Your Complete Guide to Managing High Phosphorus in Kidney Disease
Learn how to manage high phosphorus in kidney disease with diet, phosphate binders, dialysis support, and lifestyle strategies to protect your heart and bones.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. Vasanthasree Nair MBBS
Last updated on 13th Jan, 2026

Introduction
Living with chronic kidney disease (CKD) means becoming an expert in managing your body's chemistry. One of the most critical, yet often overlooked, balances to maintain is your phosphorus level. When your kidneys are damaged, they can't remove excess phosphorus from your blood effectively, leading to a condition called hyperphosphataemia. This isn't just a number on a lab report; it's a serious concern that can silently damage your heart, bones, and overall health. But here's the good news: with the right knowledge and tools, managing hyperphosphataemia in CKD is entirely within your control. This guide will walk you through everything you need to know—from understanding the risks to mastering your diet and working with your healthcare team—so you can feel empowered to protect your health every day.
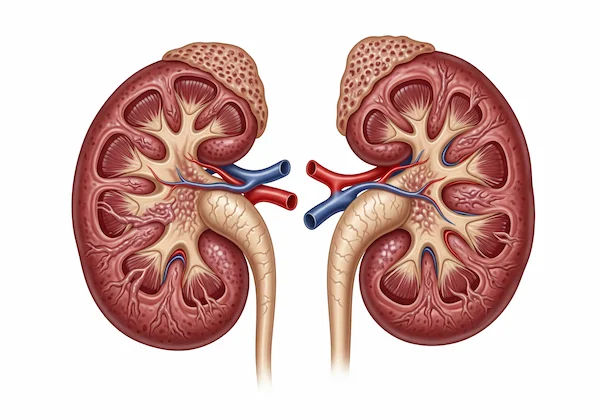
What Exactly is Hyperphosphataemia?
Hyperphosphataemia is the medical term for having abnormally high levels of phosphate in your blood. Phosphorus is a mineral found naturally in your bones and teeth and is essential for creating energy, building strong bones, and maintaining nerve and muscle function. We get it from the food we eat. Normally, healthy kidneys filter out excess phosphorus and remove it from the body through urine. However, as kidney function declines in CKD, this filtration system becomes less efficient. The phosphorus starts to build up in the bloodstream, leading to hyperphosphataemia. Think of it like a sink with a clogged drain; if water (phosphorus) keeps flowing in but can't drain out, the sink will eventually overflow.
The Crucial Kidney-Phosphorus Connection
Your kidneys and phosphorus have a tightly regulated relationship. They are designed to maintain a perfect balance. When kidney function drops below a certain point (typically around stage 3b-4 of CKD), they lose this ability. This is why monitoring your serum phosphate levels becomes a routine and vital part of your care plan. It’s not your fault; it’s a direct consequence of reduced kidney function.
Why High Phosphorus is a Silent Threat in CKD
The danger of hyperphosphataemia is that it often has no obvious symptoms in its early stages. You might feel perfectly fine, but inside, high phosphorus levels are triggering a chain reaction of damage, primarily to your cardiovascular system and skeletal structure.
The Domino Effect on Your Heart and Blood Vessels
This is the most serious risk. Excess phosphorus in the blood binds with calcium, forming hard deposits (calcification) in your blood vessels, heart valves, and heart muscles. This makes your blood vessels stiff and narrow, forcing your heart to work harder to pump blood. This significantly increases your risk of heart disease, heart attacks, and strokes. In fact, cardiovascular disease is the leading cause of death for people with CKD, and uncontrolled phosphorus is a major contributor.
Weakening Bones: Renal Osteodystrophy
Your bones and kidneys are also closely linked. High phosphorus levels disrupt the balance of calcium and vitamin D, which are essential for bone health. To correct this imbalance, your body produces too much parathyroid hormone (PTH), a condition called secondary hyperparathyroidism. This hormone leaches calcium from your bones to try and normalise blood calcium levels, leaving your bones weak, brittle, and prone to pain and fractures. This entire disorder is known as renal osteodystrophy.
Health topic carousel:
Doctor's speciality: Nephrology
Text: Consult an Nephrologist for the best advice
How Do You Know If Your Phosphorus is High? Recognising the Signs
As mentioned, early hyperphosphataemia is often asymptomatic. However, as levels become severely elevated, you might experience:
Bone and joint pain
Muscle cramps
Itchy skin
Red eyes or eye irritation
Numbness or a tingling sensation around the mouth
Because these signs can be vague or appear late, you should never wait for symptoms. Regular blood tests ordered by your nephrologist are the only reliable way to monitor your phosphorus levels. If you experience persistent itching or bone pain, it's crucial to consult a doctor online with Apollo24|7 for further evaluation and to get your levels checked. Apollo24|7 offers convenient home collection for tests like phosphorus and PTH, making monitoring easier.
The Cornerstone of Management: Your Diet
Dietary modification is your first and most powerful line of defence against high phosphorus levels. Adopting a low phosphorus diet for kidney disease is non-negotiable.
Phosphorus in Food: Organic vs. Inorganic - The Critical Difference
This is a key insight many guides miss. Not all dietary phosphorus is created equal.
Organic Phosphorus: This is naturally occurring in protein-rich foods like meat, poultry, fish, nuts, beans, and dairy. Your body only absorbs about 40-60% of this type.
