involve:
Surgery to remove hematomas (clotted blood), repair skull fractures, or relieve intracranial pressure.
Medications to prevent seizures, control blood pressure, or reduce inflammation.
Inducing a medically-induced coma in some severe cases to allow the brain to rest and swell without further damage.
The Crucial Role of Long-Term Rehabilitation
Rehabilitation is where the most significant gains in recovery are made. It leverages the brain's neuroplasticity, its ability to reorganise and form new neural connections. A multidisciplinary team guides this process.
Physical and Occupational Therapy
Physical Therapy: Focuses on rebuilding physical strength, coordination, balance, and mobility. Therapists work on walking, transferring from bed to chair, and improving gross motor skills.
Occupational Therapy: Helps patients relearn how to perform activities of daily living (ADLs) independently, such as dressing, eating, and grooming. They also work on fine motor skills and may recommend adaptive equipment.
Speech-Language and Cognitive Therapy
Speech-Language Therapy: Addresses problems with communication, including speaking, understanding language, reading, and writing. It also often involves therapy for swallowing difficulties (dysphagia).
Cognitive Therapy: Conducted by neuropsychologists or occupational therapists, this therapy uses exercises and strategies to improve memory, attention, concentration, executive functioning, and problem-solving skills.
Recovery is a marathon, not a sprint. Apollo24|7 offers connections to a network of specialists, including rehabilitation experts, who can help build a continuous and personalised recovery plan from the comfort of your home.
Living with Brain Injury: Long-Term Management and Support
The effects of a brain injury can be long-lasting, requiring ongoing management and adaptation. This journey is not just for the survivor but for their entire family and support network.
Adapting Your Home and Lifestyle
Creating a safe and supportive environment is key. This can include:
Establishing consistent routines to reduce cognitive fatigue.
Using memory aids like calendars, lists, and smartphone reminders.
Reducing clutter and distractions in the home.
Ensuring the home is well-lit and free of fall hazards.
The Importance of Mental Health and Emotional Support
The emotional toll of a brain injury is immense. Survivors may grieve their lost abilities, while caregivers experience significant stress. Seeking support is not a sign of weakness but of strength. This can include:
Individual or family therapy with a psychologist familiar with brain injury.
Joining support groups to connect with others who understand the journey.
Practising mindfulness, meditation, or other stress-reduction techniques.
Prevention: Safeguarding Your Brain Health
While not all brain injuries are preventable, many are. Key strategies include:
Always wear a seatbelt in a vehicle and ensure children are in age-appropriate car seats.
Wearing a helmet during sports like cycling, skating, skiing, and horseback riding, and for activities like riding a motorcycle.
Preventing falls by removing tripping hazards in the home, using non-slip mats, and installing handrails on stairways.
Managing underlying health conditions like hypertension and diabetes to reduce stroke risk.
Avoiding excessive alcohol and never using illicit drugs.
Conclusion
Navigating the landscape of brain damage is undoubtedly challenging, but it is a path you do not have to walk alone. Armed with knowledge, a dedicated medical team, and a strong support system, recovery and a high quality of life are achievable goals. Understanding the types, symptoms, and treatment options empowers you to advocate for yourself or your loved one effectively. If you suspect a brain injury, prioritise seeking professional medical guidance immediately.
Consult a Neurologist for Personalised Advice
Consult a Neurologist for Personalised Advice

Dr. Dipti Ranjan Tripathy
Neurologist
15 Years • MBBS, MD (GENERAL MEDICINE ),DM (NEUROLOGY)
Rourkela
Apollo Hospitals, Rourkela, Rourkela
(25+ Patients)

Dr. H Rahul
Neurologist
10 Years • MBBS, MD(Gen. Med.), DM(Neuro)
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad
(100+ Patients)

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Nipun Puranik
Neurologist
8 Years • MBBS MD, DM
Indore
Apollo Hospitals Vijay Nagar, Indore

Dr. Sandeep Gurram
Neurologist
12 Years • MBBS, MD(Internal Medicine), DM(Neurology), PDF(Movement disorders) - NIMHANS
Secunderabad
Apollo Hospitals Secunderabad, Secunderabad
More articles from Brain Injury
Frequently Asked Questions
1. Can the brain heal itself after damage?
Yes, to an extent. The brain has a natural ability to heal and rewire itself, known as neuroplasticity. Through rehabilitation and targeted therapy, healthy parts of the brain can sometimes learn to take over functions lost to injury, especially in younger individuals.
2. What is the difference between a concussion and brain damage?
A concussion is a type of brain damage—specifically, a mild traumatic brain injury (TBI). The term 'brain damage' is broader and includes all severities of TBI as well as non-traumatic acquired brain injuries like stroke.
3. How long does it take to recover from a traumatic brain injury?
Recovery time varies dramatically. Some people with a mild concussion recover in weeks, while others with moderate to severe TBI may see improvement for years. The most rapid recovery typically occurs in the first six months to two years, but progress can continue much longer.
4. Are headaches normal years after a brain injury?
Yes, persistent headaches, often resembling migraines or tension headaches, are a common long-term effect of a brain injury. If headaches persist or worsen, it is important to consult a neurologist for management strategies.
5. Can a previous brain injury make you more susceptible to future ones?
Yes. Sustaining a brain injury can make the brain more vulnerable to future injuries. This is known as second impact syndrome, where a second injury before the first has fully healed can lead to rapid and severe swelling, with potentially catastrophic consequences.