Your Complete Guide to Chronic Kidney Disease: Stages, Symptoms, and Hope
Discover a complete guide to chronic kidney disease, including its stages, symptoms, risk factors, and treatment options. Learn how early detection and proper management can help maintain kidney health and improve quality of life.

Written by Dr. Siri Nallapu
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Chronic Kidney Disease (CKD) is a condition that affects millions worldwide, yet it often progresses silently, without any obvious symptoms until significant damage has occurred. Think of your kidneys as your body's sophisticated filtration system, working tirelessly to remove waste, balance fluids, and manage electrolytes. When this system is compromised over a long period, it leads to CKD. This guide is designed to demystify this condition, walking you through everything from the early warning signs and five stages of progression to actionable management strategies and reasons for hope. Whether you're newly diagnosed, supporting a loved one, or proactively managing your health, understanding CKD is the first powerful step toward taking control of your kidney health and overall well-being.
What is Chronic Kidney Disease (CKD)?
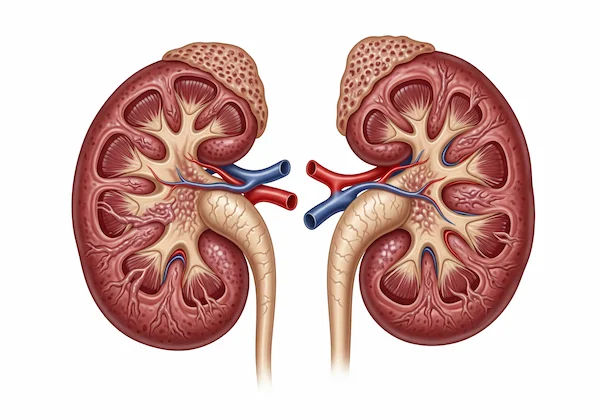
Chronic Kidney Disease, often abbreviated as CKD, is a progressive condition characterised by the gradual loss of kidney function over months or years. Unlike an acute injury that happens suddenly, CKD is a long-term journey. The kidneys' primary job is to filter excess water and waste from the blood to create urine. When they are damaged, they can't perform this vital task effectively, leading to a dangerous buildup of fluids and toxins in the body.
The Vital Role of Your Kidneys
Your two kidneys, each about the size of a fist, are powerhouses of function. They do far more than just produce urine. They are responsible for:
Filtering Waste: Removing toxins and waste products from the bloodstream.
Balancing Fluids: Regulating the body's water and salt levels to maintain healthy blood pressure.
Regulating Minerals: Managing key electrolytes like sodium, potassium, and phosphorus, which are critical for nerve and muscle function.
Producing Hormones: Creating hormones that help make red blood cells (preventing anaemia) and promote strong bones.
How CKD Differs from Acute Kidney Injury?
It's crucial to distinguish CKD from Acute Kidney Injury (AKI). AKI is a sudden episode of kidney failure or damage that happens within a few hours or days. It is often reversible if treated promptly. CKD, on the other hand, is a slow, irreversible decline in function. While its progression can often be slowed significantly, the damage that has occurred is usually permanent.
The Five Stages of Chronic Kidney Disease
CKD is classified into five stages based on how well the kidneys are filtering blood, a measure known as the glomerular filtration rate (GFR). This staging helps doctors create an appropriate treatment plan.
Understanding Your Glomerular Filtration Rate (GFR)
Your GFR is the best measure of your overall kidney function. It's calculated using a simple blood test that checks your creatinine levels (a waste product), along with your age, sex, and body size. A normal GFR is 90 or above. As your GFR number decreases, your kidney function is declining.
From Stage 1 (Mild) to Stage 5 (Kidney Failure)
Stage 1: Kidney damage with normal or high GFR (90+). Often, there are no symptoms, but protein might be detected in the urine.
Stage 2: Mild loss of kidney function (GFR 60-89). Symptoms are still rare.
Stage 3: Moderate loss of kidney function. This is split into:
* 3a: GFR 45-59
* 3b: GFR 30-44
Symptoms like swelling and fatigue may begin to appear.
Stage 4: Severe loss of kidney function (GFR 15-29). Planning for treatments like dialysis or transplant often begins here.
Stage 5: Kidney failure (GFR <15). The kidneys have lost nearly all ability to function. This is also called End-Stage Renal Disease (ESRD), requiring dialysis or a transplant to survive.
Symptoms of CKD
One of the biggest challenges with chronic kidney disease is its stealthy nature. In the early stages, the symptoms are either non-existent or so vague that they are easily mistaken for other common ailments.
The "Silent" Early Stages
Stages 1 and 2 typically present no obvious signs. The only way to detect CKD at this point is through specific blood and urine tests. This is why screening is so critical for individuals with risk factors like diabetes or hypertension.
Later-Stage Symptoms You Shouldn't Ignore
As kidney function declines to stage 3 and beyond, symptoms become more pronounced due to the buildup of waste and fluid in the body:
Fatigue and Trouble Concentrating: Caused by anaemia, a shortage of red blood cells.
Swelling (Oedema): Particularly in the ankles, feet, hands, or around the eyes due to fluid retention.
Changes in Urination: Foamy urine (indicating protein), urinating more or less frequently, or blood in the urine.
Persistent Itching: Caused by a buildup of minerals and nutrients in the blood.
Shortness of Breath: From fluid buildup in the lungs or anaemia.
Nausea and Vomiting: A result of uremia, the buildup of waste products.
If you experience a combination of these symptoms of kidney failure, it is essential to consult a doctor for a proper evaluation. If these symptoms persist, consult a doctor online with Apollo24|7 for further evaluation.
What Causes Chronic Kidney Disease?
CKD doesn't typically happen without an underlying cause. Understanding the root of the problem is key to managing the disease.
The Two Leading Causes: Diabetes and High Blood Pressure
