Guide to Breast Self Examination Guide
Learn how to perform a breast self-exam (BSE) at home with this step-by-step guide. Understand what to look for, how to feel for changes, and when to consult a doctor. Early detection saves lives.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. Vasanthasree Nair MBBS
Last updated on 13th Jan, 2026

Your Essential Guide to Breast Self-Examination: Know What's Normal for You
Breast health is a vital part of overall wellness, and being proactive is your greatest asset. While regular clinical check-ups and mammograms are the gold standard for screening, breast self-examination (BSE) is a powerful, free, and accessible tool that puts you in control. This guide isn't about promoting fear; it's about fostering familiarity. By performing a simple breast examination monthly, you learn the unique landscape of your own body—what's normal for you. This knowledge is powerful because it allows you to detect subtle changes early, when they are most treatable. This comprehensive guide will walk you through the why, when, and how of BSE, equipping you with the confidence to make it a regular part of your health routine. Let's demystify the process and empower you with knowledge.
Why Breast Self-Examination is a Key Part of Your Health Routine?
The Power of Early Detection
The core benefit of a monthly breast self-exam is early detection. According to the American Cancer Society, when breast cancer is detected early and is still localized, the 5-year relative survival rate is 99%. While BSE alone is not a definitive diagnostic tool, it is often the first step that leads a woman to seek medical attention. It’s your first line of defense, a regular check-in with your body that can identify potential issues long before they might become apparent otherwise.
It's About Knowing Your Baseline
Many women avoid self-exams out of anxiety—they're afraid of finding something. This guide reframes that thinking. The goal isn't to go on a "lump hunt" every month. Instead, it's to practice knowing your normal. Your breasts naturally have lumps, bumps, and ridges (especially if you have fibrocystic breast tissue). By examining them regularly, you learn what these normal features feel like. This makes it infinitely easier to recognize when something new, different, or unusual appears. You become the expert on your own body.
When and How Often Should You Perform a Self-Exam?
Timing is Everything: The Menstrual Cycle Connection
For menstruating women, timing is crucial. Your hormonal fluctuations can cause natural changes in your breasts, such as tenderness, swelling, and lumpiness. The best time to perform a breast self-exam is about 3 to 5 days after your period ends. At this point, hormonal activity has settled, and your breasts are least likely to be swollen or tender. This provides the most accurate baseline feel. If you no longer have periods, simply pick the same day every month—like the first day of the month—to make it easy to remember.
For Post-Menopausal Women and Men
Post-menopausal women and men should also be aware of their breast health. While the risk is different, breast cancer can still occur. Establishing a monthly routine on a fixed, easy-to-remember date is the best practice. Consistency is key, regardless of age or gender.
Step 1: The Visual Inspection in Front of a Mirror
Arm Positions for a Thorough Visual Check
Stand topless in front of a mirror with your shoulders straight and your arms on your hips. Observe your breasts in this relaxed position. Then, raise your arms high above your head and look for the same changes. Finally, place your palms on your hips and press firmly to flex your chest muscles.
What to Look For: Visual Changes
Look for any of the following changes in both breasts:
Dimpling, puckering, or bulging of the skin.
Changes in size, shape, or symmetry (it's common for one breast to be slightly larger, but look for new changes).
Nipple changes: Is one nipple inverted (turned inward) when it normally isn't? Is there redness, soreness, a rash, or swelling?
Discharge from the nipple (watery, milky, yellow, or blood).
Health Topic Carousel:
Doctor Speciality: General Physician
Text: Consult Top Specialists
Step 2: The Physical Examination – How to Feel for Changes
Choosing Your Technique: The Pattern Method
Use a firm, smooth touch with the pad of your middle three fingers. You can use one of three patterns to ensure you cover the entire breast, from your collarbone to the top of your abdomen, and from your armpit to your cleavage.
The Vertical Strip Pattern
This method, recommended by Johns Hopkins Medicine, is highly systematic. Imagine your breast divided into vertical strips. Use small, dime-sized circular motions and examine each strip from top to bottom, moving from the underarm to the breastbone.
The Circular Pattern
Move your fingers in ever-smaller concentric circles, starting from the outside of the breast and working your way toward the nipple.
The Wedge Pattern
Imagine your breast as a clock. Start at the outermost top of your breast (12 o'clock) and move inward toward the nipple in a straight line. Then move back to the outside at 1 o'clock and repeat, like slicing wedges of a pie.
The Right Touch: Using Your Fingerpads
Use three different pressure levels for each spot:
1. Light pressure to feel the tissue closest to the skin.
2. Medium pressure to feel a little deeper.
3. Firm pressure to feel the tissue closest to the chest and ribs.
Best Positions for a Physical Exam
Lying Down
Lie down on your back. This position flattens the breast evenly against your chest wall, making it easier to feel all the tissue thoroughly. Place a pillow under the shoulder of the breast you are examining.