Inorganic Phosphorus (Additives): This is the real culprit. Found in processed foods, fast food, canned items, sodas (especially colas), and packaged meats as additives (words containing "phos" like calcium phosphate, phosphoric acid), it is nearly 100% absorbed by your body. This makes it far more dangerous for someone with CKD.
Best Low-Phosphorus Food Choices
Focus on fresh, whole foods:
Fruits: Apples, berries, grapes, peaches, pears.
Vegetables: Cucumbers, carrots, lettuce, onions, peppers.
Grains: White bread, rice, and pasta (whole grains are healthier but higher in phosphorus, so portion control is key).
Protein: Fresh meat and poultry in moderate, appropriate portions.
High-Phosphorus Foods to Limit or Avoid
Dairy products (milk, cheese, yoghurt)
Nuts, seeds, and nut butters
Dried beans, lentils, and peas
Processed meats (sausage, hot dogs, lunch meat)
Cola soft drinks and bottled iced teas
Whole grain bread and bran cereals
Chocolate and beer
The Sneaky Danger of Phosphate Additives
Become a label detective. Always check ingredient lists on packaged foods for "phos" words. Avoiding processed foods is the single best way to eliminate these additives from your kidney-friendly diet plan.
Phosphate Binders: Your Dietary Ally
When diet alone isn't enough to control your levels, your doctor will prescribe phosphate binder medications.
How Phosphate Binder Medications Work
Binders are not absorbed into your bloodstream. Instead, they work like a sponge in your stomach and intestines. They bind to the phosphorus from the food you've just eaten, forming a compound that can't be absorbed. This compound is then passed out of your body through your stool, effectively removing the phosphorus before it ever enters your bloodstream.
Types of Binders and How to Take Them Correctly
There are several types (calcium-based, sevelamer, lanthanum, iron-based), each with pros and cons. The most critical rule is timing: you must take them with meals and snacks. Taking a binder without food is ineffective. If you have questions about phosphate binder side effects or timing, always speak with your doctor or pharmacist.
The Role of Dialysis in Phosphate Control
For patients on dialysis, the treatment helps remove some phosphorus from the blood. However, it's often not enough to remove all the phosphorus that builds up between sessions. Therefore, following a low phosphorus diet and taking phosphate binders correctly remains essential even for those on dialysis. It's a combined effort.
Building Your Action Plan: Daily Tips for Success
Partner with a Dietitian: A renal dietitian is your best resource for creating a personalised and enjoyable meal plan.
Cook at Home: This gives you full control over ingredients.
Read Every Label: Make it a habit to avoid "phos" additives.
Take Binders Faithfully: Keep them with you at all times so you're never caught without them at mealtime.
Attend All Appointments: Regular monitoring is key to staying on track.
Conclusion
Managing hyperphosphataemia in CKD might seem daunting at first, but it is one of the most impactful actions you can take to preserve your health and quality of life. By understanding the risks, embracing a whole-foods diet, diligently taking prescribed medications, and staying engaged with your healthcare team, you are actively protecting your heart and bones from harm. Remember, you are the most important member of your care team. Use the knowledge in this guide, ask questions, and advocate for your health. If your phosphorus levels remain high despite your best efforts, book a physical visit to a doctor or nephrologist with Apollo24|7 to reassess and adjust your management plan. You have the power to manage this condition and thrive.
Frequently Asked Questions (FAQs)
What is a safe phosphorus level for someone with CKD?
A general target is to keep your serum phosphorus level between 2.5 and 4.5 mg/dL. However, your doctor will set a personalised target range based on your specific stage of CKD and other health factors.
Can I ever cheat on my low-phosphorus diet?
An occasional, small treat might be okay, but it's crucial to discuss this with your dietitian. If you do have a higher-phosphorus meal, ensure you take your phosphate binders exactly as prescribed to help mitigate the impact.
Are there any natural phosphate binders?
Some studies have explored options like chitosan or certain clays, but they are not regulated or proven to be safe and effective for CKD patients. Always stick to the FDA-approved binders prescribed by your doctor, as their safety and efficacy are well-documented.
Does drinking more water lower phosphorus levels?
For individuals with very early CKD who still produce ample urine, hydration can help. However, for those with advanced CKD (stages 4-5) who retain fluid, increasing water intake is not recommended and can be dangerous. It can lead to fluid overload, swelling, and high blood pressure. Follow your doctor's specific fluid intake recommendations.
How often should I get my phosphorus levels checked?
The frequency depends on your stage of CKD and stability. It could range from every 3-6 months in stable early stages to every month or even more frequently if you are on dialysis or your levels are fluctuating. Your doctor will determine the appropriate schedule for you.
Health topic carousel:
Doctor's speciality: Nephrology
Text: Consult an Nephrologist for the best advice
Consult Top Nephrologists