These two conditions are responsible for about two-thirds of all CKD cases.
Diabetes (Diabetic Nephropathy): High blood sugar levels over time damage the millions of tiny filtering units (nephrons) in the kidneys.
High Blood Pressure (Hypertensive Nephrosclerosis): Uncontrolled hypertension can damage the blood vessels in the kidneys, impairing their ability to filter blood effectively.
Other Contributing Factors and Conditions
Glomerulonephritis (inflammation of the kidney's filtering units)
Polycystic Kidney Disease (an inherited genetic disorder)
Prolonged obstruction of the urinary tract (e.g., from enlarged prostate or kidney stones)
Recurrent kidney infections
Autoimmune diseases like Lupus
Consult Top Specialists
How is CKD Diagnosed?
Early diagnosis is paramount for slowing the progression of CKD. It typically involves a combination of tests that your primary care physician can order.
Key Blood Tests: Serum Creatinine and eGFR
The serum creatinine test measures the level of creatinine, a waste product, in your blood. If your kidneys aren't working well, creatinine levels will rise. This value is then used to calculate your estimated Glomerular Filtration Rate (eGFR), which is the key indicator of your kidney function stage.
The Importance of Urine Albumin Tests
A urine test checks for the presence of albumin, a type of protein. Healthy kidneys don't allow significant amounts of protein to pass into the urine. The presence of albumin (albuminuria) is an early sign of kidney damage, often appearing before a significant drop in GFR. Apollo24|7 offers convenient home collection for tests like serum creatinine and urine albumin, making monitoring easier.
Imaging and Other Diagnostics
Sometimes, an ultrasound or CT scan is used to get a picture of the kidneys to check for abnormalities in size, shape, or obstructions. In rare cases, a kidney biopsy may be needed to determine the exact cause of the damage.
Treatment and Managing Your CKD
While CKD is often irreversible, its progression can be dramatically slowed with proper treatment and lifestyle management. The goals are to treat the underlying cause, manage symptoms, and prevent complications.
Medications to Protect Kidney Function
ACE Inhibitors or ARBs: These blood pressure medications are often prescribed even to those without hypertension because they help reduce protein in the urine and protect kidney function.
SGLT2 Inhibitors: A newer class of diabetes medication that has shown significant benefits in slowing CKD progression.
Diuretics: Help the body eliminate excess fluid, reducing swelling and controlling blood pressure.
Medications for Complications: Such as drugs to control phosphorus levels, treat anaemia, or support bone health.
The Renal Diet: Navigating Sodium, Potassium, and Phosphorus
Dietary changes are a cornerstone of managing your CKD. A kidney-friendly diet often involves:
Limiting Sodium: To control blood pressure and fluid retention.
Monitoring Potassium: High levels can be dangerous for heart rhythm.
Reducing Phosphorus: To prevent bone and heart disease.
Moderating Protein Intake: Reducing the kidneys' workload. Working with a renal dietitian is highly recommended to create a personalised plan.
Lifestyle Changes for Kidney Health
Blood Pressure Control: Keeping it below 140/90 mm Hg (or a target set by your doctor).
Blood Sugar Management: For diabetics, maintaining a target HbA1c level is critical.
Regular Exercise: Helps control weight, blood pressure, and blood sugar.
Avoiding NSAIDs: Over-the-counter pain relievers like ibuprofen can harm kidneys.
Complications Associated with Advanced CKD
If left unmanaged, CKD can lead to serious health problems, including:
Cardiovascular Disease: CKD significantly increases the risk of heart attack and stroke.
Anaemia: A shortage of red blood cells, leading to severe fatigue.
Weak Bones: Kidney disease disrupts the calcium and phosphorus balance, leading to bone weakness.
Electrolyte Imbalance: Sudden, dangerous spikes in potassium can affect heart function.
Prevention: Can You Reduce Your Risk?
While not all causes are preventable, you can significantly reduce your risk by:
Managing diabetes and high blood pressure meticulously.
Maintaining a healthy weight.
Staying hydrated with water.
Not smoking.
Using over-the-counter pain medications only as directed.
Getting regular check-ups that include kidney function tests if you have risk factors.
Living a Full Life with Chronic Kidney Disease
A CKD diagnosis is life-changing, but it is not a life sentence. With modern medicine, diligent management, and a strong support system, many people live full, active lives for decades after their diagnosis. Adherence to treatment plans, open communication with your healthcare team, and a positive mindset are your greatest tools.
Conclusion
Understanding chronic kidney disease empowers you to become an active participant in your health journey. From recognising the subtle early signs to comprehending the five stages and embracing necessary lifestyle adjustments, knowledge is your first line of defence. Remember, a diagnosis is not an endpoint but a starting point for proactive management. By working closely with your healthcare providers, including the specialists available through platforms like Apollo24|7, you can create an effective care plan tailored to your needs. Whether it's controlling your blood pressure, modifying your diet, or simply staying informed, every positive step you take helps protect your kidney function and preserve your overall quality of life. Take that step today—talk to a doctor and get the answers you deserve.
Consult Top Specialists
Consult Top Specialists