In the Shower
Your fingers will glide more easily over soapy, wet skin, which can sometimes make it easier to feel subtle changes. The technique remains the same.
What Are You Actually Feeling For? Recognizing Warning Signs
H3: Common Benign (Non-Cancerous) Lumps
Most lumps are not cancerous. You might feel:
Fibroadenomas: Smooth, firm, rubbery lumps that move easily (common in young women).
Cysts: Soft, fluid-filled sacs that can feel tender, especially around your period.
General lumpiness: A ropy, ridge-like texture is common and normal.
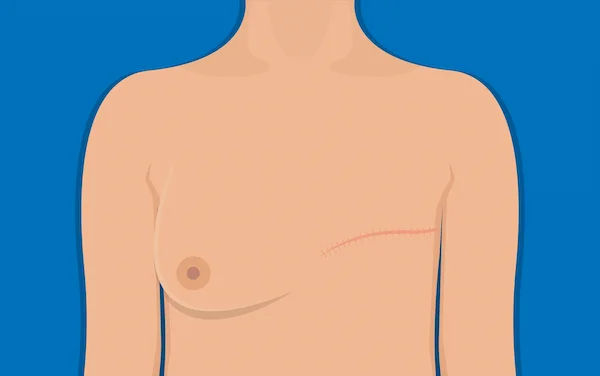
Potential Signs of Breast Cancer
Be aware of any new or changing lump. While only a doctor can diagnose, features that warrant a professional check include:
A hard, immovable lump with irregular edges.
Thickening or swelling that doesn't go away after your period.
Nipple discharge (especially if it's bloody or clear and comes from only one nipple).
Any persistent change in the skin (dimpling, redness, scaliness) or a newly inverted nipple.
What to Do (And Not to Do) If You Find a Lump?
First, don't panic. Remember, most lumps are not cancerous. Do not ignore it, but also do not assume the worst. The next step is to consult a healthcare professional for a clinical evaluation. If you notice a persistent change or lump, consult a doctor online with Apollo24|7 for a preliminary discussion and to book a physical visit for further evaluation. They can perform a clinical exam and, if needed, order imaging tests like an ultrasound or mammogram to get a clear picture.
The Limits of Self-Exams: Mammograms and Clinical Exams
It is critical to understand that breast self-examination is a supplementary screening tool. It does not replace mammograms or clinical breast exams performed by a doctor. A mammogram can detect microcalcifications and tiny tumors long before they can be felt by hand. Follow the recommended screening guidelines for your age and risk level. Think of BSE, clinical exams, and mammograms as a powerful trio working together to protect your health.
Quick Takeaways: Your BSE Cheat Sheet
Goal: Know what's normal for you, not to find cancer.
Frequency: Once a month.
Best Time: 3-5 days after your period ends.
Method: Use a systematic pattern (strip, circle, wedge) with three pressure levels.
Positions: Perform both a visual check (mirror) and a physical check (lying down/shower).
Action: Note any new, hard, immovable lumps or persistent visual changes.
Next Step: Always report any concerning changes to a doctor for a professional evaluation.
Conclusion: Empowerment Through Awareness
Making breast self-examination a regular monthly habit is one of the simplest yet most impactful actions you can take for your long-term health. It transforms you from a passive recipient of healthcare into an active, informed participant. This guide provides the roadmap, but the journey is yours. By committing just a few minutes each month, you build a deep familiarity with your body that is irreplaceable. This awareness brings peace of mind and, if ever needed, a significant head start on addressing any issues. Remember, you are your own best advocate. If you ever have questions about what you're feeling or want to discuss your breast cancer risk factors, don't hesitate to seek professional guidance. Your health is worth it.
FAQs
1. At what age should I start doing breast self-exams?
It's generally recommended that women begin practicing breast self-awareness in their early 20s. The goal is to establish a baseline of what's normal for you early on.
2. What if I have breast implants? Can I still perform a self-exam?
Yes, you can and should. You will need to learn the feel of the implant's edge and the breast tissue around it. Your surgeon can help guide you on the best technique to examine your specific anatomy.
3. I feel lumpy breasts all over. Is that normal?
Yes, this is very common and is often described as fibrocystic breast tissue. It's typically not a cause for concern. The key is to learn your specific pattern of lumpiness so you can detect any new or different lump that stands out.
4. How do I distinguish between a concerning lump and normal breast tissue?
Normal breast tissue often feels ropy or granular, especially in the upper outer quadrants. A potentially concerning lump often feels distinctly different from the rest of your breast tissue—it may be harder, immovable, have irregular edges, and not change with your menstrual cycle.
5. Is nipple discharge always a bad sign?
No. Nipple discharge can be caused by medications, hormonal imbalances, or stimulation. However, spontaneous discharge (without squeezing) that is clear or bloody, and that comes from only one nipple, should always be evaluated by a doctor.
Health Topic Carousel:
Doctor Speciality: General Physician
Text: Consult Top Specialists

_1.webp)