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly

Dr Madhav Desai
Nephrologist
22 Years • MBBS, MD, DM (Nephrology)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Seerapani Gopaluni
Nephrologist
18 Years • MBBS, MRCP(UK), CCT(Oxford), PhD(Cambridge), FRCP(London)
Hyderabad
Apollo Hospitals Financial District, Hyderabad
Dr. Sunil Jawale
Nephrologist
17 Years • MBBS, MD (Internal Medicine), DM (Nephrology)
Pune
Apollo Hospitals Pune, Pune

Dr. Vamsee Priya Marina
Nephrologist
13 Years • MBBS, MD (Internal Medicine), MD (Nephrology), Diplomate American Board of Internal Medicine
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
(50+ Patients)
Consult Top Specialists

Dr. Manju Kamal
Nephrologist
12 Years • MBBS,MD(General Medicine), DNB,DM(Nephrology)
Angamaly
Apollo Hospitals Karukutty, Angamaly

Dr Madhav Desai
Nephrologist
22 Years • MBBS, MD, DM (Nephrology)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Seerapani Gopaluni
Nephrologist
18 Years • MBBS, MRCP(UK), CCT(Oxford), PhD(Cambridge), FRCP(London)
Hyderabad
Apollo Hospitals Financial District, Hyderabad
Dr. Sunil Jawale
Nephrologist
17 Years • MBBS, MD (Internal Medicine), DM (Nephrology)
Pune
Apollo Hospitals Pune, Pune

Dr. Vamsee Priya Marina
Nephrologist
13 Years • MBBS, MD (Internal Medicine), MD (Nephrology), Diplomate American Board of Internal Medicine
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda
(50+ Patients)
_0.webp)

.webp)