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly

Dr Madhav Desai
Nephrologist
22 Years • MBBS, MD, DM (Nephrology)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Seerapani Gopaluni
Nephrologist
18 Years • MBBS, MRCP(UK), CCT(Oxford), PhD(Cambridge), FRCP(London)
Hyderabad
Apollo Hospitals Financial District, Hyderabad
Dr. Sunil Jawale
Nephrologist
17 Years • MBBS, MD (Internal Medicine), DM (Nephrology)
Pune
Apollo Hospitals Pune, Pune

Dr. Vamsee Priya Marina
Nephrologist
13 Years • MBBS, MD (Internal Medicine), MD (Nephrology), Diplomate American Board of Internal Medicine
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
(50+ Patients)
More articles from Chronic Kidney Disease Ckd
Frequently Asked Questions
1. Is chronic kidney disease curable?
2. What foods are good for kidneys?
Kidney-friendly foods generally include apples, berries, cauliflower, fish, olive oil, and skinless chicken. The best diet depends on your specific stage of CKD, so it's important to work with a doctor or dietitian to create a personalized renal diet plan.
3. Can you live a long life with stage 3 kidney disease?
Yes, many people live for decades with stage 3 CKD. Life expectancy depends heavily on factors like age, overall health, and, most importantly, how well you manage the condition through medication, diet, and controlling underlying causes.
4. What is the difference between kidney disease and kidney failure?
Kidney disease is a broad term for any condition that damages the kidneys. Kidney failure, also called End-Stage Renal Disease (ESRD), is the final stage (Stage 5) of chronic kidney disease, where the kidneys have lost nearly all their function and require dialysis or a transplant to sustain life.
5. How often should I get my kidneys checked?
If you have major risk factors like diabetes, high blood pressure, or a family history of kidney disease, you should have your kidney function checked with blood and urine tests at least once a year. If you have been diagnosed with CKD, your doctor will recommend more frequent monitoring.

.webp)
_0.webp)